Most crops are contaminated with fungal mycotoxins, but some foods are worse than others.
Oats can be thought of as “uniquely nutritious.” One route by which they improve human health is by providing prebiotics that “increase the growth of beneficial gut microbiota.” There are all manner of oats, ranging from steel-cut oats to, even better, intact oat groats (their form before being cut), all the way down to highly processed cereals, like Honey Nut Cheerios.
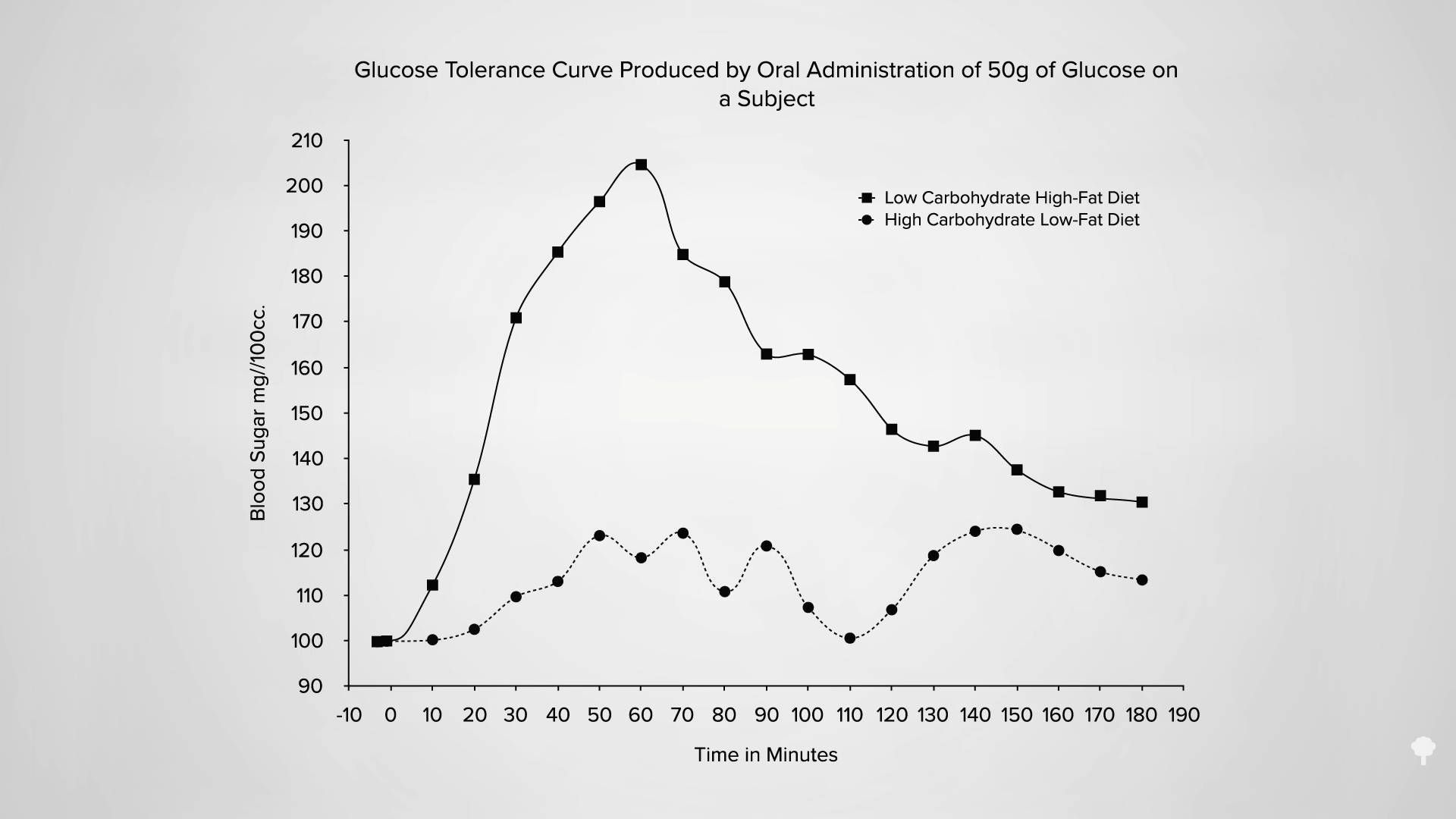
“Rolling crushes the grain, which may disrupt cell walls and damage starch granules, making them more available for digestion.” This is bad because we want the starch to make it all the way down to our colon to feed our good gut bacteria. Grinding oats into oat flour to make breakfast cereals is even worse. When you compare blood sugar and insulin responses, you can see significantly lower spikes with the more intact steel-cut oats, as shown below and at 0:54 in my video Ochratoxin in Certain Herbs, Spices, and Wine.
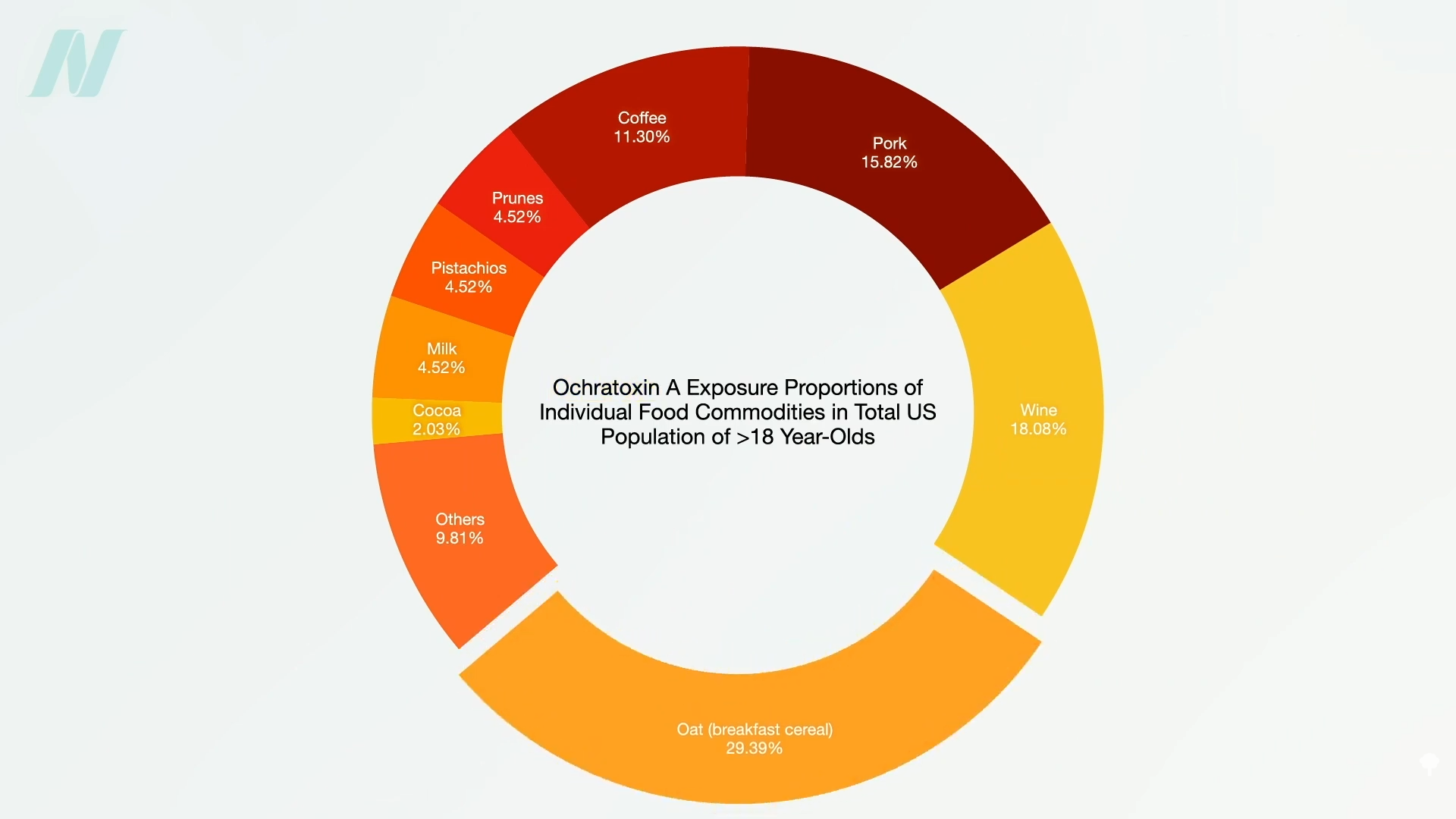
What about ochratoxin? As seen here and at 1:01 in my video, oats are the leading source of dietary exposure to this mold contaminant, but they aren’t the only source.
There is a global contamination of food crops with mycotoxins, with some experts estimating as much as 25% of the world’s crops being affected. That statistic is attributed to the Food and Agriculture Organization of the United Nations, but it turns out the stat is bogus. It isn’t 25%. Instead, it may be more like 60% to 80%. “The high occurrence is likely explained by a combination of the improved sensitivity of analytical [testing] methods and the impact of climate change.”
Spices have been found to have some of the highest concentrations of mycotoxins, but because they are ingested in such small quantities, they aren’t considered to be a significant source. We can certainly do our part to minimize our risk, though. For instance, we should keep spices dry after opening sealed containers or packages.
What about dried herbs? In “Mycotoxins in Plant-Based Dietary Supplements: Hidden Health Risk for Consumers,” researchers found that milk thistle–based supplements had the highest mycotoxin concentrations. It turns out that humid, wet weather is needed during milk thistle harvest, which is evidently why they get so moldy. “Considering the fact that milk thistle preparations are mainly used by people who suffer from liver disease,” such a high intake of compounds toxic to the liver may present some concern.
Wine sourced from the United States also appears to have particularly high levels. In fact, the single highest level found to date around the world is in a U.S. wine, but there’s contamination in wine in general. In fact, some suggest that’s why we see such consistent levels in people’s blood—perhaps because a lot of people are regular wine drinkers.
Ochratoxin is said to be a kidney toxin with immunosuppressive, birth defect–causing, and carcinogenic properties. So, what about ochratoxin decontamination in wine? That is, removing the toxin? Ideally, we’d try to prevent the contamination in the first place, but since this isn’t always practical, there is increased focus on finding effective methods of detoxification of mycotoxins already present in foods. This is where yeast enters as “a promising and friendly solution,” because the mycotoxins bind to the yeast cell wall. The thought is that we could strain out the yeast. Another approach is to eat something like nutritional yeast to prevent the absorption.
It works in chickens. Give yeast along with aflatoxin (another mycotoxin), and the severity of the resulting disease is diminished. However, using something like nutritional yeast as a binder “depends on stability of the yeast-mycotoxin complex through the passage of the gastrointestinal tract.” We know yeasts can remove ochratoxin in foods, but we didn’t have a clue if it would work in the gut until 2016. Yeast was found to bind up to 44% of the ochratoxin, but, in actuality, it was probably closer to only about a third, since some of the bindings weren’t stable. So, if you’re trying to stay under the maximum daily intake and you drink a single glass of wine, even if your bar snack is popcorn seasoned with nutritional yeast, you’d still probably exceed the tolerable intake. But what does that mean? How bad is this ochratoxin? We’ll find out next.
Doctor’s Note
This is the second video in a four-part series on mold toxins. The first one was Ochratoxin in Breakfast Cereals.
Stay tuned for Should We Be Concerned About the Effects of Ochratoxin? and Should We Be Concerned About Aflatoxin?. You can also check: Friday Favorites: Should We Be Concerned About Ochratoxin and Aflatoxin?.
Michael Greger M.D. FACLM
Source link










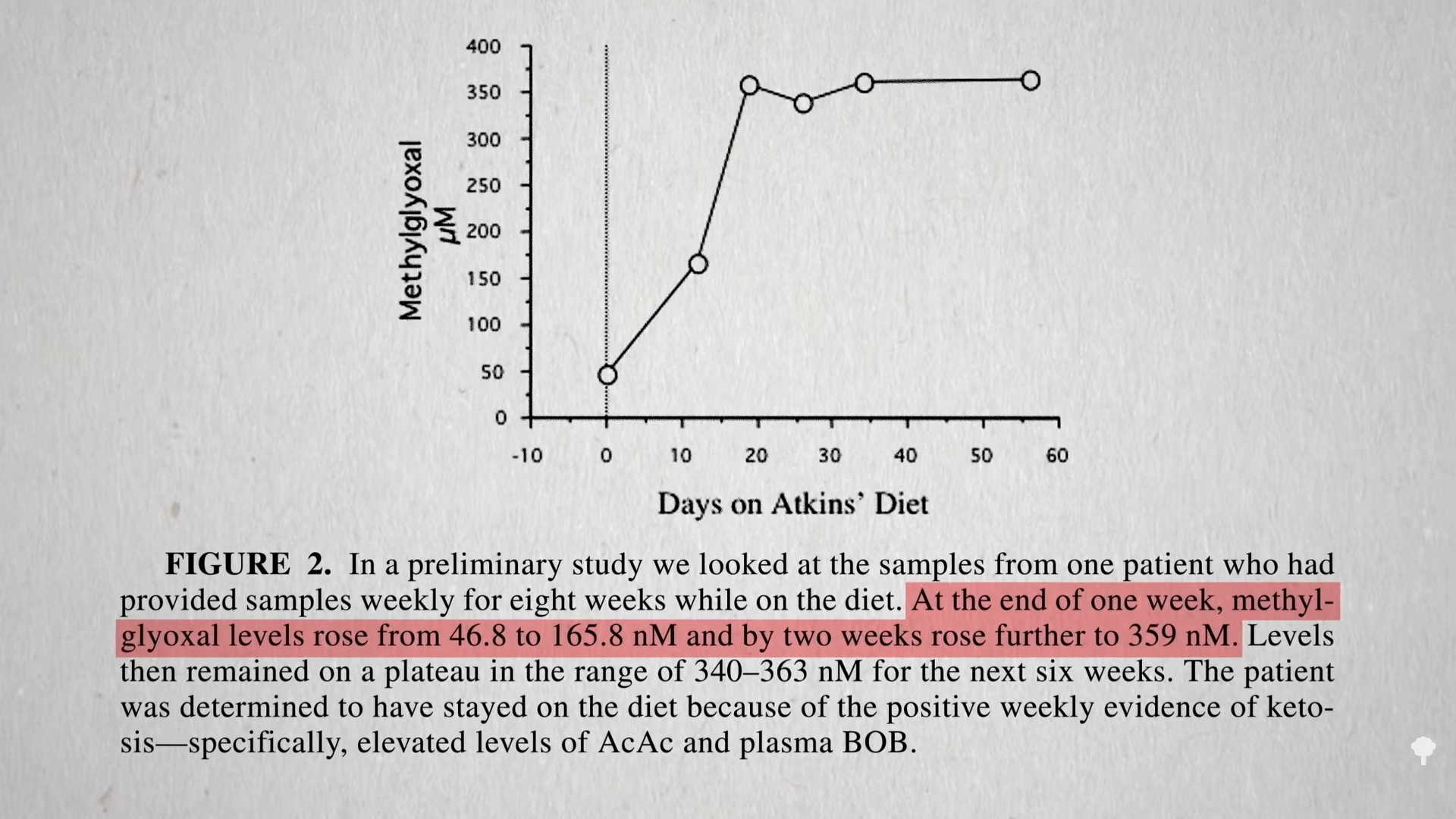
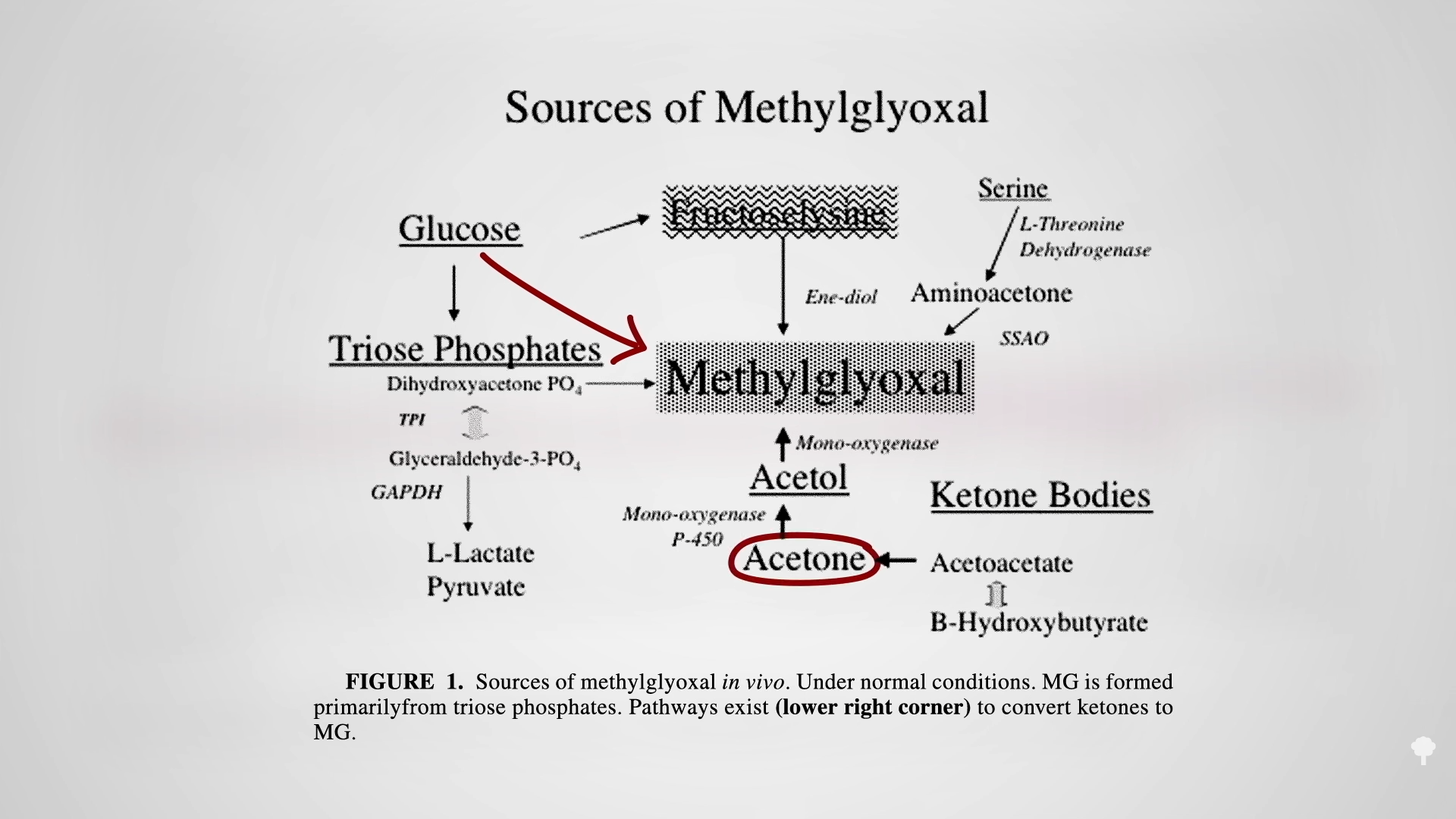
 The irony doesn’t stop there. One of the reasons people with diabetes suffer such nerve and artery damage is due to an inflammatory metabolic toxin known as methylglyoxal, which forms at high blood sugar levels. Methylglyoxal
The irony doesn’t stop there. One of the reasons people with diabetes suffer such nerve and artery damage is due to an inflammatory metabolic toxin known as methylglyoxal, which forms at high blood sugar levels. Methylglyoxal 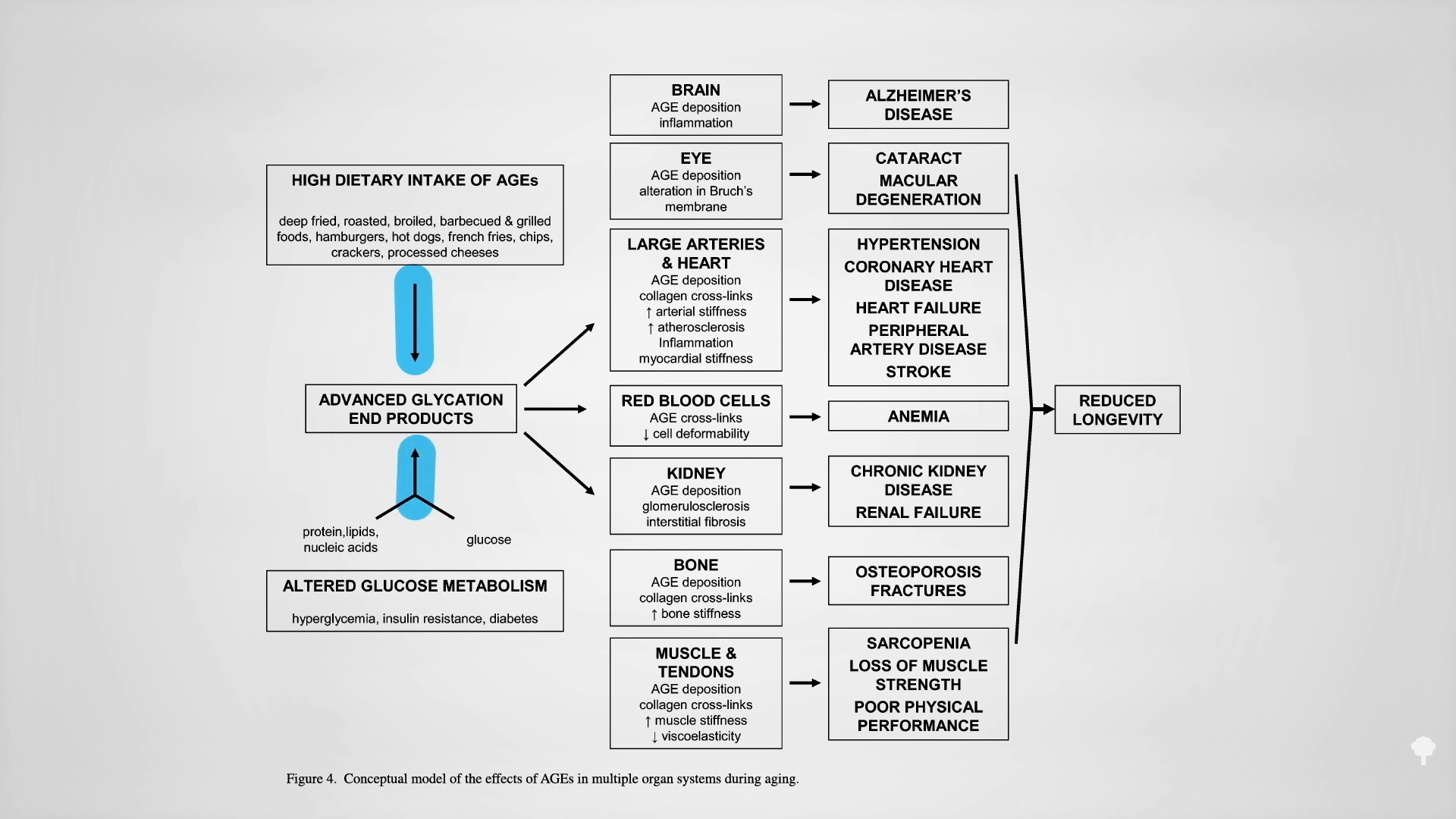



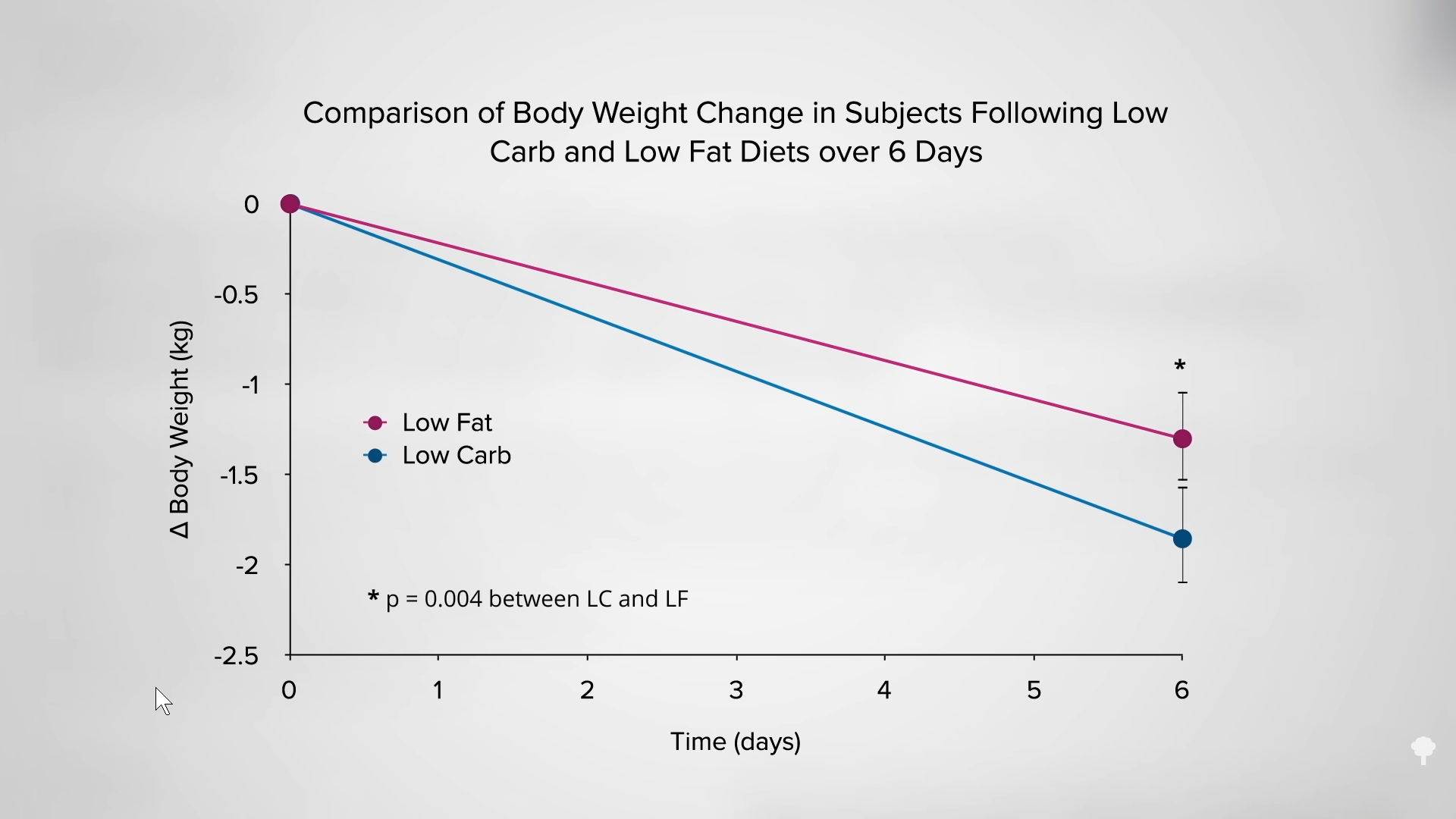
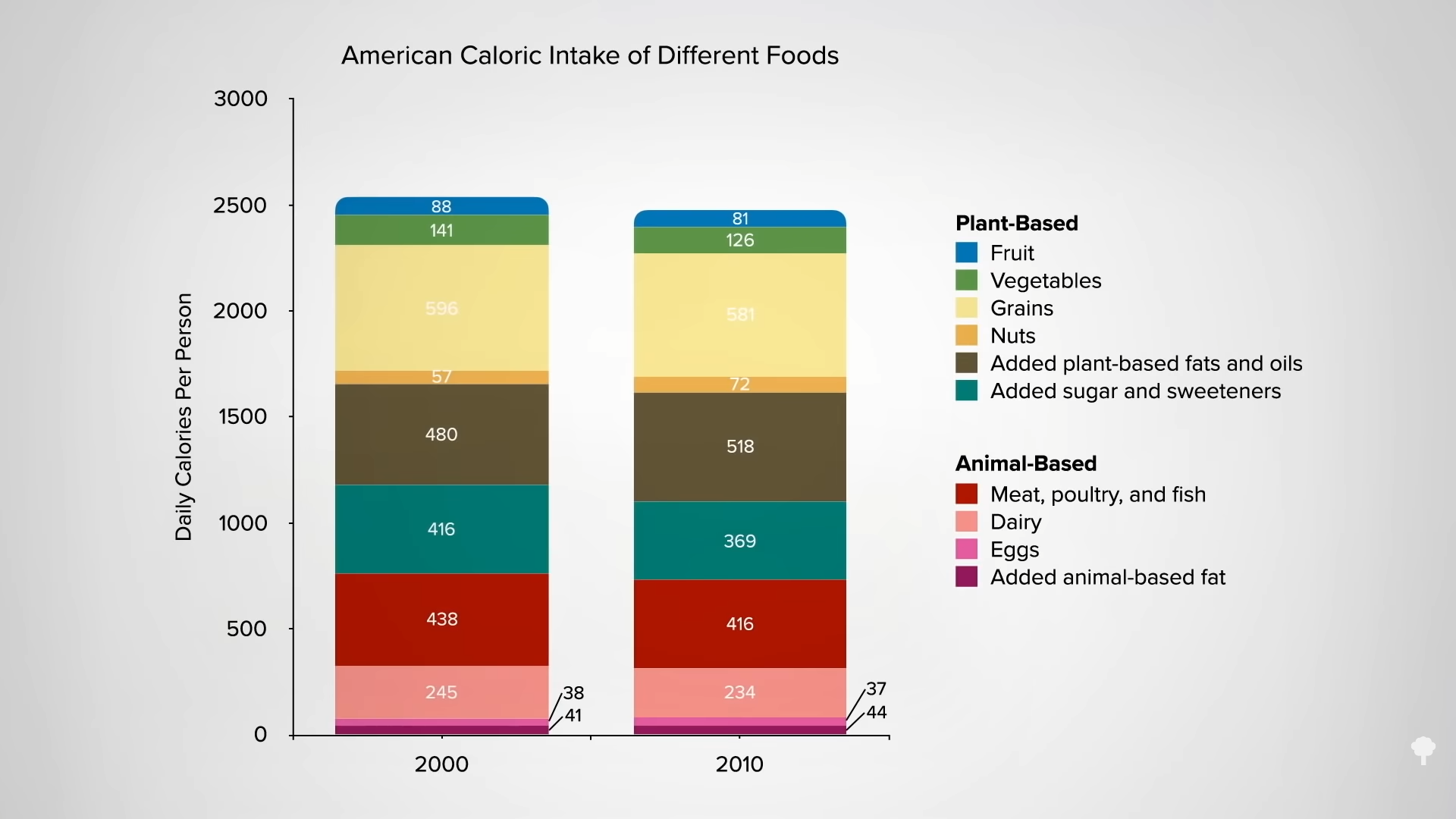 Low-carb diets cut down on refined grains and added sugars, and low-fat diets tend to cut down on added fats and meat, so they both tell people to cut down on donuts. Any diet that does that already has a leg up. I figure a don’t-eat-anything-that-starts-with-the-letter-D diet could also successfully cause weight loss if it caused people to cut down on donuts, danishes, and Doritos, even if it makes no nutritional sense to exclude something like dill.
Low-carb diets cut down on refined grains and added sugars, and low-fat diets tend to cut down on added fats and meat, so they both tell people to cut down on donuts. Any diet that does that already has a leg up. I figure a don’t-eat-anything-that-starts-with-the-letter-D diet could also successfully cause weight loss if it caused people to cut down on donuts, danishes, and Doritos, even if it makes no nutritional sense to exclude something like dill.