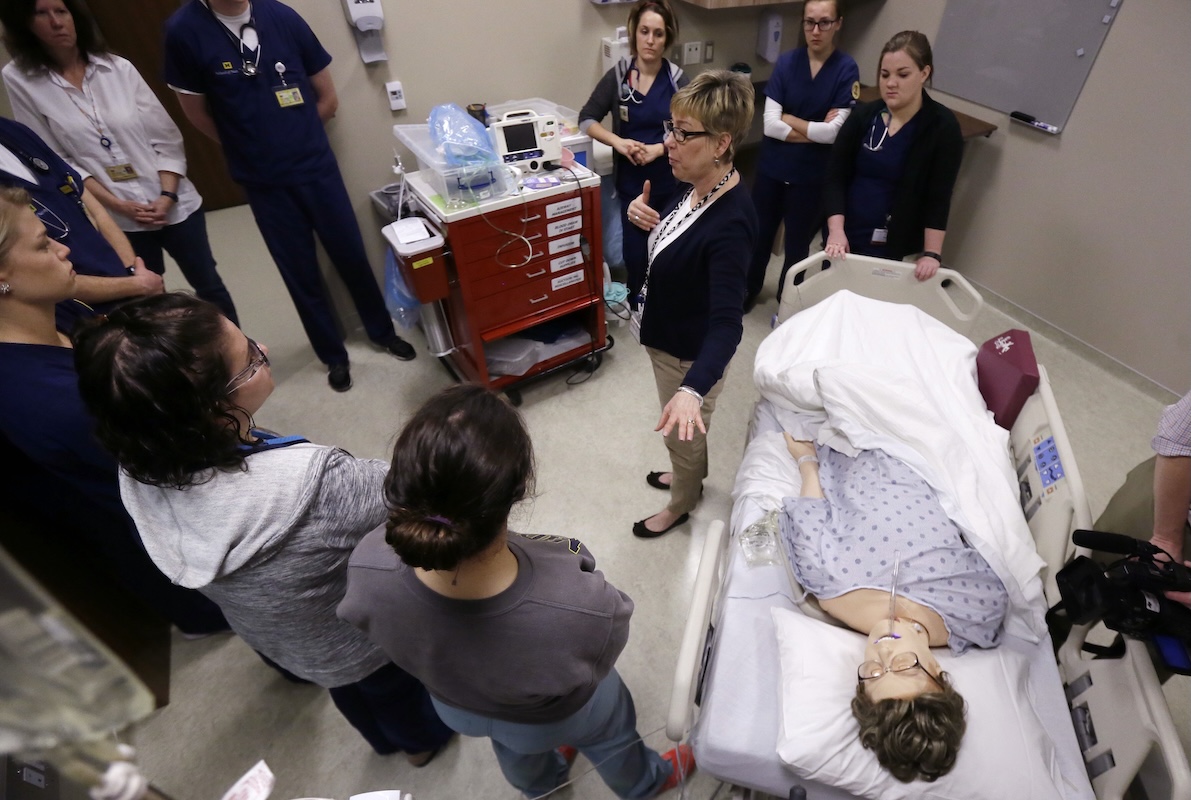
STUDENT. THAT’S RIGHT. AND THE STUDENT WORRIES ABOUT LOANS AND PAYING FOR HER EDUCATION. UNIVERSITY OF MARYLAND, BALTIMORE ADMINISTRATORS SAY TO THE STUDENTS, CONTINUE TO PURSUE YOUR DREAMS. HE HAS NO ALLERGIES TO THIS MEDICATION. IN THIS CLINICAL SITUATION, LAB STUDENTS AT THE UNIVERSITY OF MARYLAND NURSING SCHOOL IN BALTIMORE ARE PRACTICING AND GAINING CONFIDENCE IN THEIR SKILLS TO CARE FOR PATIENTS. OTHER STUDENTS ARE GIVING THEIR END OF SEMESTER PRESENTATIONS. SOME NURSES WHO HAVE COME BACK TO SCHOOL FOR MORE PROFESSIONAL TRAINING ARE WORRIED ABOUT NEWS. THE U.S. DEPARTMENT OF EDUCATION IS CONSIDERING EXCLUDING NURSING FROM ITS DEFINITION OF PROFESSIONAL DEGREE PROGRAMS. IT’S PRETTY UPSETTING FOR, I THINK, A LOT OF US. JAMIE CUTLER HAS BEEN A NURSE FOR FOUR AND A HALF YEARS. SHE IS NOW STUDYING TO GET HER DOCTORATE DEGREE IN NURSING. THEY SAW US AS FRONTLINE WORKERS ABOUT FIVE YEARS AGO. WE WERE ESSENTIAL IN THE COVID PANDEMIC, AND NOW THEY’RE SAYING THAT WE’RE NOT ESSENTIAL AND THAT THEY DON’T WANT TO LOAN US MONEY TO GET OUR DEGREES AND ENHANCE OURSELVES. UNIVERSITY OF MARYLAND. BALTIMORE’S TAKE ON THE PROPOSAL. IT WAS SHOCKING, BUT IT WASN’T COMPLETELY UNEXPECTED BECAUSE WE HAVE BEEN TRACKING THIS ISSUE. THE PROVOST SAYS THIS WILL IMPACT STUDENTS AND HEALTH CARE. WE WANT TO ATTRACT STUDENTS FROM A VARIETY OF SOCIOECONOMIC BACKGROUNDS SO THAT THEY COULD GO OUT AND BE PRACTITIONERS IN THEIR COMMUNITIES, INCLUDING IN RURAL COMMUNITIES. AND SO THE DIRECT IMPACT OF THIS, IT MAKES THESE PROGRAMS LESS, LESS ACCESSIBLE. WHAT ARE ADMINISTRATORS TELLING STUDENTS? WE’VE GOT YOU AND WILL CONTINUE TO WORK HARD TO MAKE SURE THAT, NOTWITHSTANDING THE POLICY AND THE CHALLENGES THAT WE CONTINUE TO WORK TOWARDS OUR MISSION, WHICH IS TO IMPROVE THE HUMAN CONDITION. THE FINAL DECISION IS SET FOR JULY 2026. UNIVERSITY’S NURSING AND OTHER ORGANIZATIONS ARE NOT GIVING UP. THEY ARE TRYING TO GET THE DEPARTMENT OF EDUCATION TO RECONSIDER. REPORTING LIVE FROM DOWNTOWN
Lawmakers urge Education Department to add nursing to ‘professional’ programs list amid uproar
Updated: 1:17 AM EST Dec 12, 2025
A bipartisan group in Congress is urging the Education Department to add nursing to a list of college programs that are considered “professional,” adding to public outcry after nurses were omitted from a new agency definition.The Trump administration’s list of professional programs includes medicine, law and theology but leaves out nursing and some other fields that industry groups had asked to be included. The “professional” label would allow students to borrow larger amounts of federal loans to pursue graduate degrees in those fields.Video above: Nursing students concerned over possible loss of federal student loan accessUnder new rules proposed by the Trump administration, students in graduate programs deemed professional could borrow up to $200,000 for their degrees in total, and up to $50,000 a year. Loans for other graduate programs would be capped at $100,000 in total and $20,500 per year.In the past, graduate students had been able to borrow federal loans up to the full cost of their programs.In a Friday letter, lawmakers argue that a $100,000 cap on nursing graduate programs would make it harder for students to pay for expensive but high-demand programs, like those for nurse anesthetists. The annual cap would also pinch students in year-round nurse practitioner programs, which charge for three terms a year rather than just two and often cost more than $20,500 a year, they wrote.The letter challenges the Education Department’s claim that few nursing students would be affected by the caps.Programs for certified nurse anesthetists can cost more than $200,000, lawmakers said, but the programs typically pay off and supply a workforce that “overwhelmingly provides anesthesia to rural and underserved communities where higher cost physicians do not practice.”Video below: Massachusetts hospitals cut vacancies but critical staffing gaps persist, report saysThe letter was signed by more than 140 lawmakers, including 12 Republicans. It was sent by Sen. Jeff Merkley, D-Ore., Sen. Roger Wicker, R-Miss., Rep. Suzanne Bonamici, D-Ore., and Rep. Jen Kiggans, R-Va., leaders of the Senate and House nursing caucuses.Another Democrat, Rep. Ritchie Torres of New York, sent a similar letter this week. Excluding nurses would require students to take out riskier private loans or put tuition out of reach entirely, said Torres, who represents the South Bronx.”A restrictive interpretation would undermine our healthcare and education systems, weaken our workforce, and close doors for low-income, first-generation, and immigrant students who make up much of my district,” Torres said.The Trump administration has said new loan caps are needed to pressure colleges to reduce tuition prices.In deciding what would count as a professional degree, the department relied on a 1965 law governing student financial aid. The law lays out several examples of professional programs but says it is not an exhaustive list. The Trump administration adopted those examples as the only fields in its definition.Those deemed professional are: pharmacy, dentistry, veterinary medicine, chiropractic, law, medicine, optometry, osteopathic medicine, podiatry, theology and clinical psychology.The definition drew blowback from nursing organizations and other industry groups that were left out, including physical therapists and social workers. Department officials have said the new proposal may change as it’s finalized in a federal rulemaking process.
A bipartisan group in Congress is urging the Education Department to add nursing to a list of college programs that are considered “professional,” adding to public outcry after nurses were omitted from a new agency definition.
The Trump administration’s list of professional programs includes medicine, law and theology but leaves out nursing and some other fields that industry groups had asked to be included. The “professional” label would allow students to borrow larger amounts of federal loans to pursue graduate degrees in those fields.
Video above: Nursing students concerned over possible loss of federal student loan access
Under new rules proposed by the Trump administration, students in graduate programs deemed professional could borrow up to $200,000 for their degrees in total, and up to $50,000 a year. Loans for other graduate programs would be capped at $100,000 in total and $20,500 per year.
In the past, graduate students had been able to borrow federal loans up to the full cost of their programs.
In a Friday letter, lawmakers argue that a $100,000 cap on nursing graduate programs would make it harder for students to pay for expensive but high-demand programs, like those for nurse anesthetists. The annual cap would also pinch students in year-round nurse practitioner programs, which charge for three terms a year rather than just two and often cost more than $20,500 a year, they wrote.
The letter challenges the Education Department’s claim that few nursing students would be affected by the caps.
Programs for certified nurse anesthetists can cost more than $200,000, lawmakers said, but the programs typically pay off and supply a workforce that “overwhelmingly provides anesthesia to rural and underserved communities where higher cost physicians do not practice.”
Video below: Massachusetts hospitals cut vacancies but critical staffing gaps persist, report says
The letter was signed by more than 140 lawmakers, including 12 Republicans. It was sent by Sen. Jeff Merkley, D-Ore., Sen. Roger Wicker, R-Miss., Rep. Suzanne Bonamici, D-Ore., and Rep. Jen Kiggans, R-Va., leaders of the Senate and House nursing caucuses.
Another Democrat, Rep. Ritchie Torres of New York, sent a similar letter this week. Excluding nurses would require students to take out riskier private loans or put tuition out of reach entirely, said Torres, who represents the South Bronx.
“A restrictive interpretation would undermine our healthcare and education systems, weaken our workforce, and close doors for low-income, first-generation, and immigrant students who make up much of my district,” Torres said.
The Trump administration has said new loan caps are needed to pressure colleges to reduce tuition prices.
In deciding what would count as a professional degree, the department relied on a 1965 law governing student financial aid. The law lays out several examples of professional programs but says it is not an exhaustive list. The Trump administration adopted those examples as the only fields in its definition.
Those deemed professional are: pharmacy, dentistry, veterinary medicine, chiropractic, law, medicine, optometry, osteopathic medicine, podiatry, theology and clinical psychology.
The definition drew blowback from nursing organizations and other industry groups that were left out, including physical therapists and social workers. Department officials have said the new proposal may change as it’s finalized in a federal rulemaking process.