Ketogenic diets are put to the test for diabetes reversal.
As you can see at the start of my video Does a Ketogenic Diet Help Diabetes or Make It Worse?, ketogenic diets can lower blood sugars better than conventional diets. So much so, in fact, that there is a keto product company that claims ketogenic diets can “reverse” diabetes. However, they are confusing the symptom (high blood sugars) with the disease (carbohydrate intolerance). People with diabetes can’t properly handle carbohydrates, and this manifests as high blood sugars. Clearly, if you stick to eating mostly fat, your blood sugars will stay low, but you may be actually making the underlying disease worse at the same time.
We’ve known for nearly a century that if you put people on a ketogenic diet, their carbohydrate intolerance can skyrocket within just two days. Below and at 0:46 in my video, you can see a graph from the study showing the blood sugar response two days after eating sugar. On a high-carb diet, blood sugar response is about 90 mg/dL. But, the blood sugar response to the same amount of sugar after a high-fat diet is about 190 mg/dL, nearly double. The intolerance to carbohydrates skyrocketed on a high-fat diet.
After one week on an 80 percent fat diet, you can quintuple your blood sugar spike in reaction to the same carb load compared to a week on a low-fat diet, as you can see in the graph below and at 1:12 in my video. 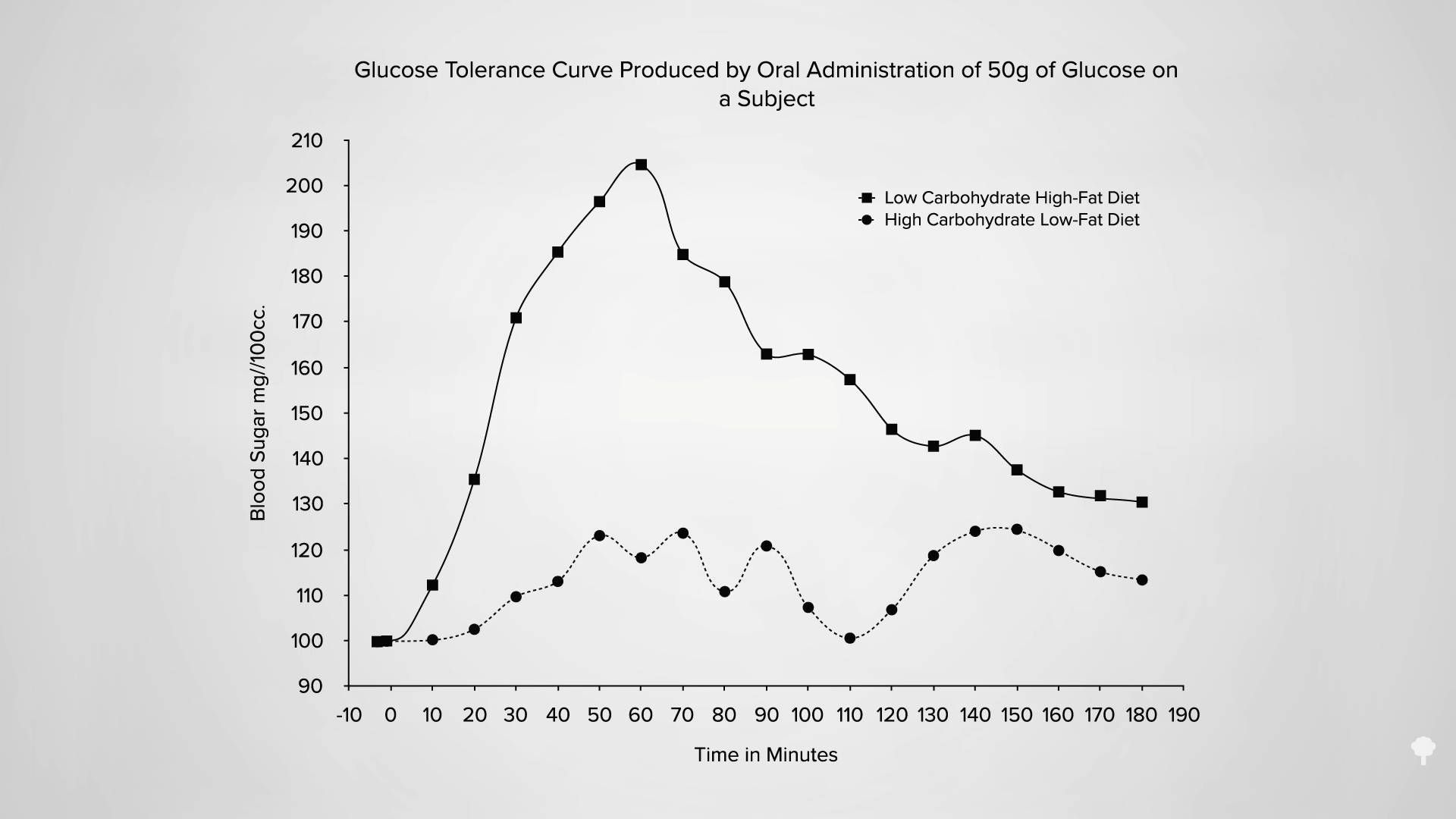
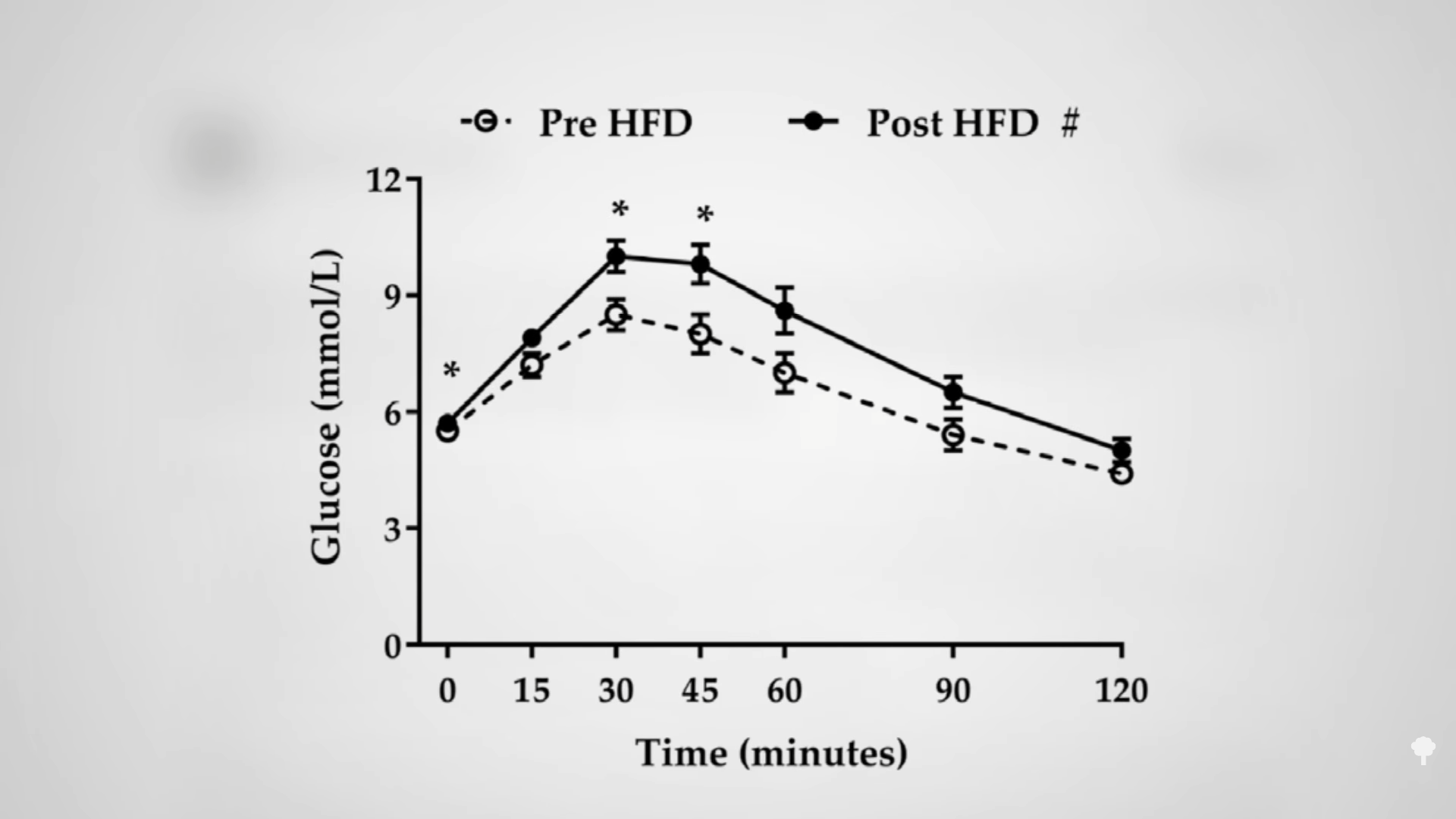
Even a single day of excessive dietary fat intake can do it, as you can see in the graph below and at 1:26 in my video. If you’re going in for a diabetes test, having a fatty dinner the night before can adversely affect your results. Just one meal high in saturated fat can make carbohydrate intolerance, the cause of diabetes, worse within four hours.
Given enough weight loss by any means, whether from cholera or bariatric surgery, type 2 diabetes can be reversed, but a keto diet for diabetes may not just be papering over the cracks, but actively throwing fuel on the fire.
I’ve been trying to think of a good metaphor. It’s easy to come up with things that just treat the symptoms without helping the underlying disease, like giving someone with pneumonia aspirin for their fever instead of antibiotics. However, a keto diet for diabetes is worse than that because it may treat the symptoms while actively worsening the disease. It may be more like curing the fever by throwing that pneumonia patient out into a snow bank or “curing” your amputated finger by amputating your hand. One of the co-founders of masteringdiabetes.org suggested it’s like a CEO who makes their bad bottom line look better by borrowing tons of cash. The outward numbers look better, but on the inside, the company is just digging itself into a bigger hole.
Do you remember The Club, that popular car anti-theft device that attaches to the steering wheel and locks it in place so the steering column can only turn a few inches? Imagine you’re in a car at the top of a hill with the steering wheel locked. Then, the car starts rolling down the hill. What do you do? Imagine there’s also something stuck under your brake pedal. The keto-diet equivalent response to this situation is who cares if you’re barreling down into traffic with a locked steering wheel and no brakes—just stick to really straight deserted roads without any stop signs or traffic lights. If you do that, problem solved! The longer you go, the more speed you’ll pick up. If you should hit a dietary bump in the road or start to veer off the path, the consequences could get more and more disastrous over time. However, if you stick to the keto straight and narrow, you’ll be a-okay! In contrast, the non-keto response would be to just unlock the steering wheel and dislodge whatever’s under your brake. In other words, fix the underlying problem instead of just whistling past—and then into—the graveyard.
The reason keto proponents claim they can “reverse” diabetes is they can successfully wean type 2 diabetics off their insulin. That’s like faith-healing someone out of the need for a wheelchair by making them stay in bed the rest of their life. No need for a wheelchair if you never move. Their carbohydrate intolerance isn’t gone. Their diabetes isn’t gone. In fact, it could be just as bad or even worse. Type 2 diabetes is reversed when you are weaned off insulin while eating a normal diet like everyone else. Then and only then do you not have diabetes anymore. A true diabetes reversal diet, as you can see below and at 4:58 in my video, is practically the opposite of a ketogenic diet: getting diabetics off their insulin within a matter of weeks by eating more than 300 grams of carbs a day! 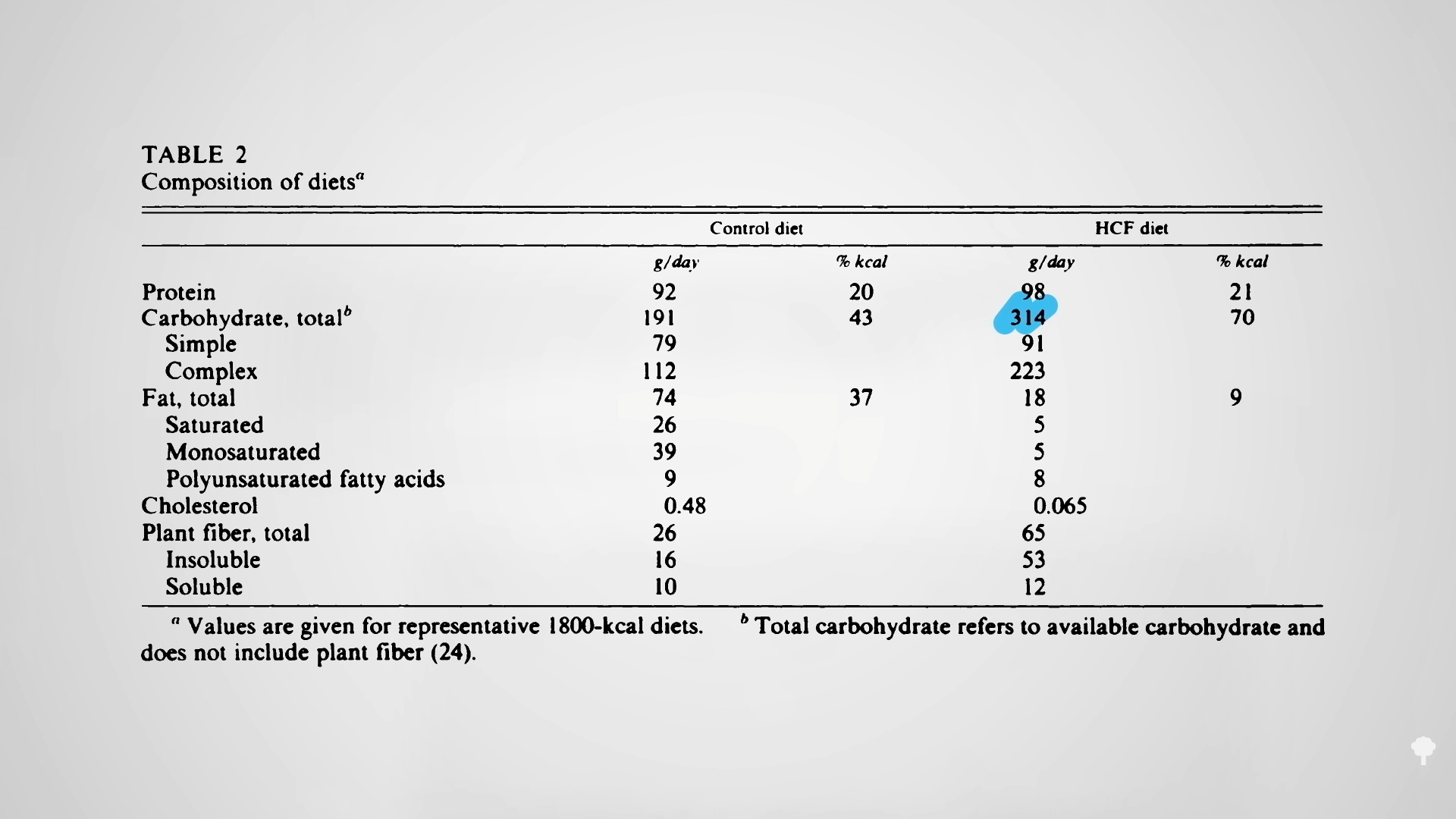 The irony doesn’t stop there. One of the reasons people with diabetes suffer such nerve and artery damage is due to an inflammatory metabolic toxin known as methylglyoxal, which forms at high blood sugar levels. Methylglyoxal is the most potent creator of advanced glycation end products (AGEs), which are implicated in degenerative diseases—from Alzheimer’s and cataracts to kidney disease and strokes, as you can see below and at 5:31 in my video.
The irony doesn’t stop there. One of the reasons people with diabetes suffer such nerve and artery damage is due to an inflammatory metabolic toxin known as methylglyoxal, which forms at high blood sugar levels. Methylglyoxal is the most potent creator of advanced glycation end products (AGEs), which are implicated in degenerative diseases—from Alzheimer’s and cataracts to kidney disease and strokes, as you can see below and at 5:31 in my video.
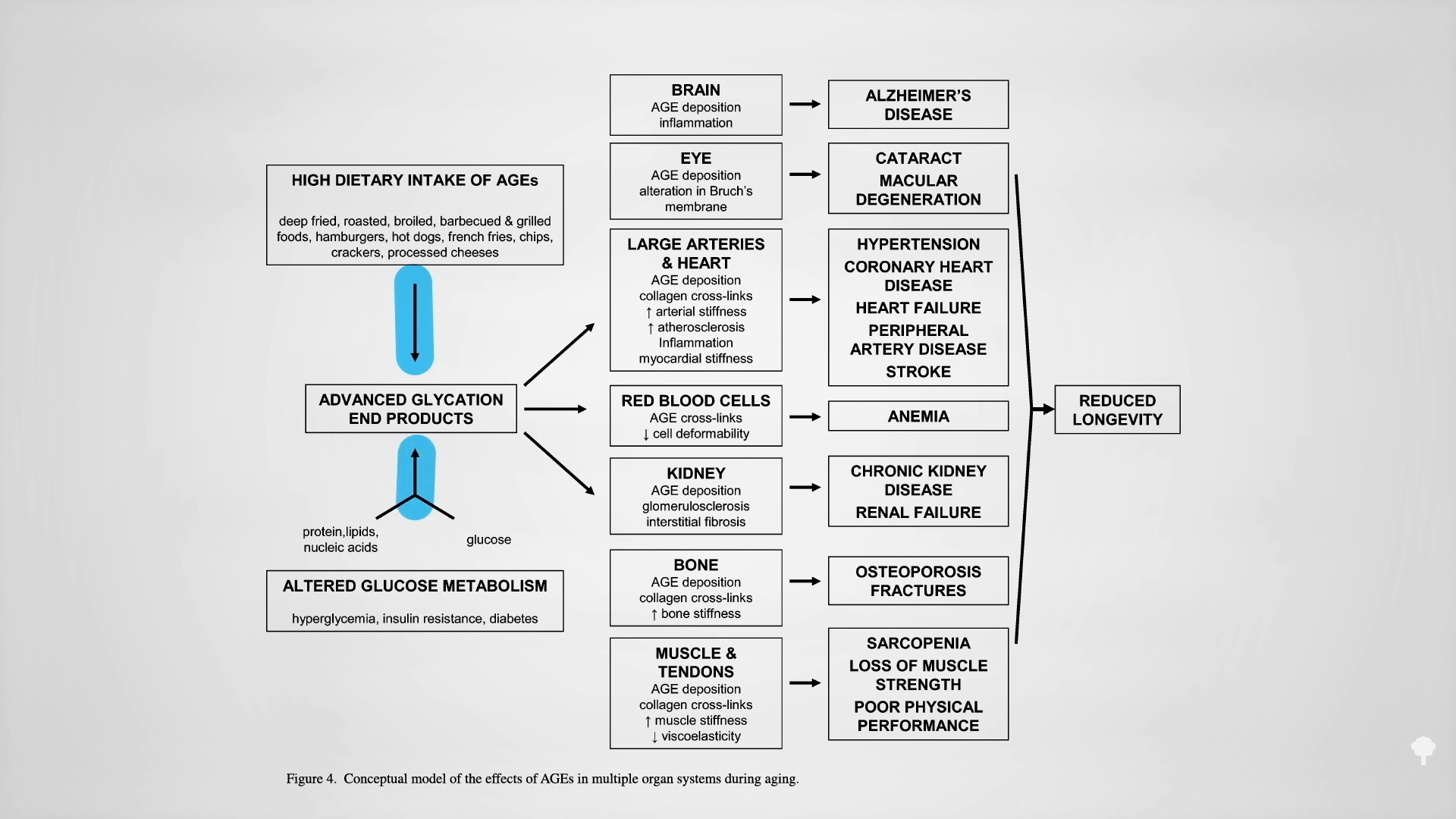
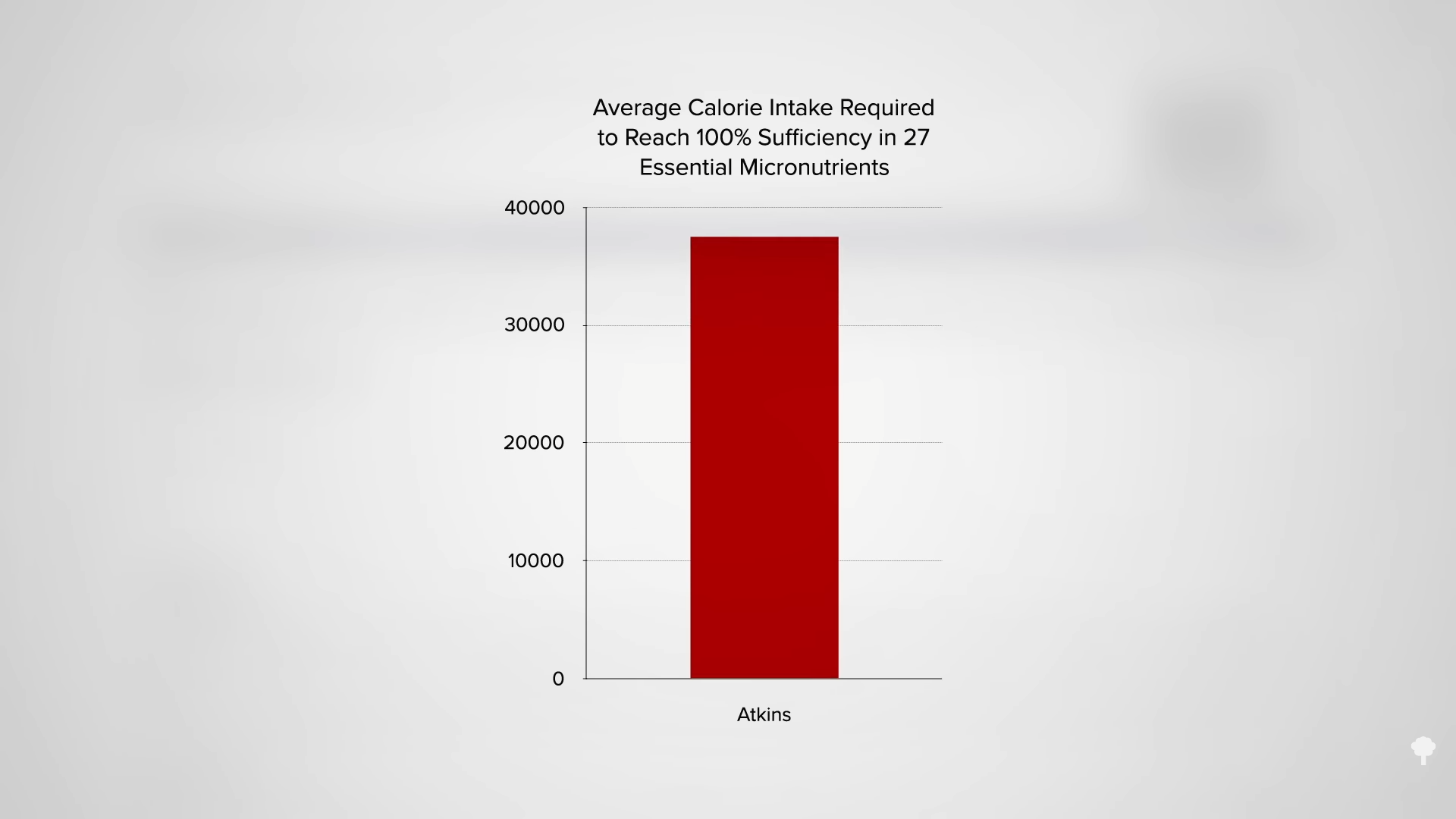
You get AGEs in your body from two sources: You can eat them preformed in your diet or make them internally from methylglyoxal if you have high blood sugar levels. On a keto diet, one would expect high exposure to preformed AGEs, since they’re found concentrated in animal-derived foods high in fat and protein, but we would expect less internal, new formation due to presumably low levels of methylglyoxal, given lower blood sugars from not eating carbs. Dartmouth researchers were surprised to find more methylglyoxal! As shown in the graph below and at 6:11 in my video, a few weeks on the Atkins diet led to a significant increase in methylglyoxal levels. Those in active ketosis did even worse, doubling the level of this glycotoxin in their bloodstream.
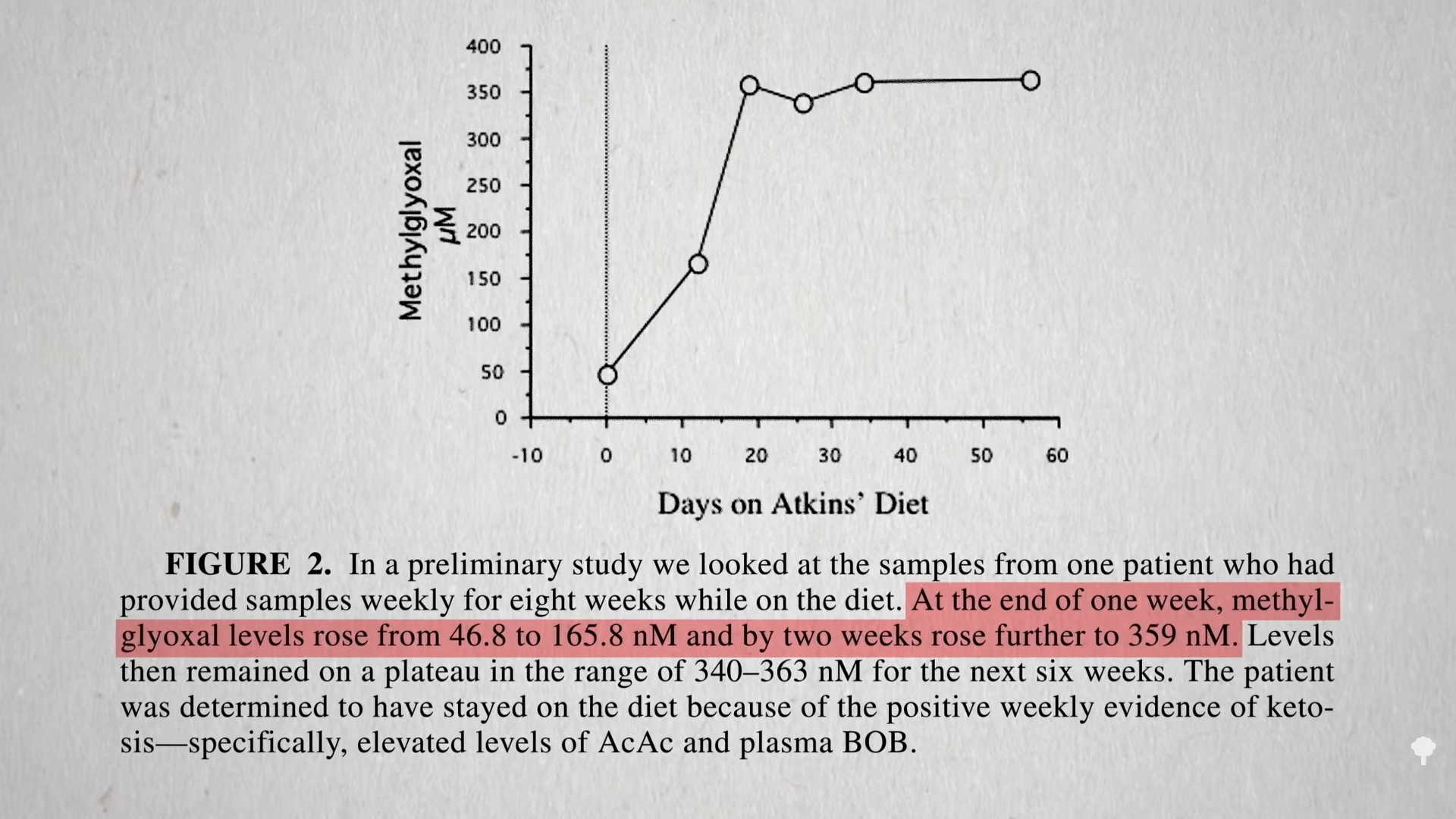
It turns out that high sugars may not be the only way to create this toxin, as you can see below and at 6:24 in my video. One of the ketones you make on a ketogenic diet is acetone (known for its starring role in nail polish remover). Acetone does more than just make keto dieters fail breathalyzer tests, “feel queasy and light-headed, and develop what’s been described as ‘rotten apple breath.’” Acetone can oxidize in the blood to form acetol, which may be a precursor for methylglyoxal. 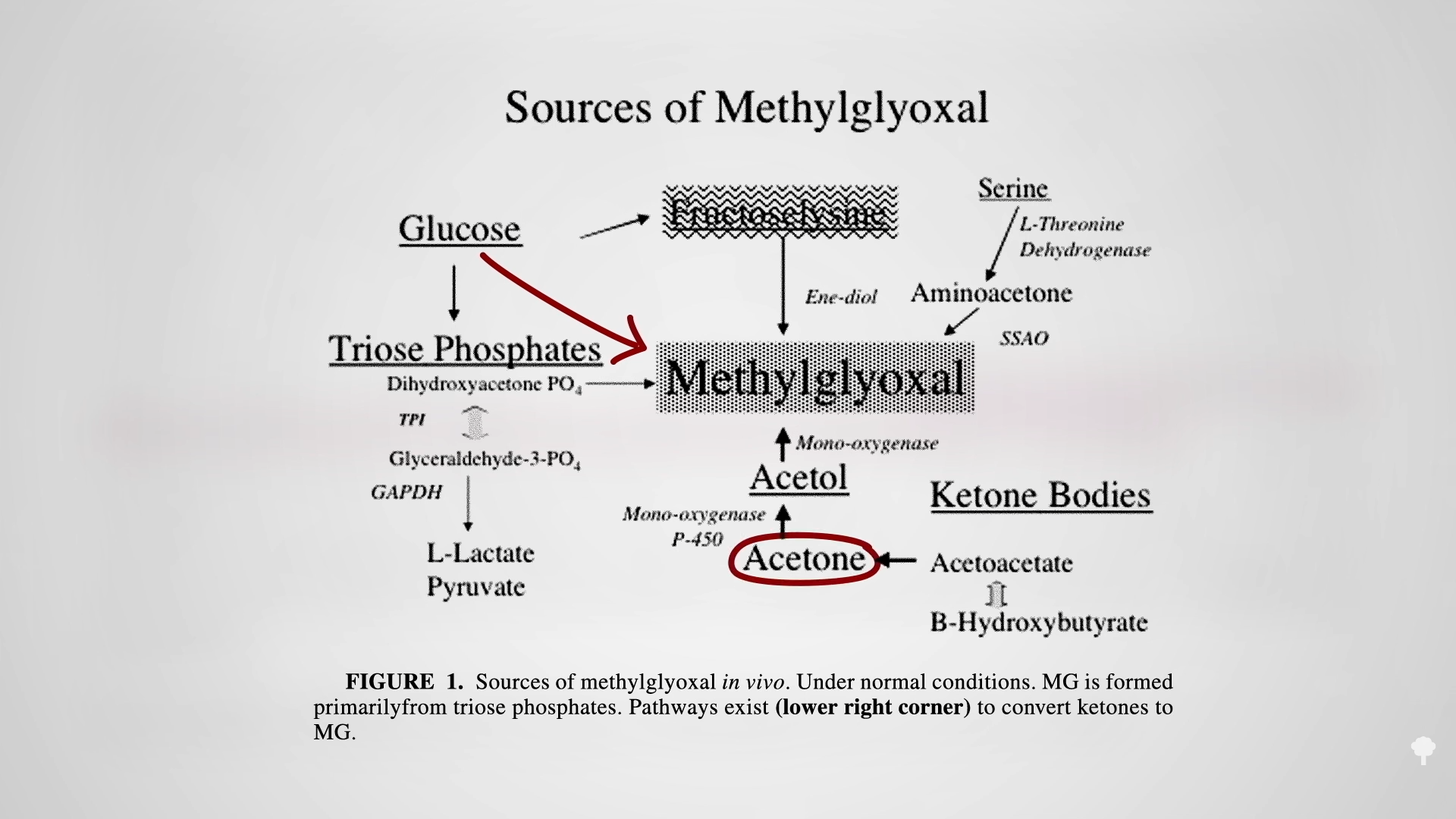
That may be why keto dieters can end up with levels of this glycotoxin as high as those with out-of-control diabetes, which can cause the nerve damage and blood vessel damage you see in diabetics. That’s another way keto dieters can end up with a heart attack. The irony of treating diabetes with a ketogenic diet may extend beyond just making the underlying diabetes worse, but by mimicking some of the disease’s dire consequences.
This is part of a seven-video series on keto, which you can find in related videos below.
I also recently tackled diabetes.
Michael Greger M.D. FACLM
Source link