[ad_1]
The public health numbers were cause for celebration: U.S. overdose deaths fell for a second year in a row.
After two decades of rising deaths, fatal overdoses killed 21.4% fewer people from August 2024 to 2025 than the year prior, the U.S. government reported in January.
White House spokesperson Anna Kelly attributed the decline to President Donald Trump’s policies at the southern border, military strikes on alleged drug vessels in the Caribbean Sea and Pacific Ocean, and Trump’s work to stop chemicals used to make fentanyl from being imported from China.
A year prior, the Biden administration gave different reasons for the start of the overdose deaths decline, describing its work to distribute more of the opioid-overdose reversing drug naloxone, increase access to addiction treatment medications and support of harm reduction programs.
The short answer for why drug overdose deaths are falling nationally: It’s a lot of reasons.
Experts on overdoses and drug markets told us that no single intervention can fully explain the significant drop. It might have more to do with the drug supply than public health interventions meant to reduce overdoses.
Rising overdose deaths are “a complex societal problem requiring a multitude of solutions,” said Regina LaBelle, a Georgetown University professor of addiction policy. It can also be hard to pin down what works when research on the solutions is sometimes hindered by stigma about drug use, she said.
Here are what some of the researchers say is likely contributing to the measured declines.
Lummi Nation crisis outreach supervisor Evelyn Jefferson looks down at her shirt as she stands at the grave of her son, who died due to an overdose of street drugs containing the synthetic opioid carfentanil, at the Lummi Nation cemetery on tribal reservation lands, Feb. 8, 2024, near Bellingham, Wash. Jefferson had to wait a week to bury her son due to several other overdose deaths in the community. (AP)
There’s less fentanyl in the U.S. drug supply
Fentanyl became less available in the U.S. in 2023, researchers wrote in the journal Science in January.
The synthetic opioid is a leading cause of overdose deaths in both the U.S. and Canada. Experts on illicit drug markets say that illegal fentanyl in both countries stems from precursor chemicals imported from China.
Although the Chinese government often obscures its actions, its official statements show that in late 2023 China began taking action against manufacturers of fentanyl precursor chemicals, the Science study said. The crackdown partly followed Biden administration pressure to take action against fentanyl.
Peter Reuter, a University of Maryland public policy and criminology professor and one of the study’s authors, said the purity of fentanyl seized by the Drug Enforcement Administration began to decrease around the same time as overdose deaths started to decline in the U.S. and Canada in 2023.
“It’s very likely that (the change in purity) has something to do with precursor supply, because that’s what the two markets share,” Reuter said.

David Guthrie, a senior research chemist at the Drug Enforcement Administration, stands near chemical precursors that can be used in the manufacture of fentanyl at a DEA research laboratory on Tuesday, April 29, 2025, in Northern Virginia. (AP)
The pool of people at risk of overdosing may have gotten smaller
Several factors might help explain why fewer people are at risk of overdosing.
These factors include the fact that more people are aware of opioids’ risks, CDC overdose prevention researchers wrote.
Additionally, many people who were once at the highest risk for overdose have already died of overdoses, CDC researchers said.
Opioid sales and prescriptions are also declining, which means fewer people are misusing opioids or developing opioid use disorder.
A JAMA Psychiatry study also pointed out that even though public health interventions meant to prevent overdose deaths are uneven, overdose deaths decreased nationally.

Jonathan Dumke, a senior forensic chemist with the Drug Enforcement Administration, holds vials of fentanyl pills at a DEA research laboratory on Tuesday, April 29, 2025, in Northern Virginia. (AP)
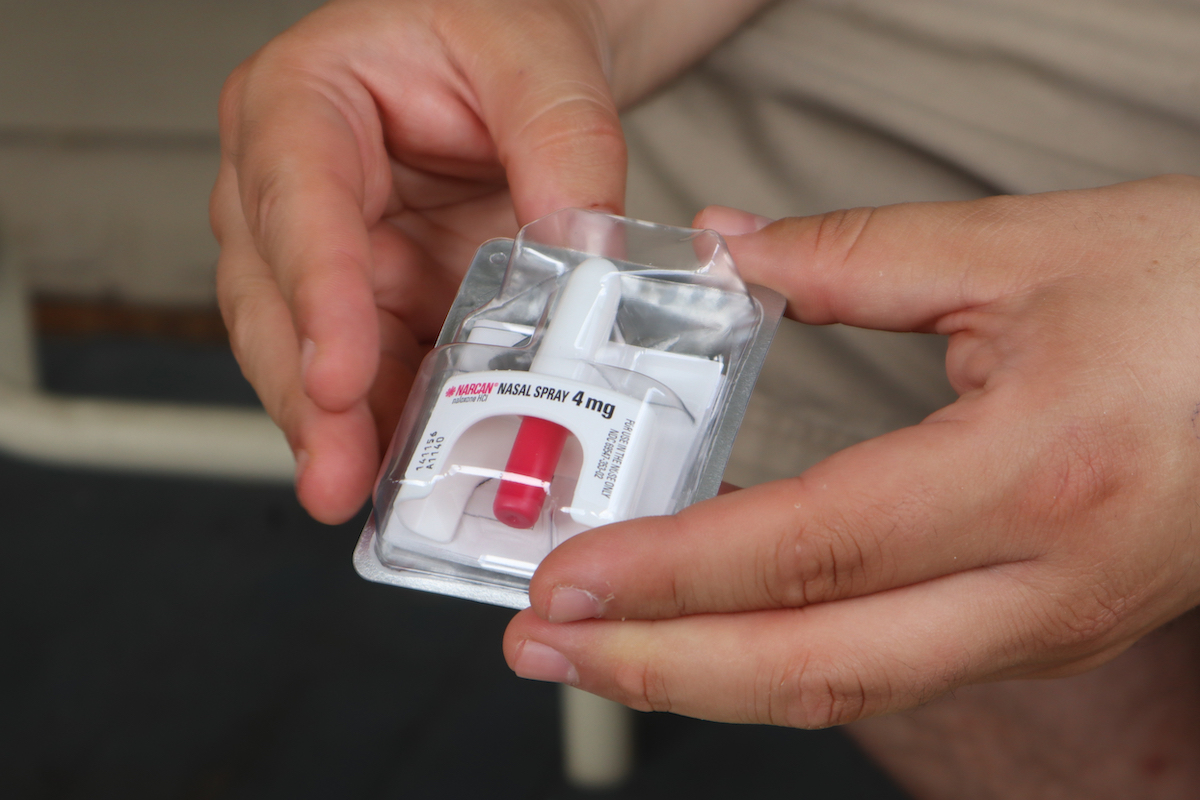
Overdose-reversing naloxone is increasingly available
Experts on drug use and addiction policy also attributed the decline in overdose deaths to the increased availability of naloxone, also known as Narcan.
April Rovero, National Coalition Against Prescription Drug Abuse founder and executive director, said her organization provides education on prescription drug safety and simultaneously distributes naloxone kits that include fentanyl test strips.
“When we train (people), we say, ‘Okay, if you save a life with this kit, you need to let us know,’” Rovero said. “We’ve had a number of those call backs or email messages letting us know that our kit saved literally a life.”
Joe Solomon, co-director of Charleston-based Solutions Oriented Addiction Response, holds a dose of the opioid overdose reversal drug Narcan in Charleston, W.Va., on Sept. 6, 2022. (AP)
From 2014 to 2024, the number of naloxone products dispensed from pharmacies jumped from about 6,000 to 1.97 million, according to the American Medical Association. Naloxone became available over-the-counter in 2023, but some research showed limited sales.
The National Harm Reduction Coalition’s executive director Laura Guzman emphasized the importance of sending naloxone where it is most beneficial. California’s Naloxone Distribution Project says its kits have reversed more than 407,000 overdoses.
Organizations that used naloxone kits as one aspect of their overall harm reduction programs — programs based around safer drug use, management and abstinence strategies — credited those kits as being responsible for nearly 221,000 California overdose reversals, or about 54%.
Naloxone can also give people more time to consider or pursue addiction treatment.

William Perry, founder of This Must Be The Place, right, gives free naloxone medication to concert goers at the Governors Ball Music Festival on Sunday, June 9, 2025, at Flushing Meadows Corona Park in the Queens borough of New York. (AP)
Access to treatment has improved
Increased treatment availability is another factor experts cited for declines in overdose deaths.
Starting on a medication such as buprenorphine or methadone that treats opioid use disorder can protect people from overdoses.
Several studies show that medication treatments, sometimes referred to as opioid agonist treatment, increase the likelihood a person with opioid use disorder will remain in treatment and reduce their risk of overdose.
Guzman said the availability and access to treatment when someone voluntarily seeks it out is crucial.
“Forcing or mandating treatment will not have the same results,” she said.
Data shows that people forced into treatment involuntarily — such as through a drug court — are more likely to die of an opioid-related overdose or a substance use-related cause than those who entered treatment voluntarily.
“People go in and out of treatment a lot,” Rovero said. Sometimes people relapse after being sober for many years. She said she encourages people to consider addiction “a chronic illness that can be treated successfully.”
Experts said that despite signs of progress, it’s too soon to say if overdose deaths will continue to decline. The federal numbers run through August 2025, because the government shutdown delayed the data. Other available data shows some slight regional overdose rate increases in early 2025.
Ultimately, they recommend a multi-faceted approach toward reducing drug overdose deaths — one that includes public health interventions, overdose education, addiction treatment and efforts to reduce the drug supply.
“Public health research focuses on interventions while criminal justice focuses on disrupting the drug supply and criminalizing drug use,” said Lori Ann Post, a Northwestern University emergency medicine professor who studies overdose deaths. “The solution is somewhere in the middle.”
PolitiFact Researcher Caryn Baird contributed to this report.
RELATED: Fact-checking Donald Trump: Has each boat strike off the coast of Venezuela saved 25,000 lives?
RELATED: The US attacked Venezuelan boats it says are carrying drugs. Is Venezuela sending drugs to the US?
RELATED: Misinformation about fentanyl exposure threatens to undermine overdose response
[ad_2]




















