The Buchinger-modified fasting program is put to the test.
A century ago, fasting—“starvation, as a therapeutic measure”—was described as “the ideal measure for the human hog…” (Fat shaming is not a new invention in the medical literature.) I’ve covered fasting for weight loss extensively in a nine-video series, but what about all the other purported benefits? I also have a video series on fasting for hypertension, but what about psoriasis, eczema, type 2 diabetes, lupus, metabolic disorder, rheumatoid arthritis, other autoimmune disorders, depression, and anxiety? Why hasn’t it been tested more?
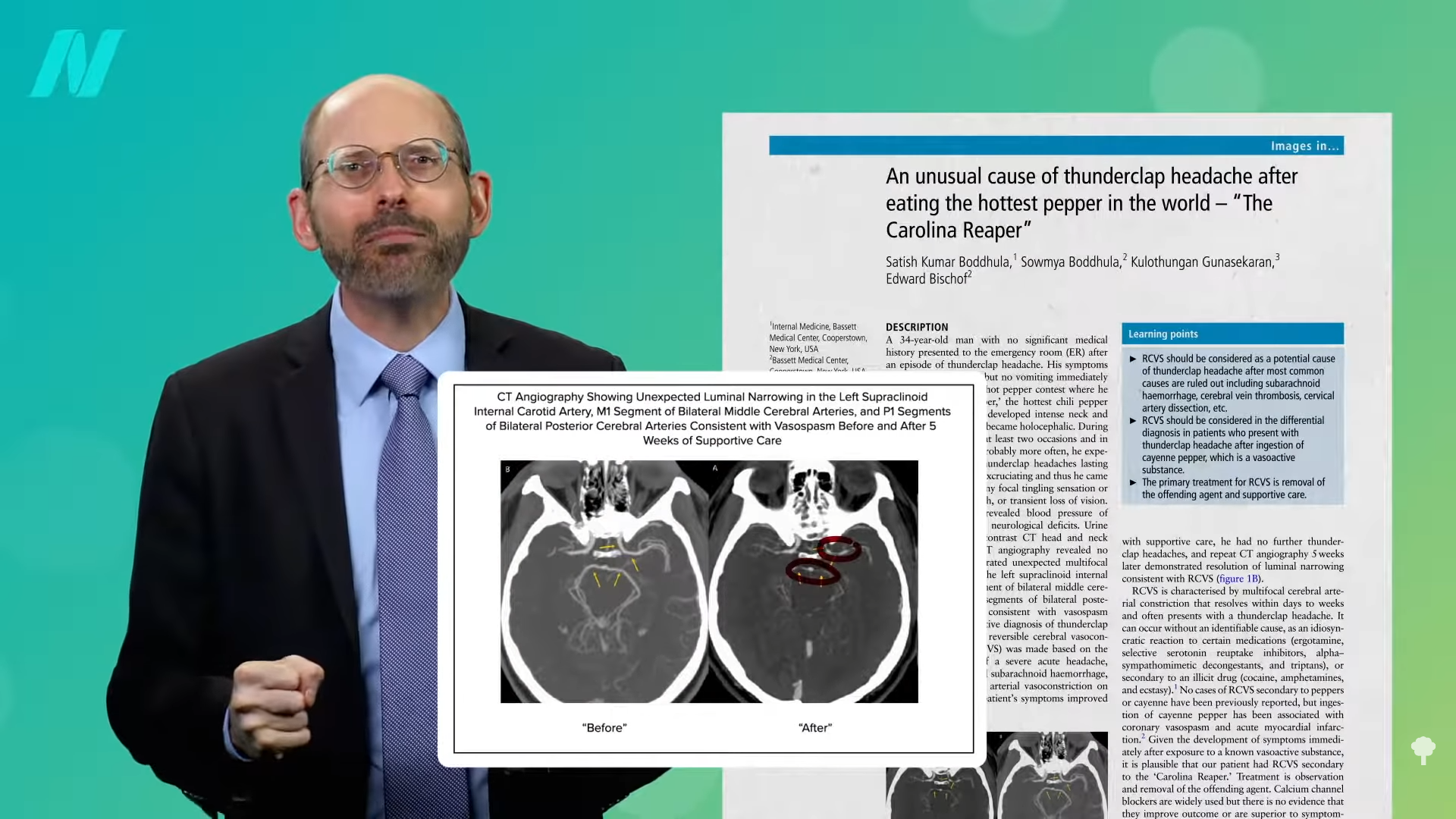
One difficulty with fasting research is: What do you mean by fasting? When I think of fasting, I think of water-only fasting, but, in Europe, they tend to practice “modified therapeutic fasting,” also known as Buchinger fasting, which is more like a very low-calorie juice fasting with some vegetable broth. Some forms of fasting may not even cut calories at all. As you can see below and at 1:09 in my video The World’s Largest Fasting Study, Ramadan fasting, for example, is when devout Muslims abstain from food and drink from sunrise to sunset, yet, interestingly, they end up eating the same amount—or even more food—overall.
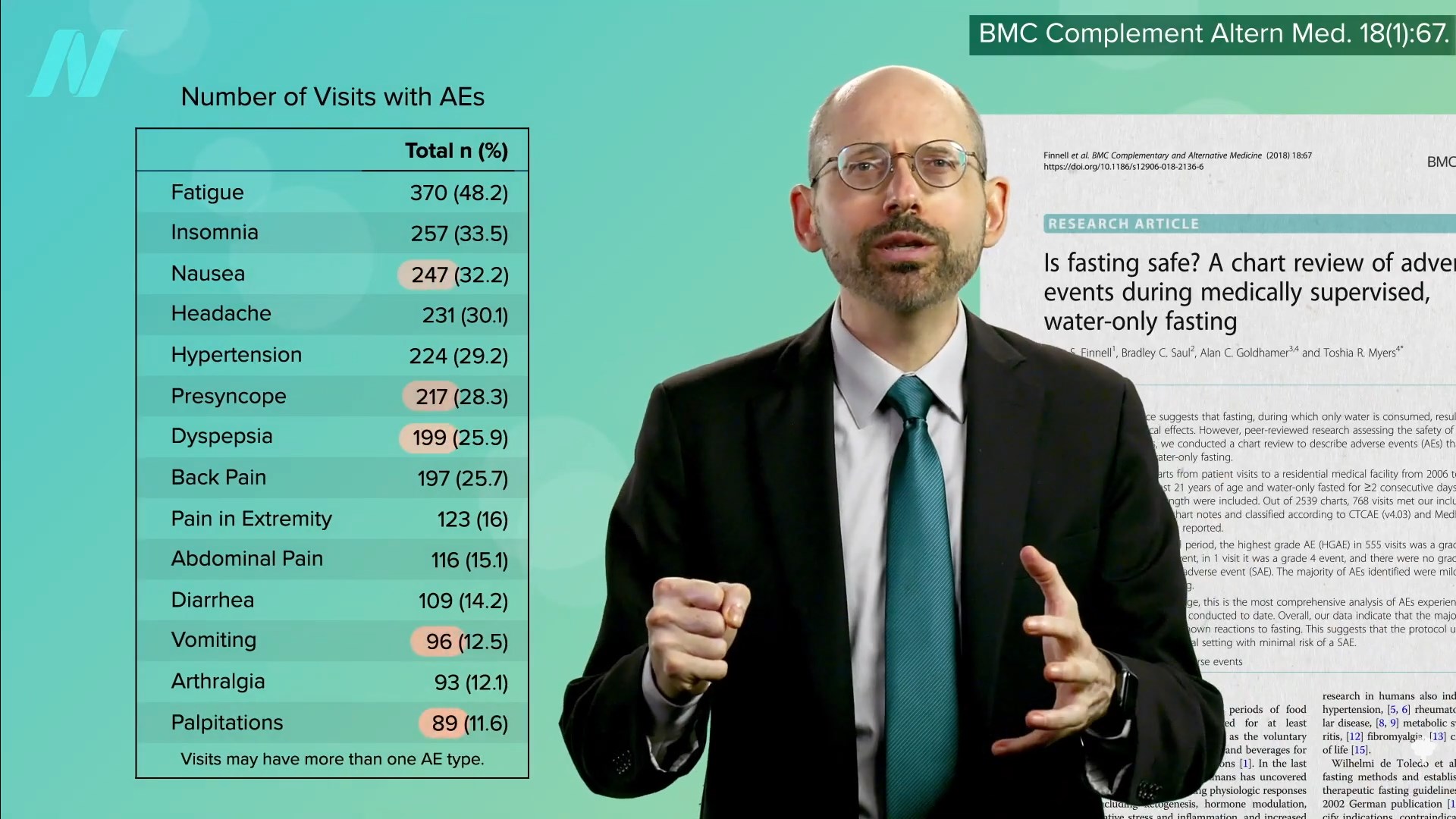
The largest study on fasting to date was published in 2019. More than a thousand individuals were put through a modified fast, cutting daily intake down to about ten cups of water, a cup of fruit juice, and a cup of vegetable soup. They reported very few side effects. In contrast, the latest water-only fasting data from a study that involved half as many people reported nearly 6,000 adverse effects. Now, the modified fasting study did seem to try to undercount adverse effects by only counting reported symptoms if they were repeated three times. However, adverse effects like nausea, feeling faint, upset stomach, vomiting, or palpitations were “observed only in single cases,” whereas the water-only fasting study reported about 100 to 200 of each, as you can see below and at 2:05 in my video. What about the benefits though?
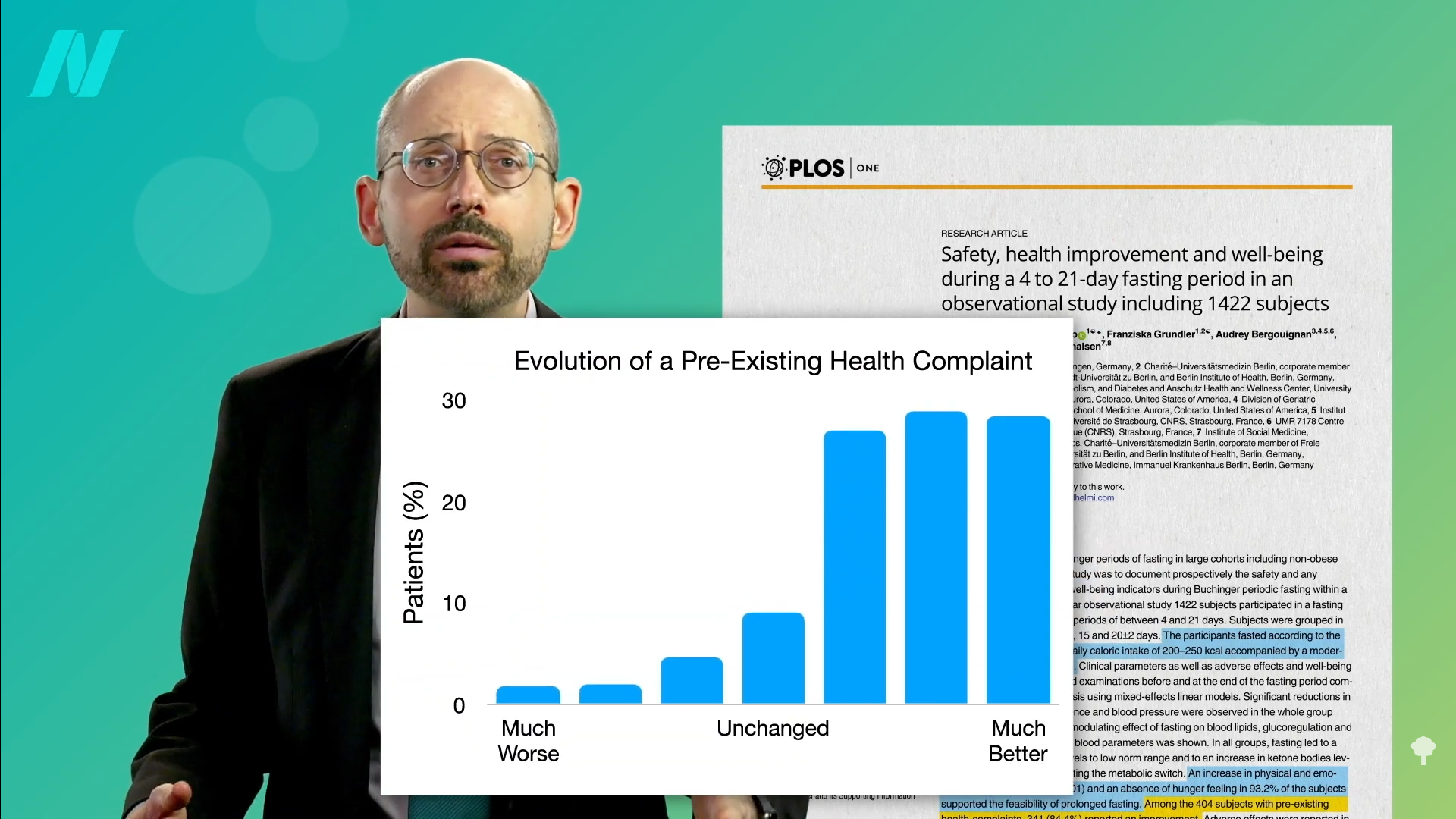
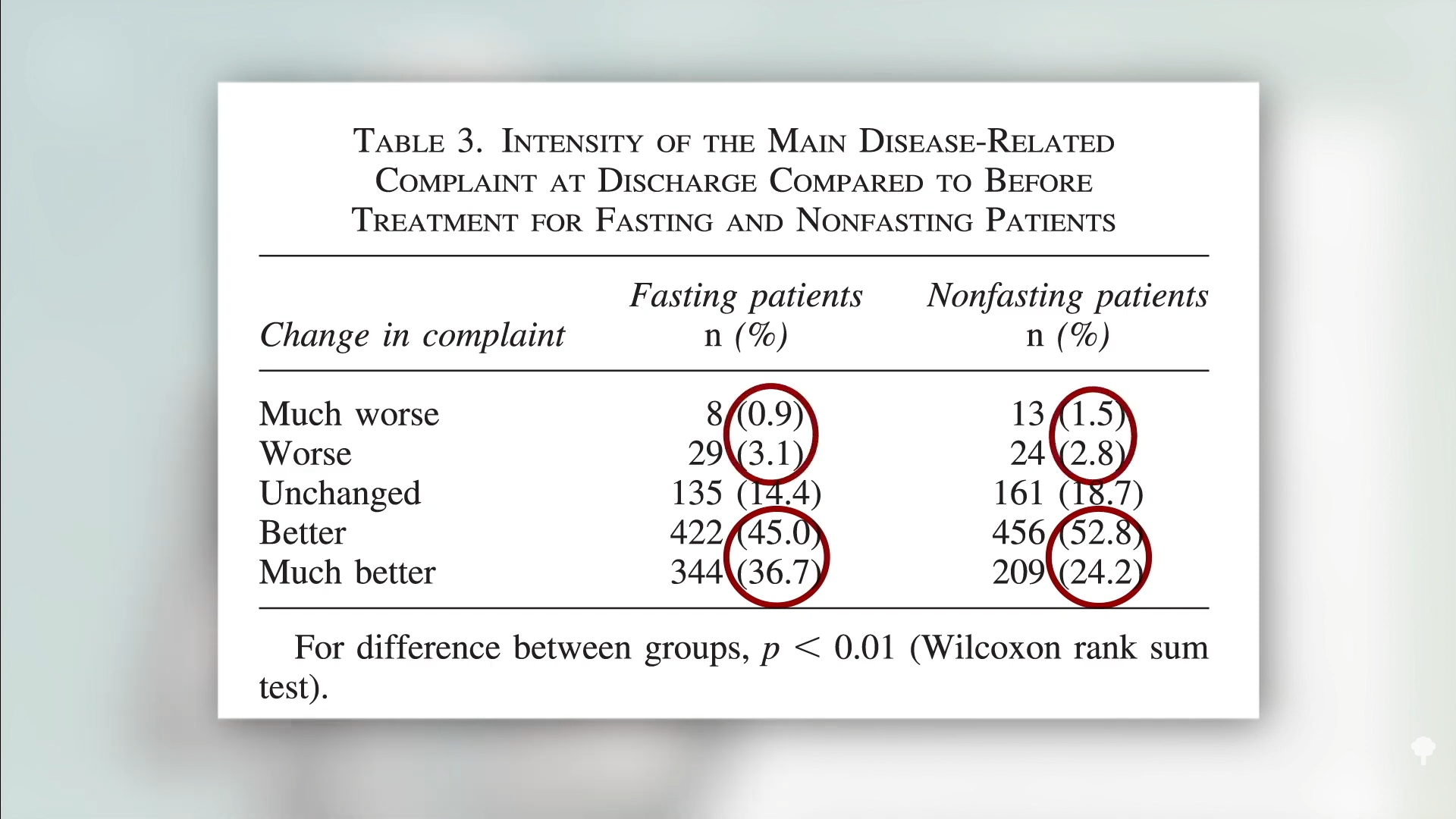
In the modified fasting study, participants self-reported improvements in physical and emotional well-being, along with a surprising lack of hunger. What’s more, the vast majority of those who came in with a pre-existing health complaint reported feeling better, with less than 10 percent stating that their condition worsened, as you can see in the graph below and at 2:24 in my video.
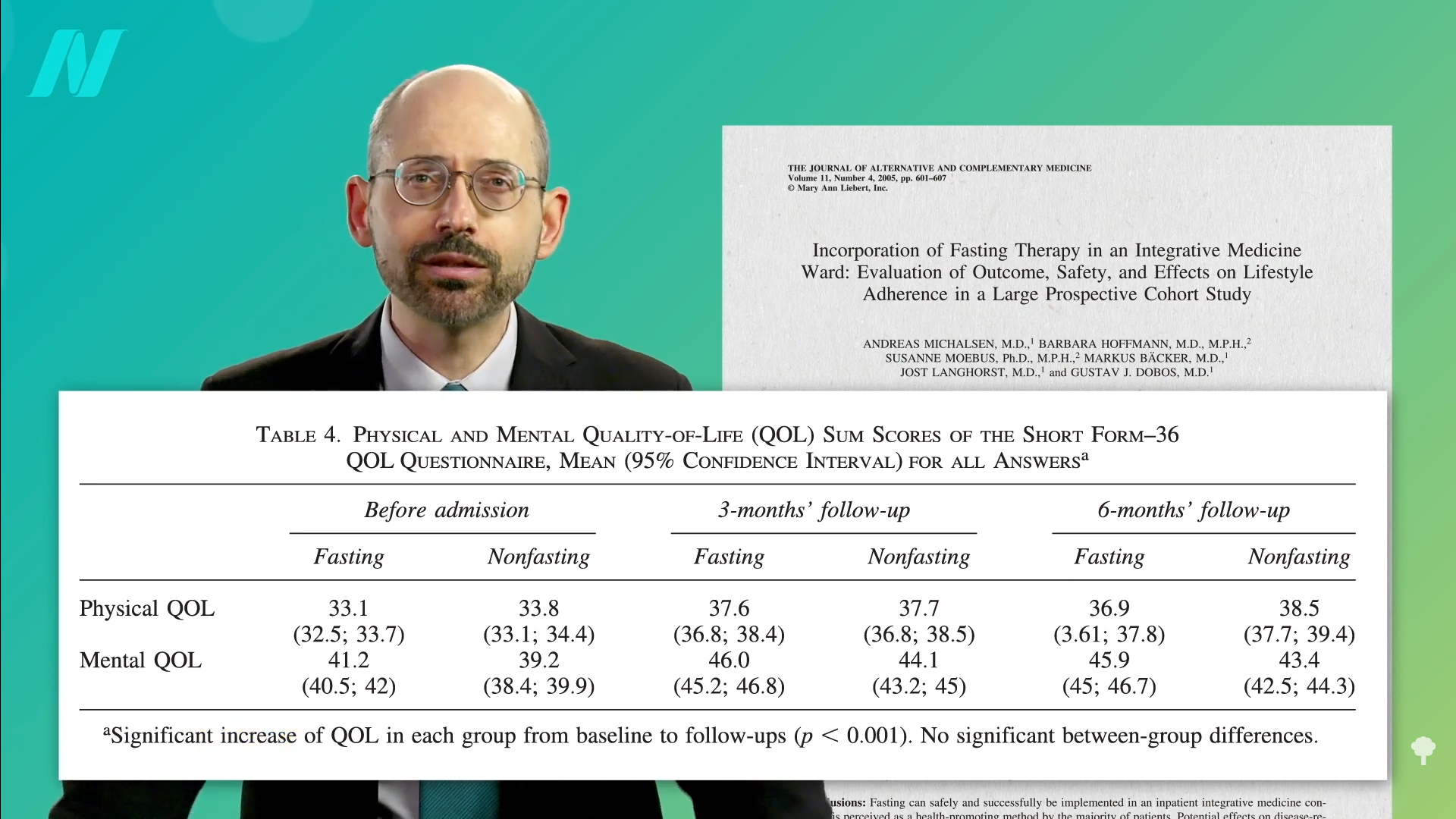
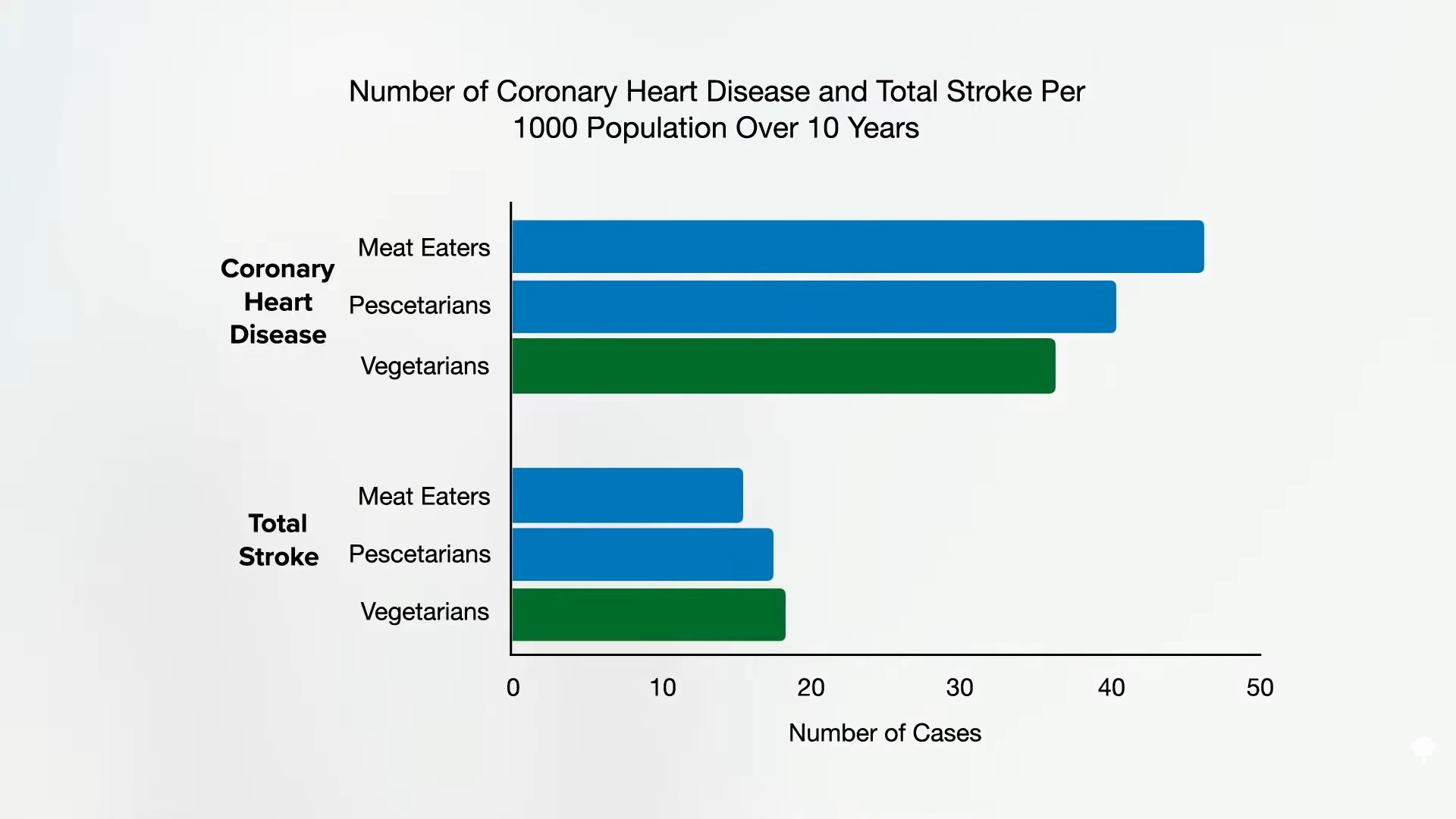
However, the study participants didn’t just fast; they also engaged in a lifestyle program, which included being on a plant-based diet before and after the modified fast. If only the researchers had had some study participants follow the healthier, plant-based diet without the fast to tease out fasting’s effects. Oh, but they did! About a thousand individuals fasted for a week on the same juice and vegetable soup regimen and others followed a normocaloric (normal calorie) vegetarian diet.
As you can see below and at 2:54 in my video, both groups experienced significant increases in both physical and mental quality of life, and, interestingly, there was no significant difference between the groups.
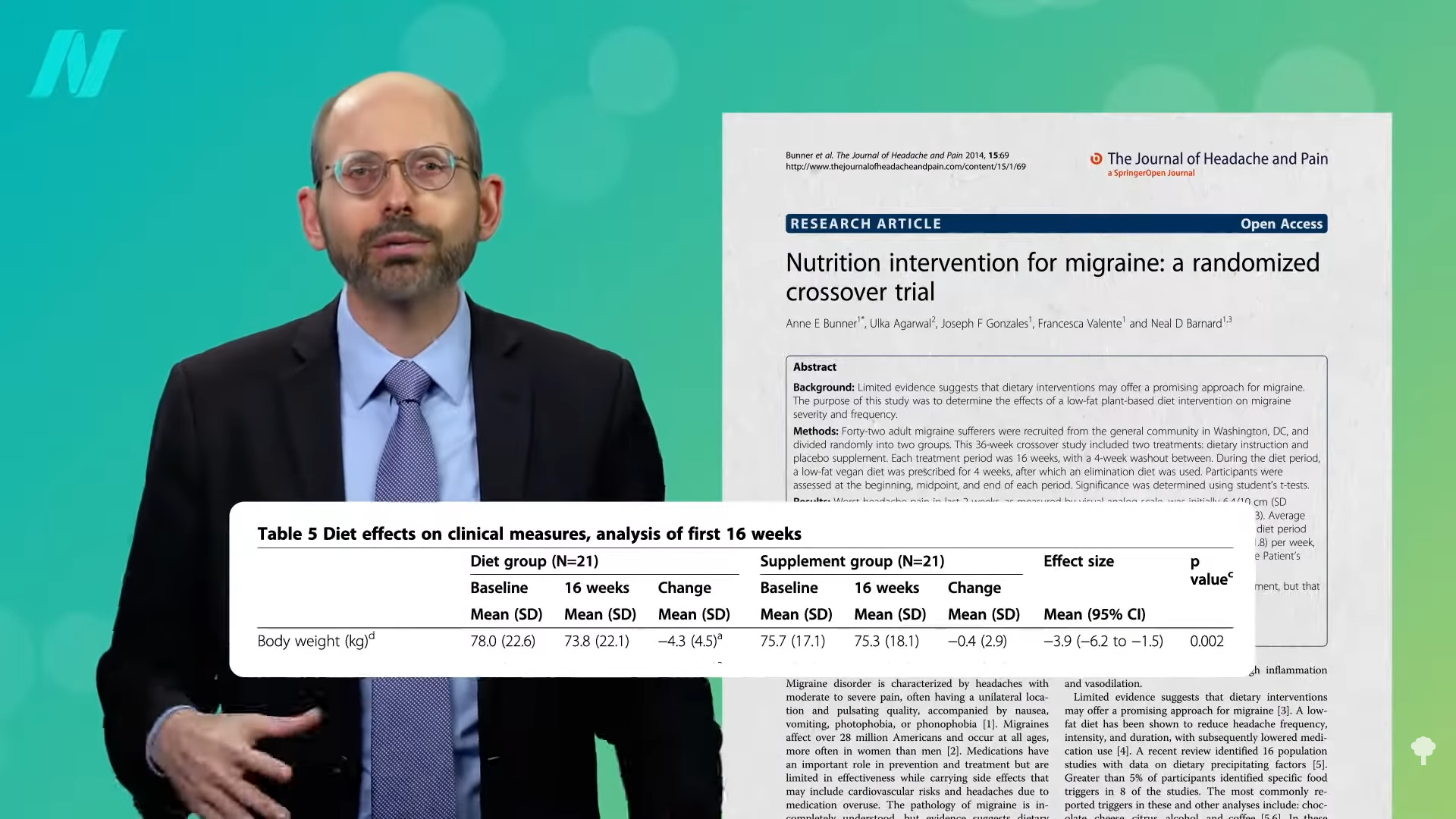
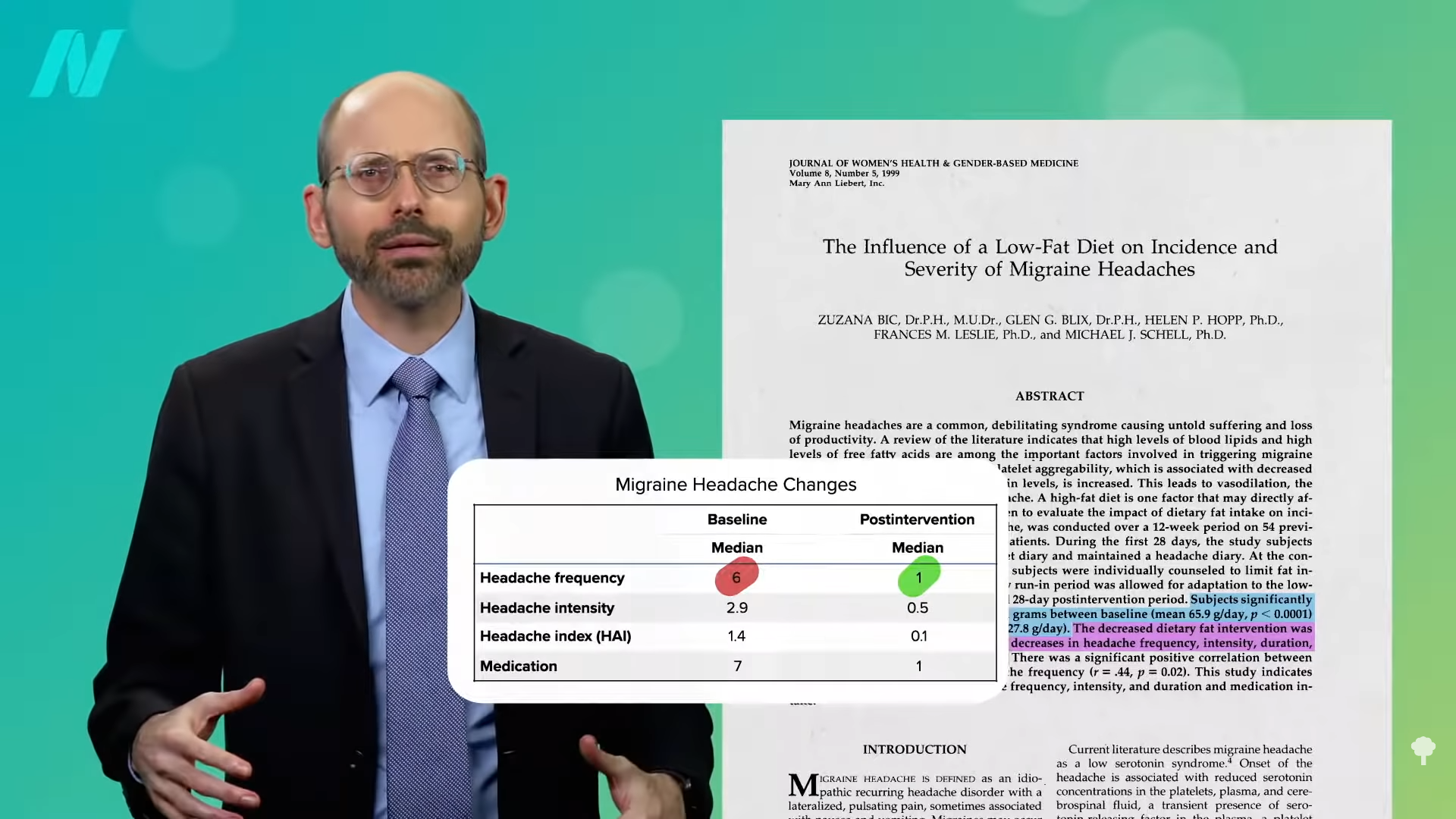
In terms of their major health complaints—including rheumatoid arthritis; chronic pain syndromes, like osteoarthritis, fibromyalgia, and back pain; inflammatory and irritable bowel disease; chronic pulmonary diseases; and migraine and chronic tension-type headaches—the fasting group appeared to have an edge, but both groups did well, with about 80 percent reporting improvements in their condition and only about 4 percent reporting feeling worse, as you can see below and at 3:25 in my video.
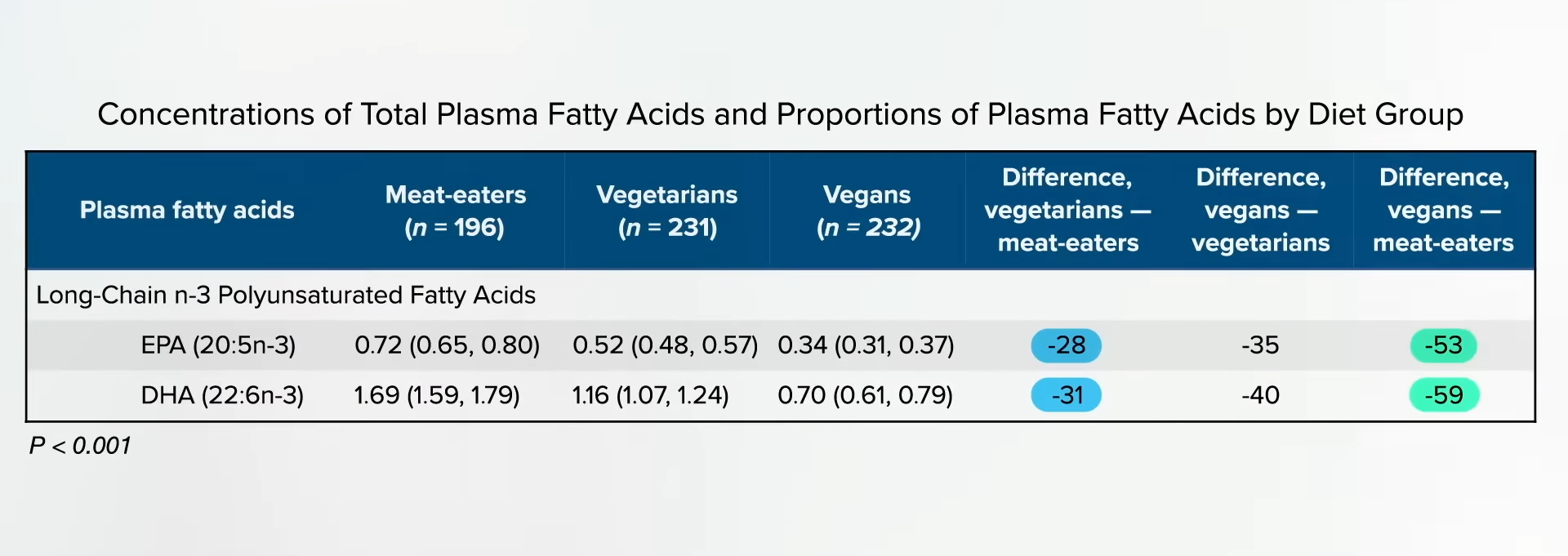
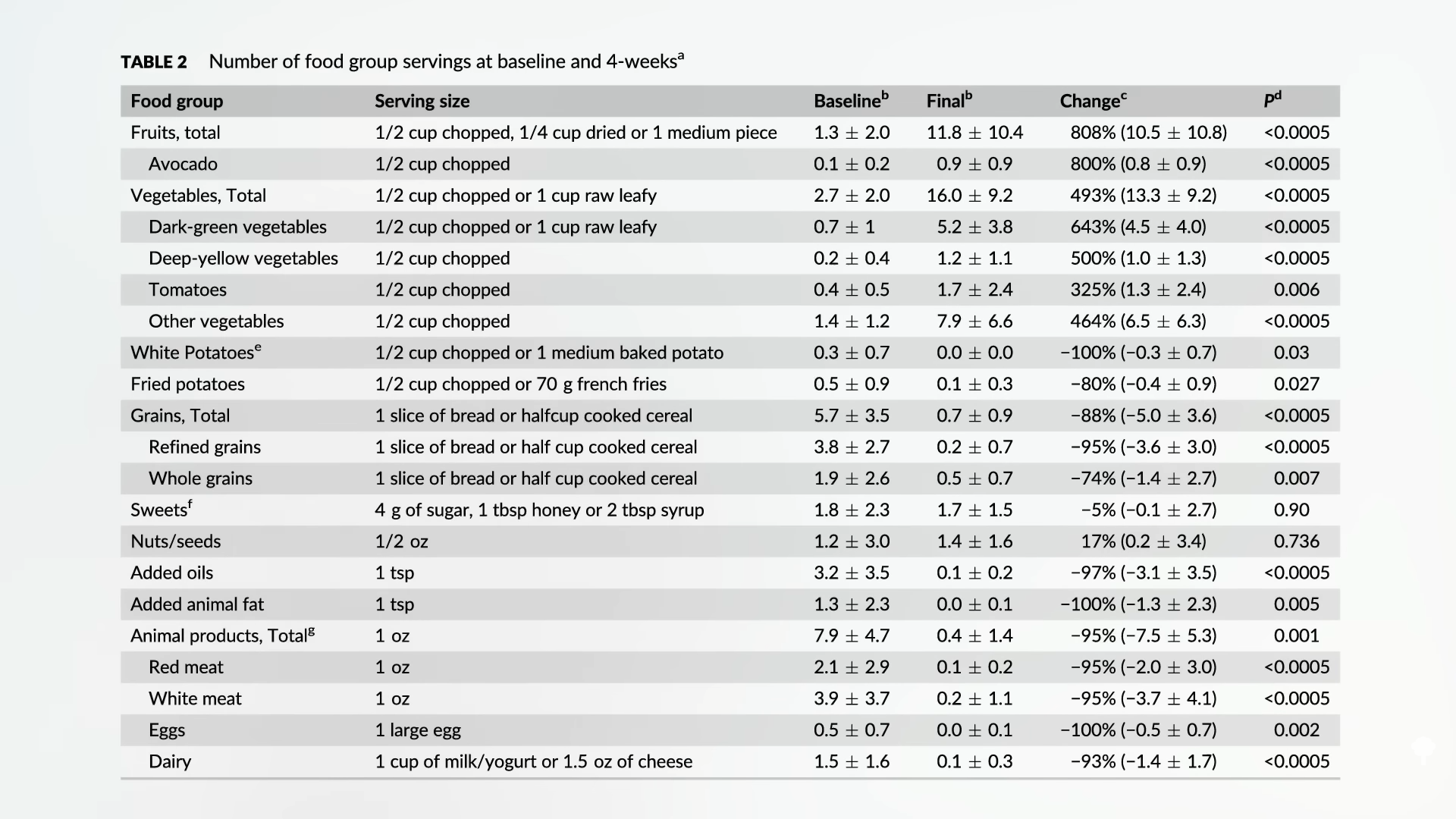
Now, this was not a randomized study; people chose which treatment they wanted to follow. So, maybe, for example, those choosing fasting were sicker or something. Also, the improvements in quality of life and disease status were all subjective self-reporting, which is ripe for placebo effects. There was no do-nothing control group, and the response rates to the follow-up quality of life surveys were only about 60 to 70 percent, which also could have biased the results. But extended benefits are certainly possible, given they all tended to improve their diets, as you can see below and at 4:00 in my video.
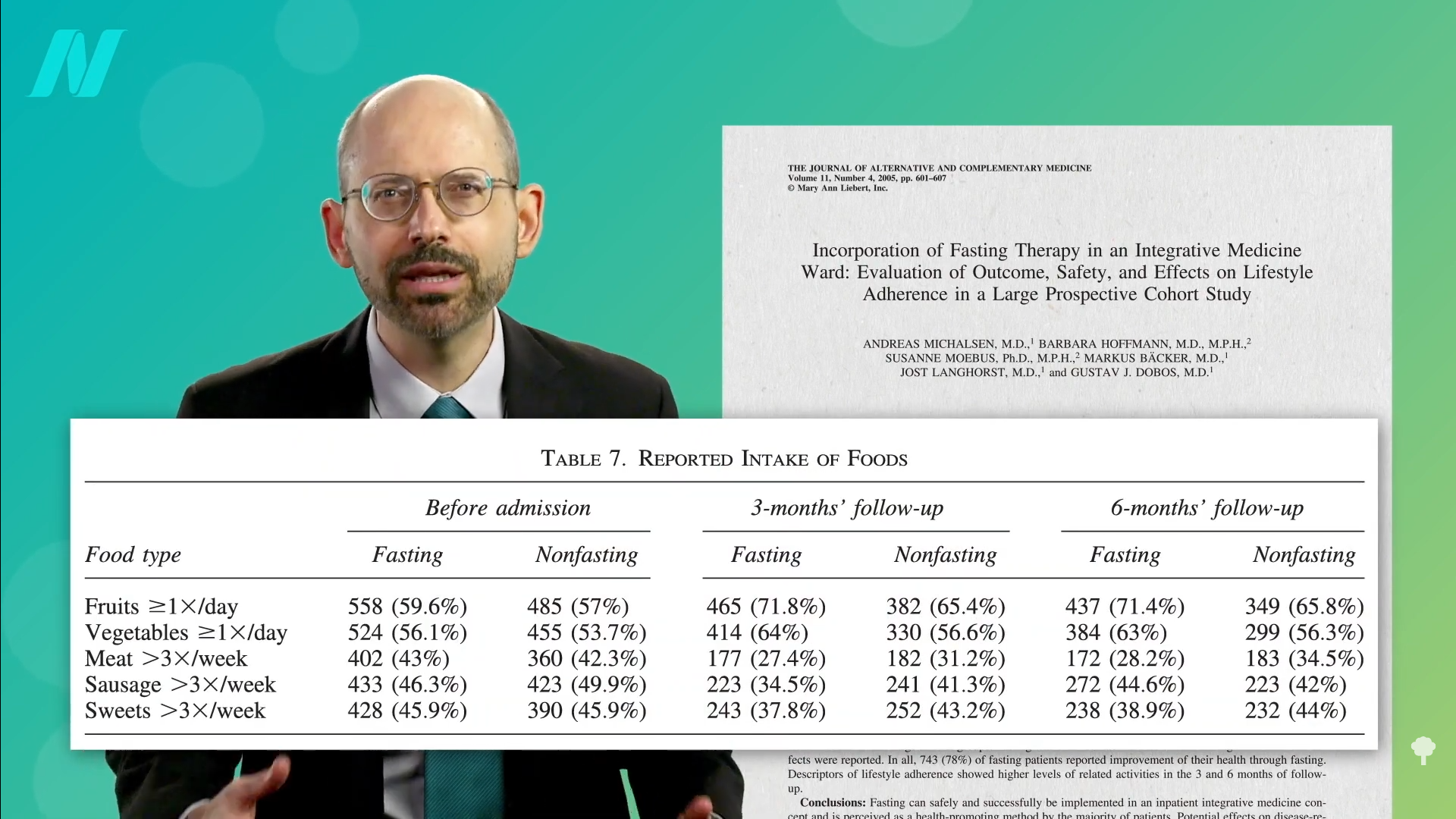
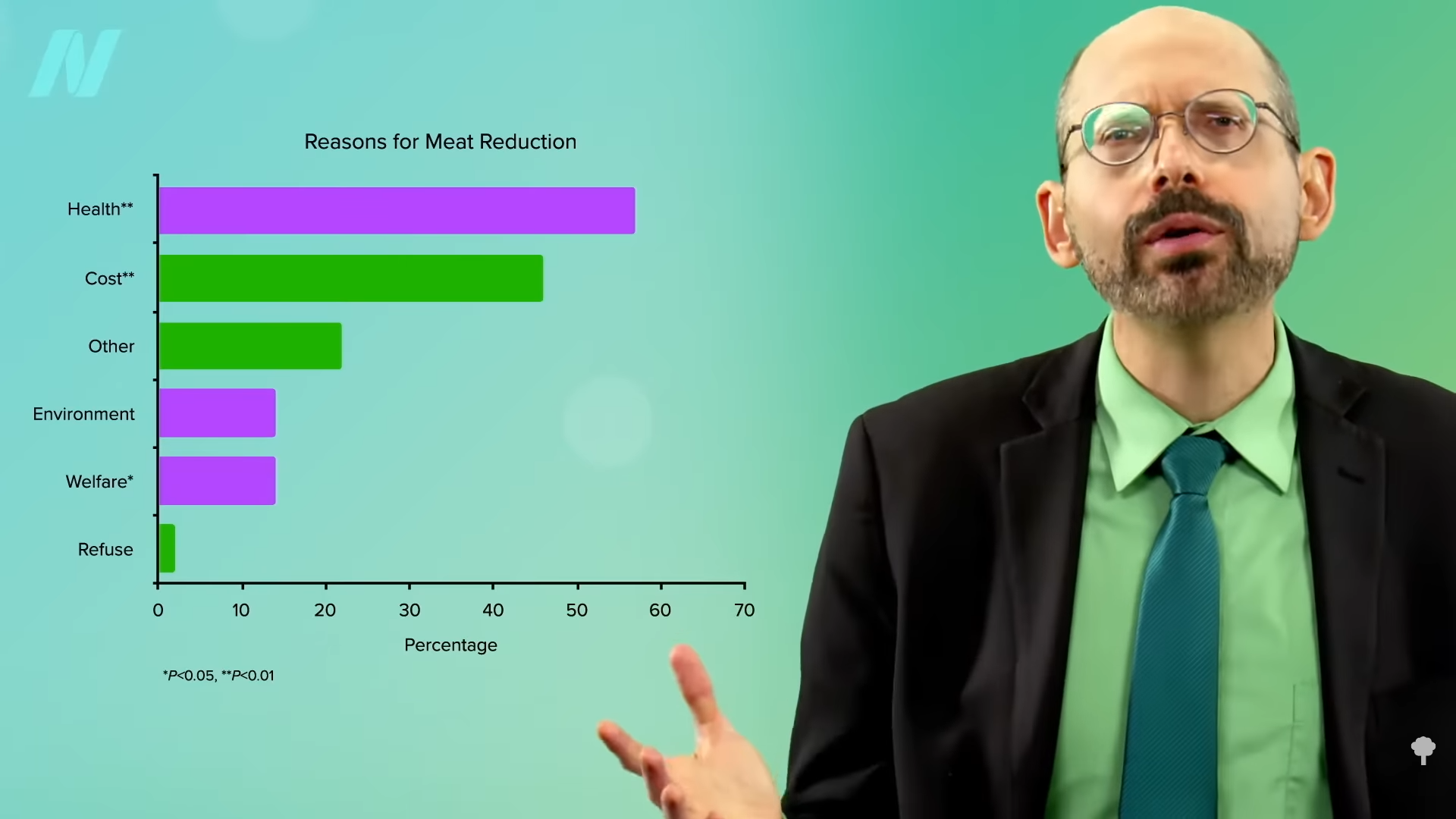
They ate more fruits and vegetables, and less meats and sweets, and therein may lie the secret. “Principally, the experience of fasting may support motivation for lifestyle change. Most fasters experience clarity of mind and feel a ‘letting go’ of past actions and experiences and thus may develop a more positive attitude toward the future.”
As a consensus panel of fasting experts concluded, “Nutritional therapy (theory and practice) is a vital and integral component of fasting. After the fasting therapy and refeeding period, nutrition should follow the recommendations/concepts of a…plant-based whole-food diet…”
If you missed the previous video, check out The Benefits of Fasting for Healing.
Michael Greger M.D. FACLM
Source link









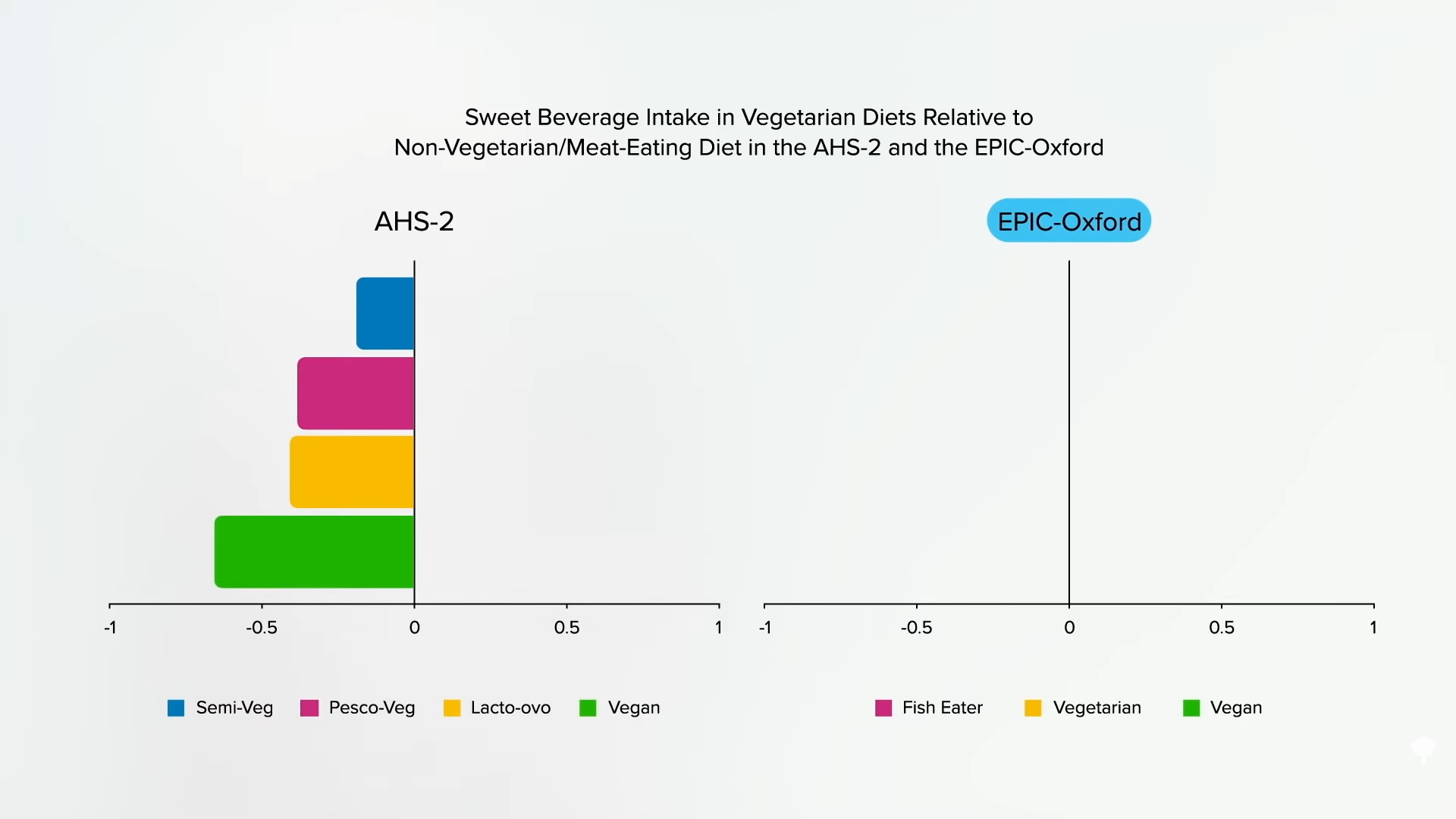
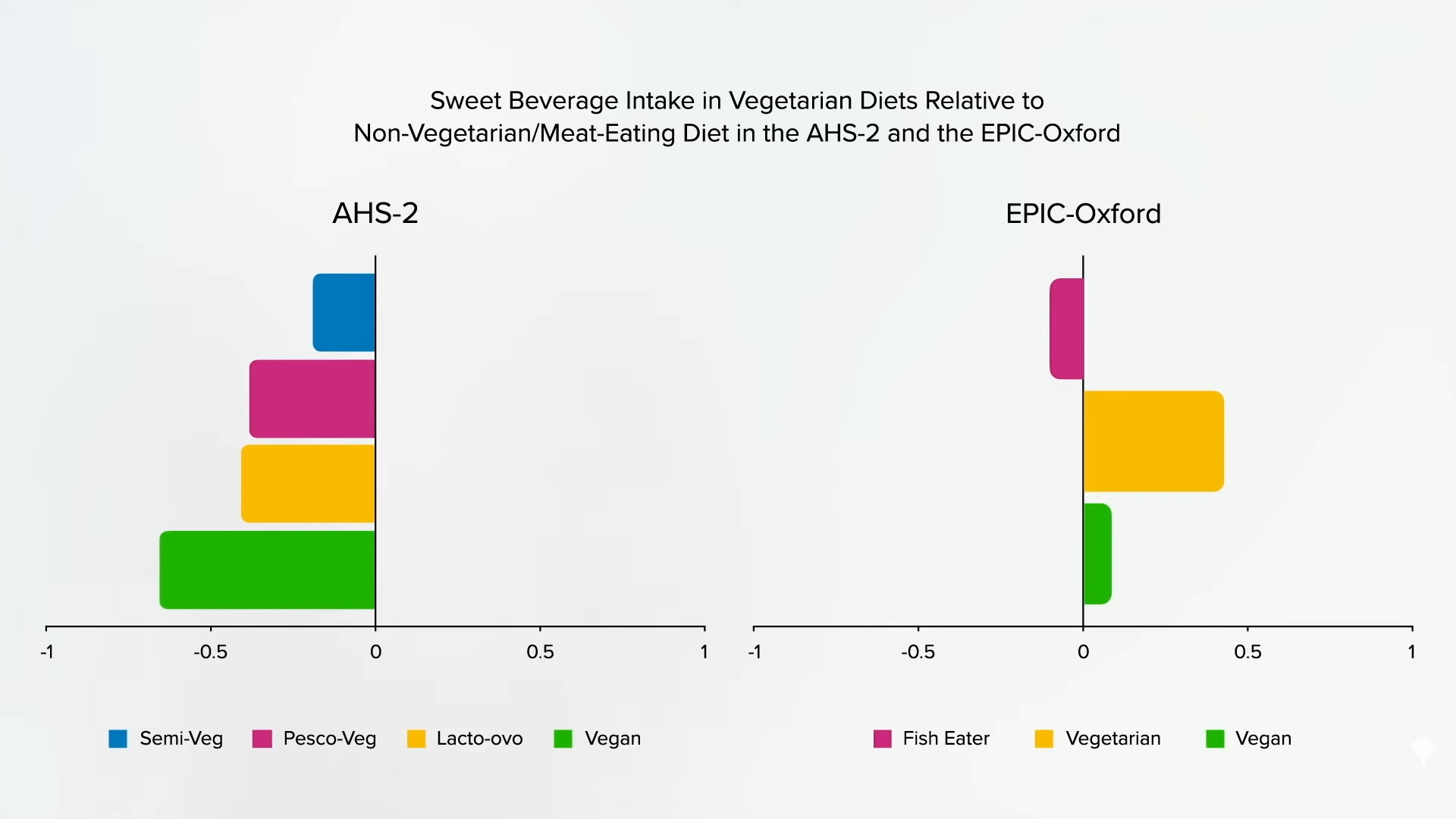
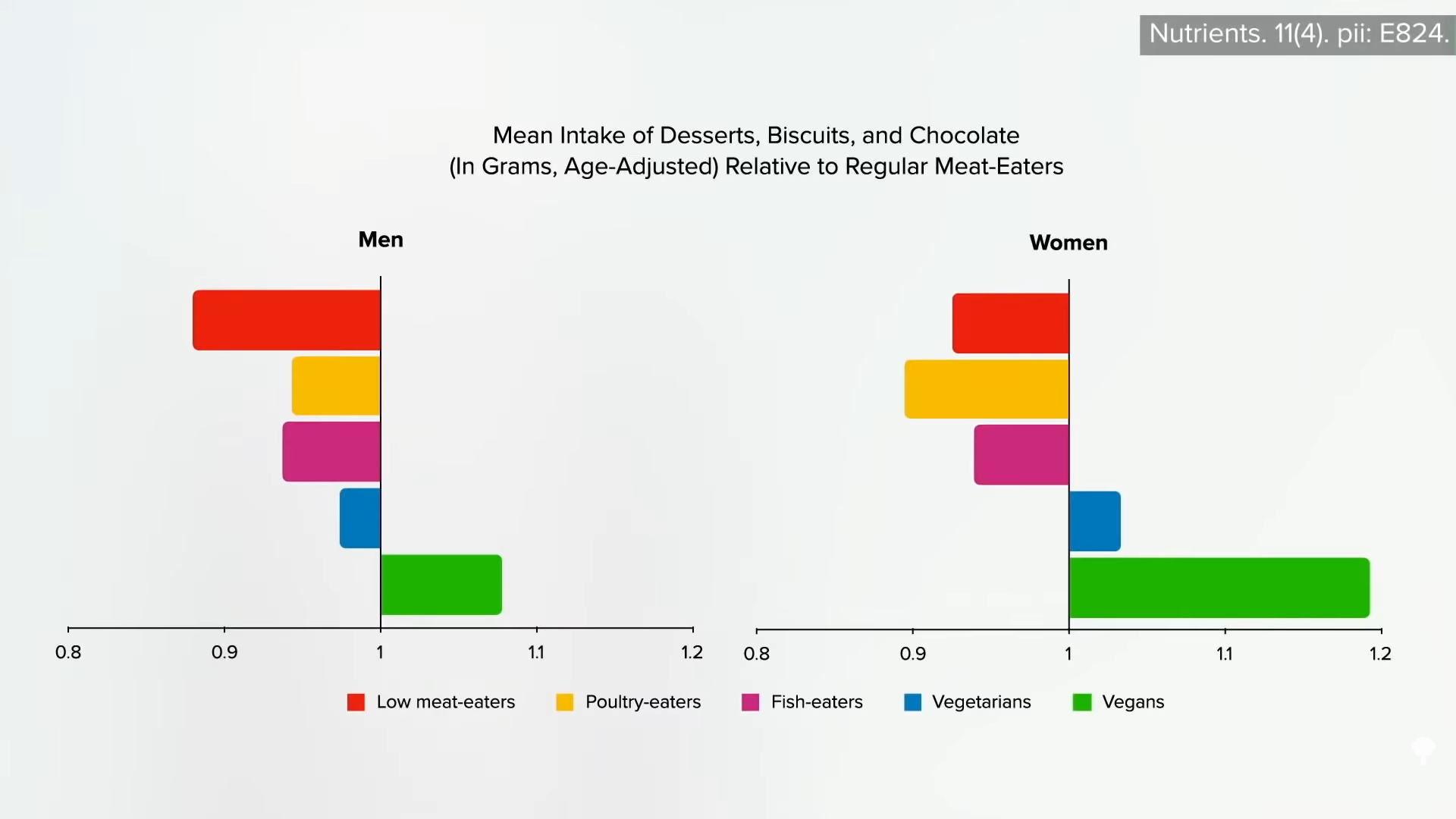
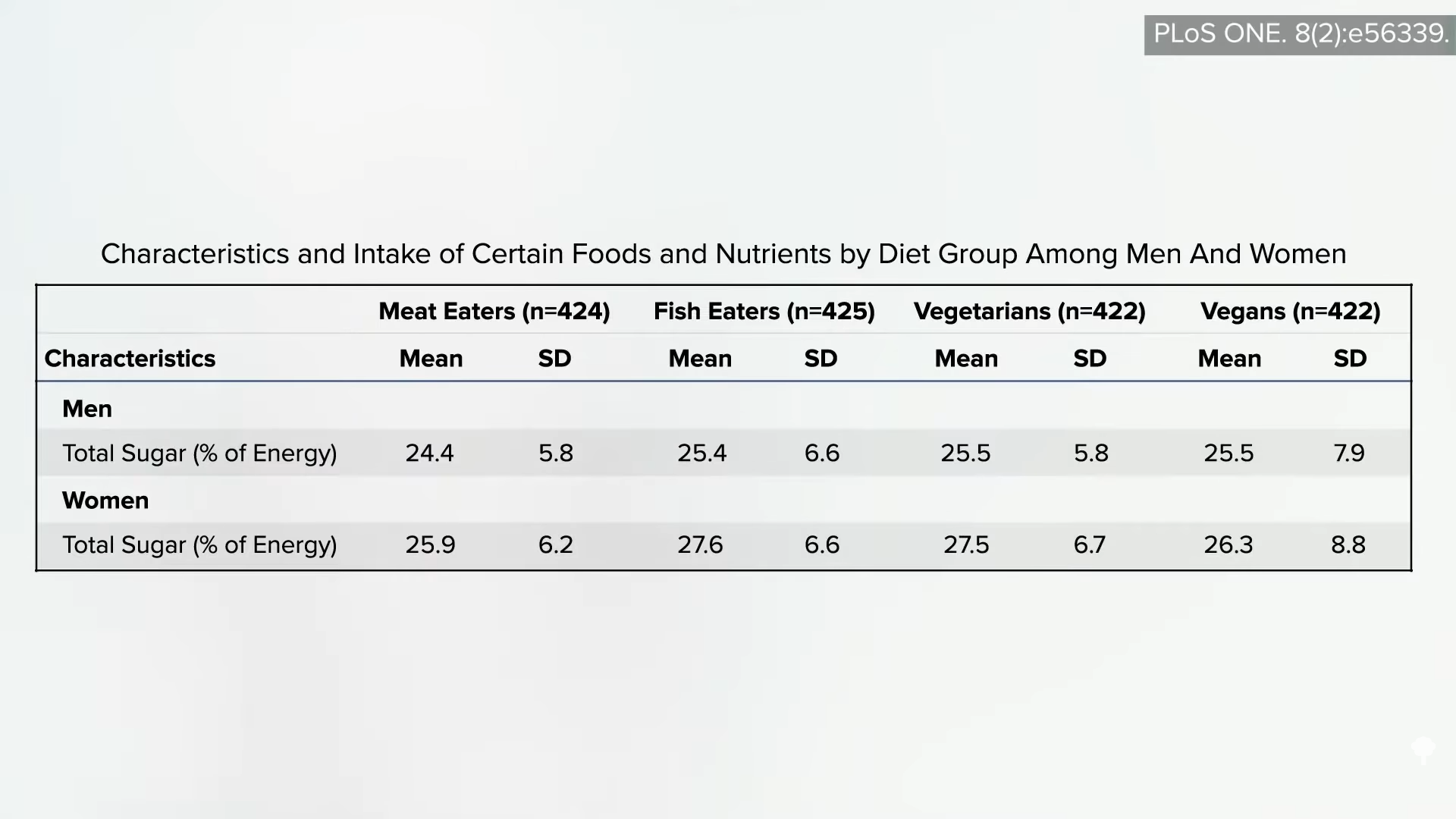
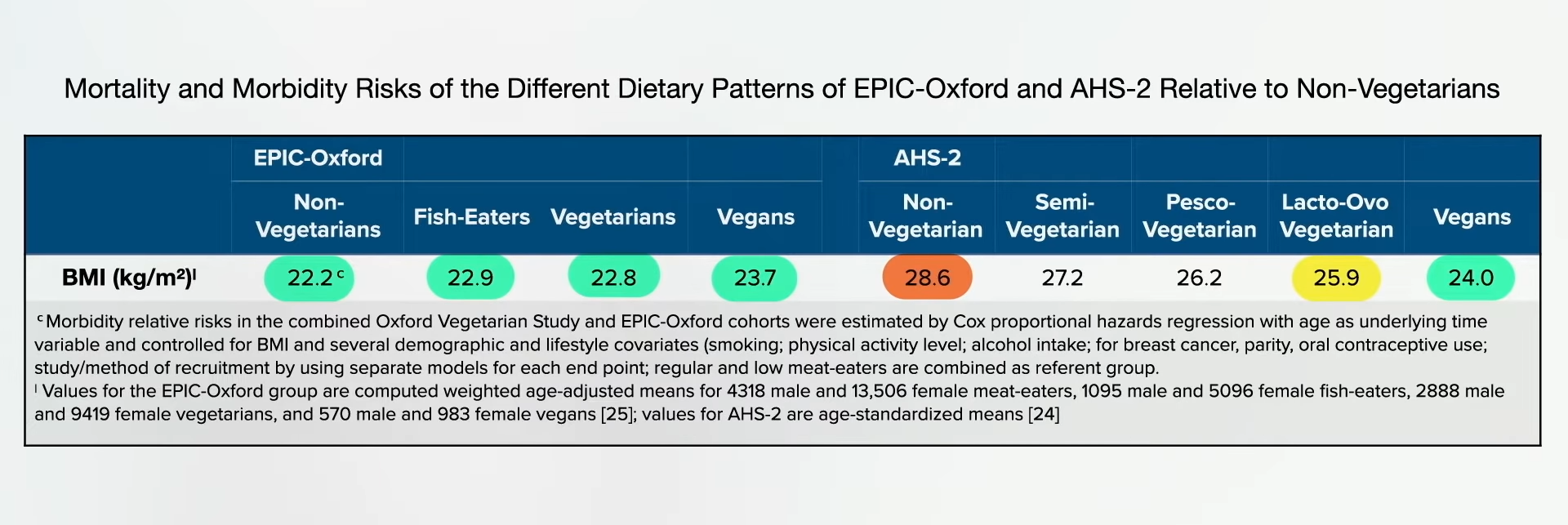

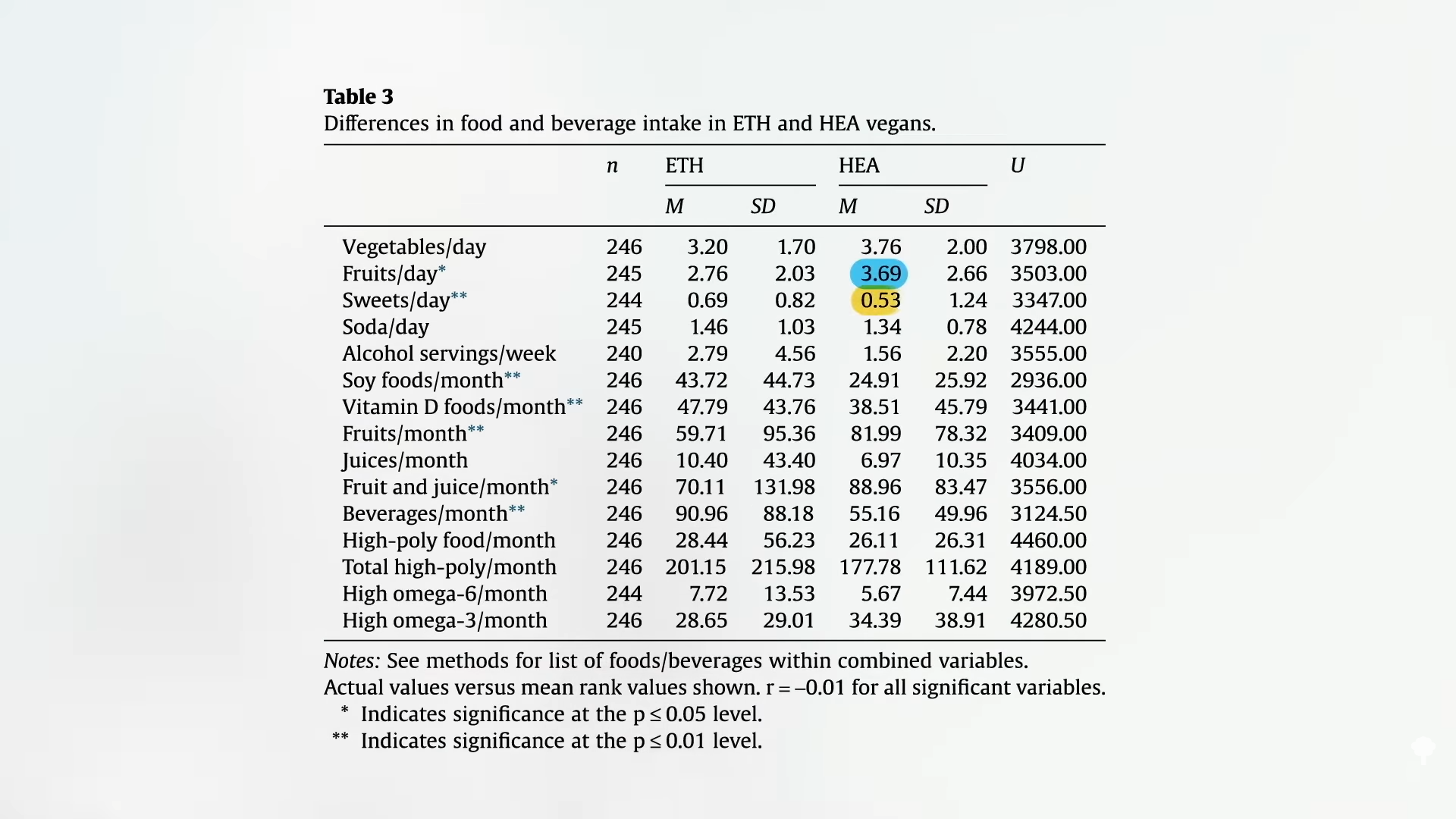
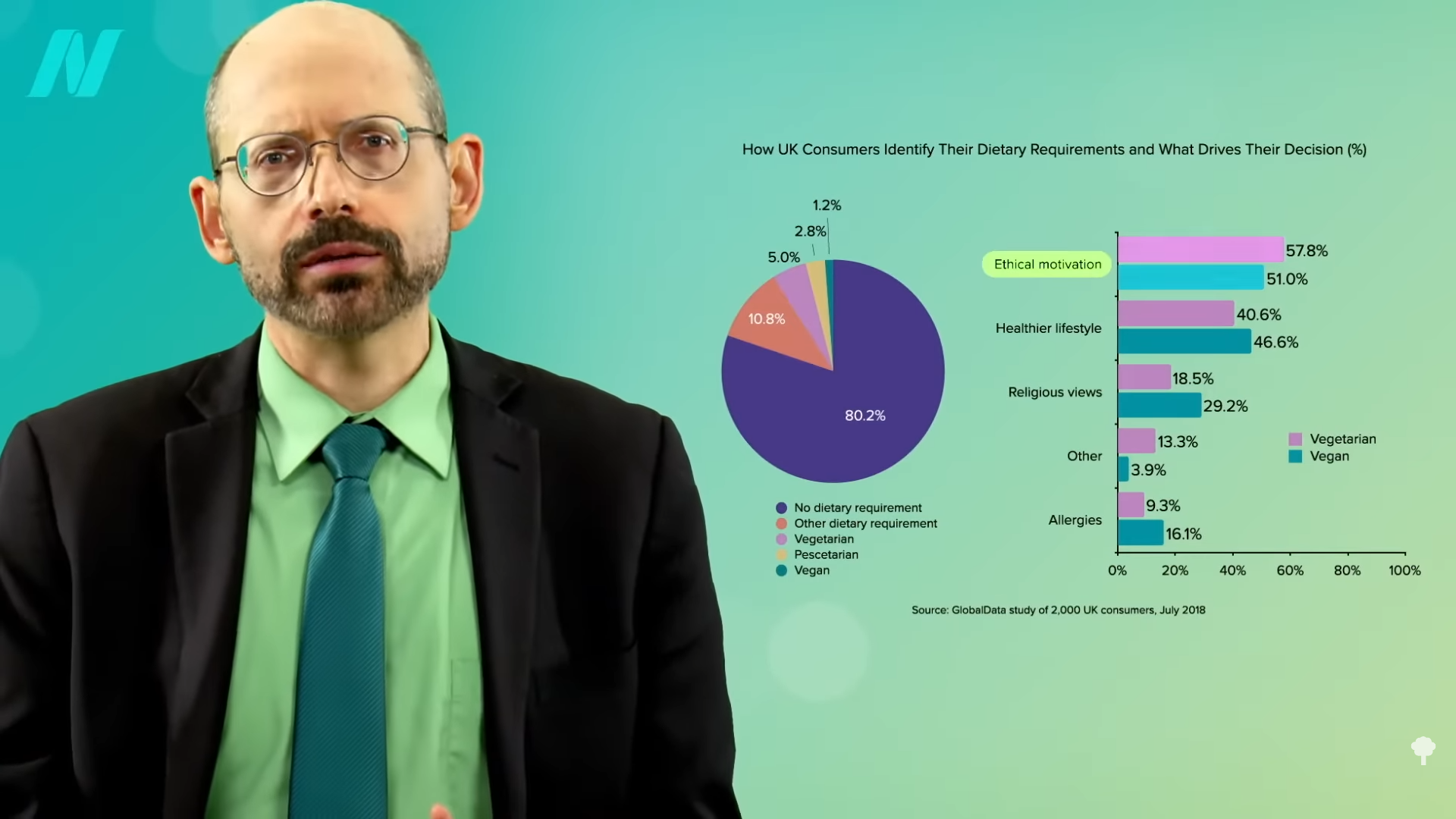




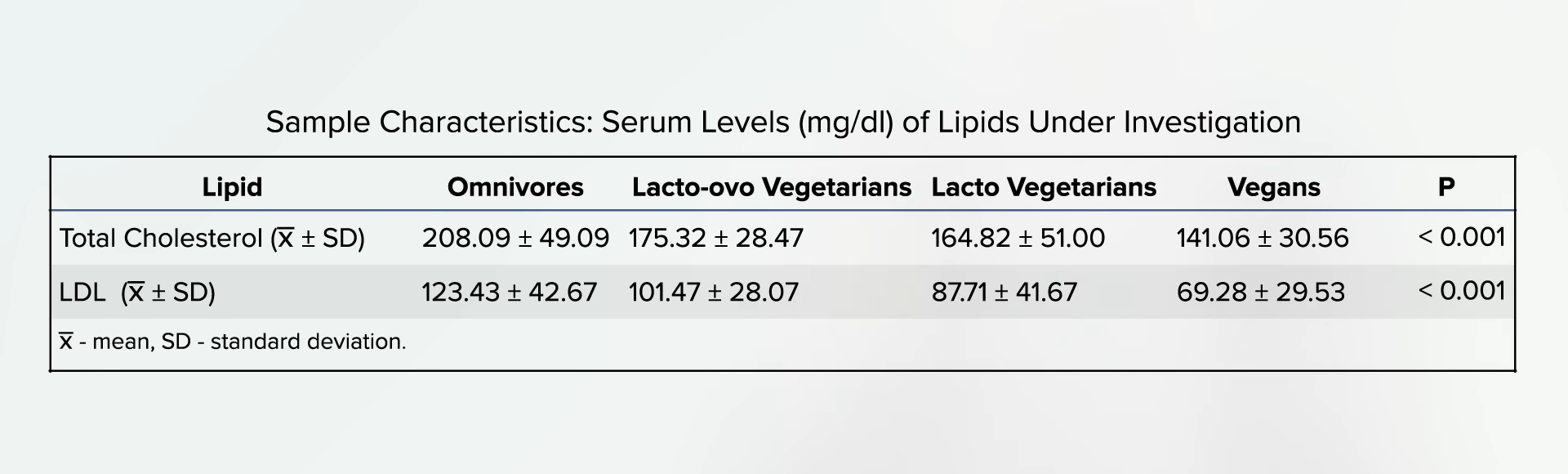



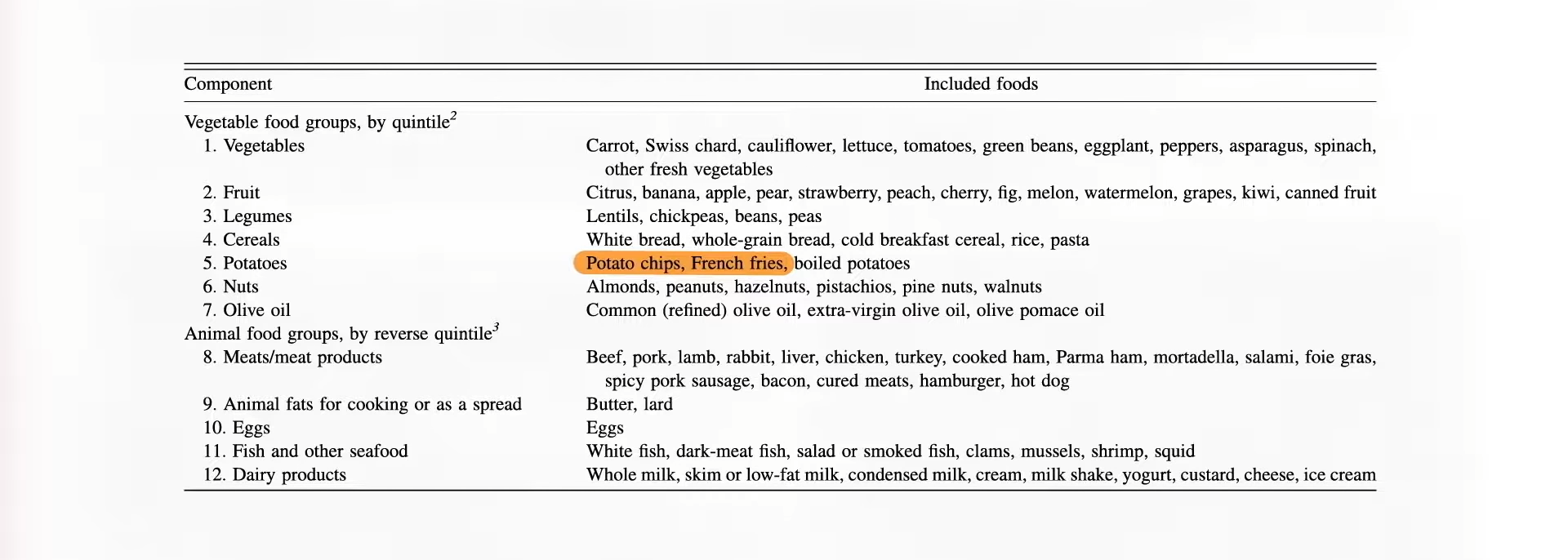
 As a physician, labels like vegetarian and vegan just tell me what you don’t eat, but there are a lot of unhealthy vegetarian fare like French fries, potato chips, and soda pop. That’s why I prefer the term whole food and plant-based nutrition. That tells me what you do eat—a diet centered around the healthiest foods out there.
As a physician, labels like vegetarian and vegan just tell me what you don’t eat, but there are a lot of unhealthy vegetarian fare like French fries, potato chips, and soda pop. That’s why I prefer the term whole food and plant-based nutrition. That tells me what you do eat—a diet centered around the healthiest foods out there.