Doctors may soon have a new way to treat high blood pressure, even among people for whom medicines haven’t worked well in the past.Baxdrostat, an experimental medicine made by AstraZeneca, showed promise in treating people with uncontrolled or resistant high blood pressure in a recent trial. If the medicine gets approved by regulatory authorities, it will be one of the first new approaches to treating high blood pressure in decades, researchers say.Scientists presented the trial results Saturday at the European Society of Cardiology Congress 2025 in Madrid and simultaneously published them in the New England Journal of Medicine.For the study, researchers enrolled 800 adults who still had high blood pressure after taking two or more medications for at least four weeks. To qualify for the study, patients’ systolic blood pressure had to be between 140 and 170.Blood pressure is measured in millimeters of mercury, which is abbreviated as mm Hg. The measurement has an upper number, or systolic reading, and a lower number, a diastolic reading. Systolic pressure measures the force of blood as it pumps out of the heart into the arteries; diastolic is the pressure created as the heart rests between beats.Normal blood pressure is less than 120/80 mm Hg, and elevated blood pressure is considered to be from 120 to 129/80 mm Hg. At 130/80 mmHg or higher, according to new U.S. guidelines, a person’s medical provider will want them to take a blood pressure medication if lifestyle changes — including eating healthier, reducing salt in the diet and exercising more — don’t work first.The researchers on the new trial placed the participants into three groups. One received 1 milligram of baxdrostat, another got 2 mg, and another got a placebo, which does nothing. Participants took their dose in addition to medicines they were already taking.At 12 weeks, about 4 in 10 patients taking baxdrostat reached healthy blood pressure levels, compared with less than 2 in 10 who got a placebo.Specifically, participants who got 1 or 2 mg of baxdrostat daily saw their systolic blood pressure – the upper number in the reading – fall around 9 to 10 mm Hg more than those taking a placebo. This reduction, studies show, is large enough to cut cardiovascular risk.When blood pressure is high, the force of the blood pushes against the walls of their blood vessels, making the heart less efficient: Both the vessels and the heart must work harder, and it’s more difficult to get blood to essential organs and cells. Without treatment, high blood pressure will eventually damage the arteries, raising the risk of conditions like a heart attack, stroke, coronary disease, vascular dementia and cognitive problems.Heart disease is the No. 1 killer in the world. Lowering blood pressure is the most modifiable way to avoid such a death.Nearly half of all adults in the U.S. have higher than normal blood pressure, and 1 in 10 people have what doctors call resistant hypertension: Despite being on three or more medications, they are not meeting the goal for blood pressure control.When a patient has high blood pressure, doctors may need to try a variety of medications to see what works best.Adding baxdrostat to the list of options could be a big help for patients, according to Dr. Stacey E. Rosen, volunteer president of the American Heart Association, who was not involved with the new research.“What’s interesting about this medication is that they can really be a wonderful partner, so to speak, with some of the more classically recommended anti-hypertensive medications,” said Rosen, who is also a senior vice president of women’s health and executive director of the Katz Institute for Women’s Health of Northwell Health in New York City.Medication options now on the market control blood pressure in a variety of ways. Some, such as vasodilators, relax and widen arteries and veins to allow blood to get through easier and increase flow. Diuretics primarily work by removing excess fluid and salt from the body by increasing urine production. Centrally acting alpha agonists help prevent the nervous system from responding to stress. ACE inhibitors keep the body from producing angiotensin II, a hormone that makes blood vessels constrict. ARBs, or angiotensin II receptor blockers, help reduce the production of aldosterone, a hormone that promotes salt and water retention. Calcium channel blockers can keep calcium away from the cells of the heart and arteries so they don’t have to work as hard.Each can have different side effects, including dizziness, rapid or slower heart rate, exhaustion, upset stomach and swelling in the legs.Baxdrostat’s side effects, the study showed, were mild overall. The most common problem was abnormalities in potassium and sodium levels, but this was rare.Baxdrostat takes a new approach to managing high blood pressure. It focuses on blocking aldosterone, a hormone created by the adrenal glands that helps kidneys regulate salt and maintain the body’s water balance. Some people produce too much aldosterone, leading their body to retain too much water and salt, pushing up blood pressure.“We’ve also known for a while now that most of us eat too much salt and in doing that, it raises blood pressure. But we’re also increasingly recognizing that aldosterone may have a direct impact on causing damage to the blood vessels, to the heart, to the kidneys,” said Dr. Jenifer Brown, one of the lead investigators and co-author of the published study.Brown said she often sees cardiology patients at Brigham and Women’s who may have had a heart event, so she needs to be aggressive in getting their blood pressure under control to prevent another. Some patients may have trouble tolerating other blood pressure medications. For others, the standard medicines just don’t work well. Baxdrostat could be a good complement, she said.“We really have had the same tools as clinicians for many years,” Brown said. “I would be excited to have an option like this.”In an editorial accompanying the publication, Dr. Tomasz Guzik, a cardiovascular scientist at the University of Edinburgh, and Dr. Maciej Tomaszewski, a cardiovascular expert at the University of Manchester, write that next steps should be to figure out which patients would best respond to this new medicine and provide longer-term data. If the medication works long-term, they wrote, it could become a “central piller of therapy for difficult-to-control hypertension.”AstraZeneca said it plans to submit its data to regulatory agencies before the end of 2025.
Doctors may soon have a new way to treat high blood pressure, even among people for whom medicines haven’t worked well in the past.
Baxdrostat, an experimental medicine made by AstraZeneca, showed promise in treating people with uncontrolled or resistant high blood pressure in a recent trial. If the medicine gets approved by regulatory authorities, it will be one of the first new approaches to treating high blood pressure in decades, researchers say.
Scientists presented the trial results Saturday at the European Society of Cardiology Congress 2025 in Madrid and simultaneously published them in the New England Journal of Medicine.
For the study, researchers enrolled 800 adults who still had high blood pressure after taking two or more medications for at least four weeks. To qualify for the study, patients’ systolic blood pressure had to be between 140 and 170.
Blood pressure is measured in millimeters of mercury, which is abbreviated as mm Hg. The measurement has an upper number, or systolic reading, and a lower number, a diastolic reading. Systolic pressure measures the force of blood as it pumps out of the heart into the arteries; diastolic is the pressure created as the heart rests between beats.
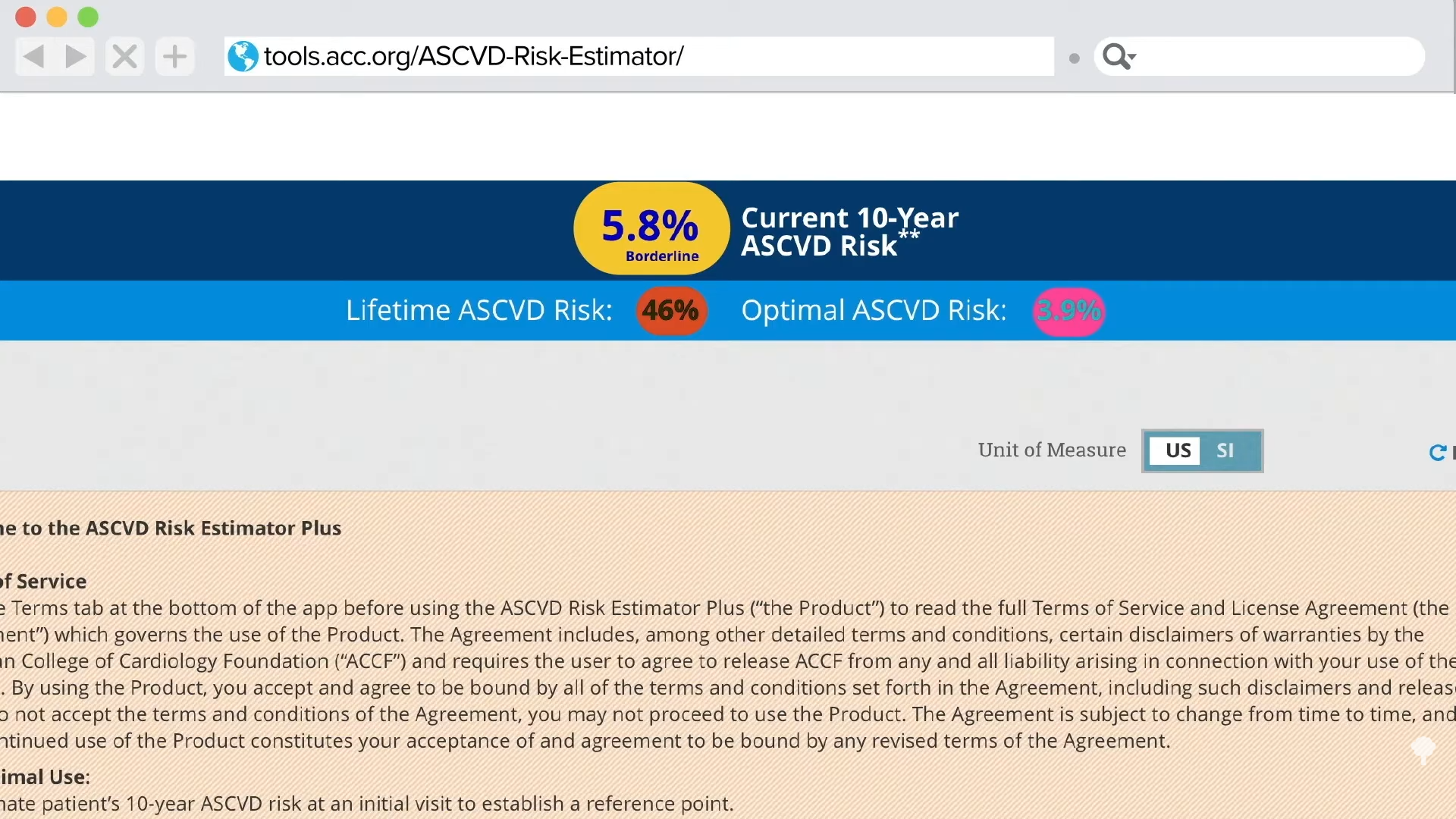
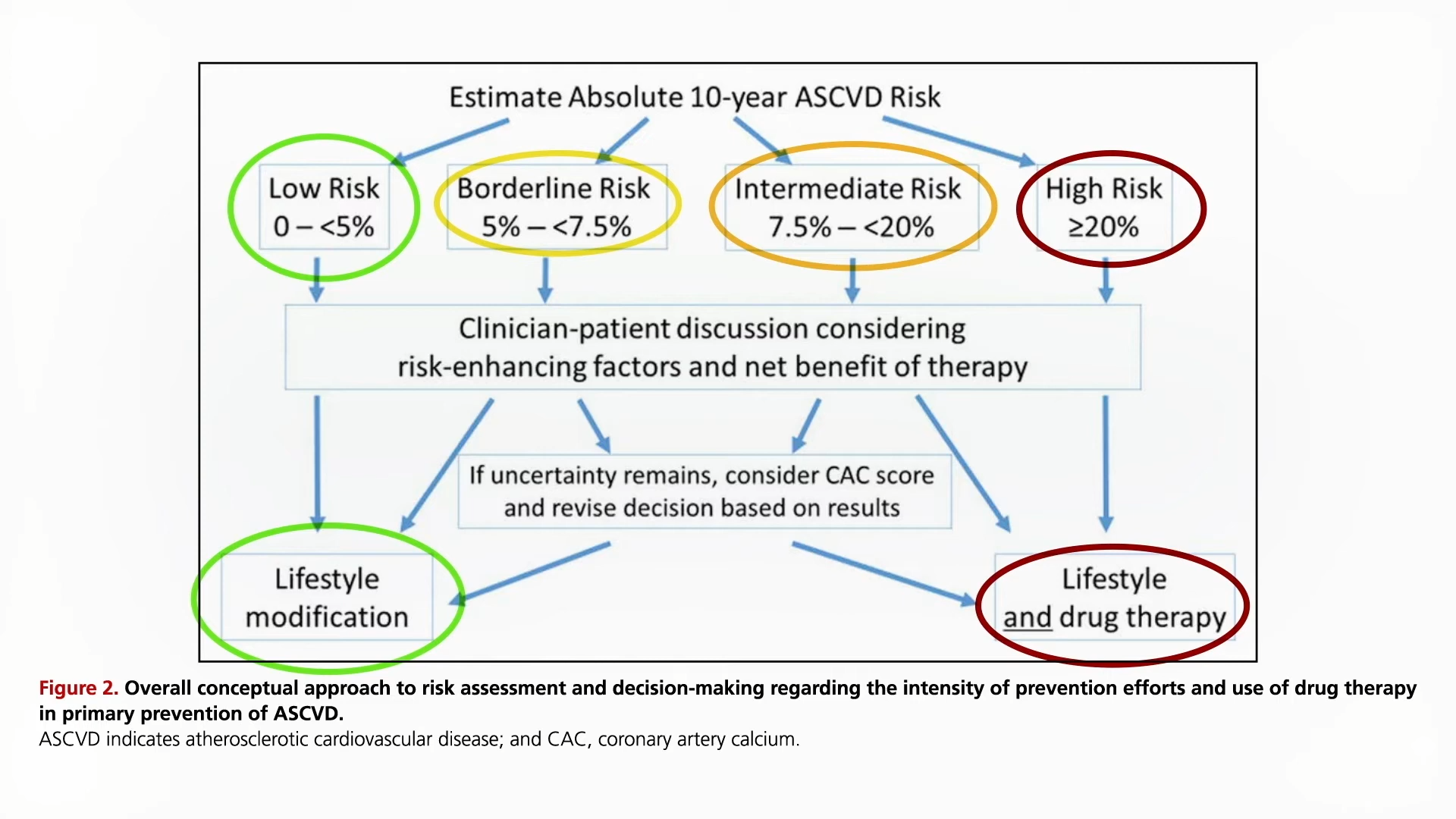
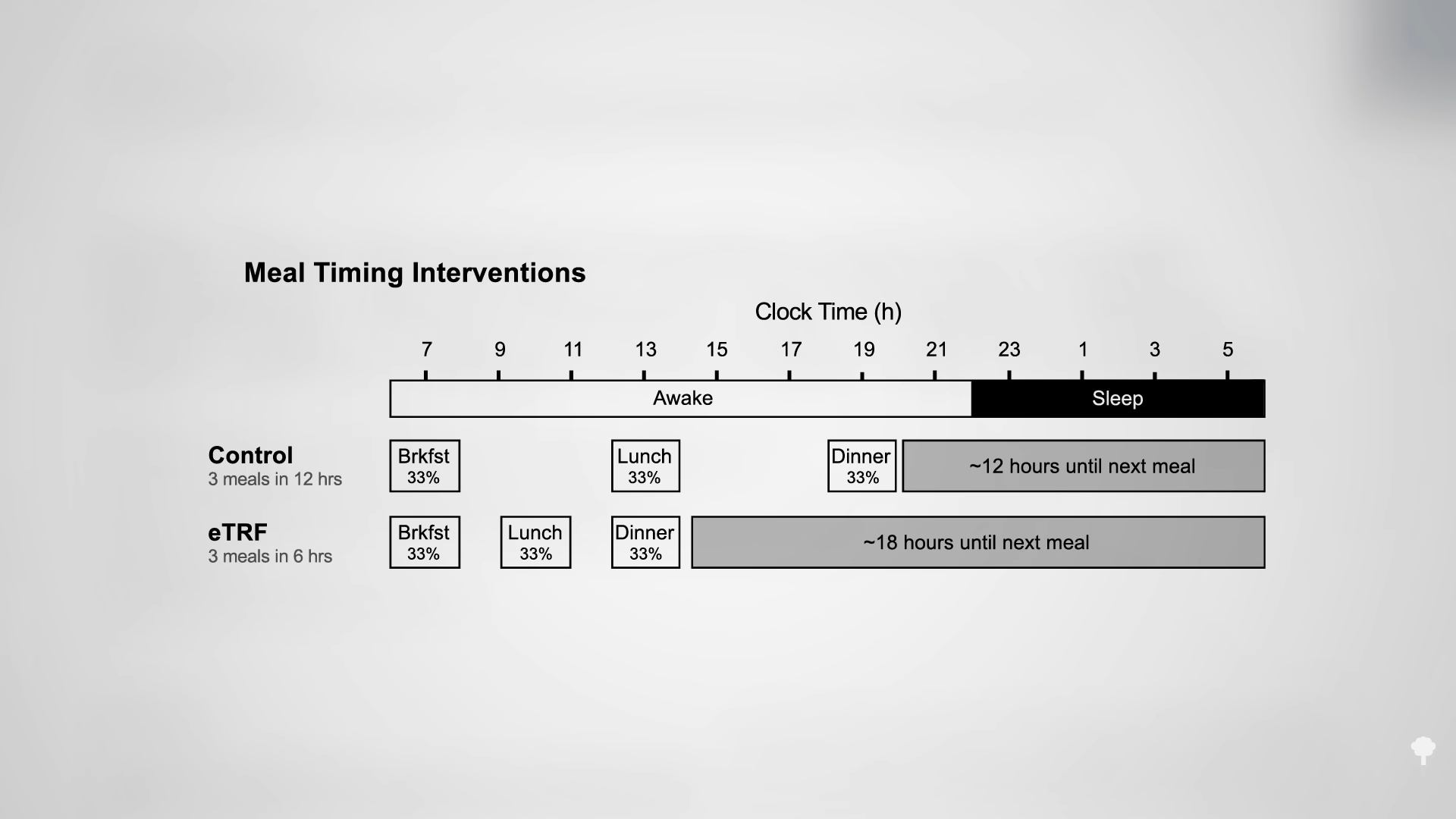
Normal blood pressure is less than 120/80 mm Hg, and elevated blood pressure is considered to be from 120 to 129/80 mm Hg. At 130/80 mmHg or higher, according to new U.S. guidelines, a person’s medical provider will want them to take a blood pressure medication if lifestyle changes — including eating healthier, reducing salt in the diet and exercising more — don’t work first.
The researchers on the new trial placed the participants into three groups. One received 1 milligram of baxdrostat, another got 2 mg, and another got a placebo, which does nothing. Participants took their dose in addition to medicines they were already taking.
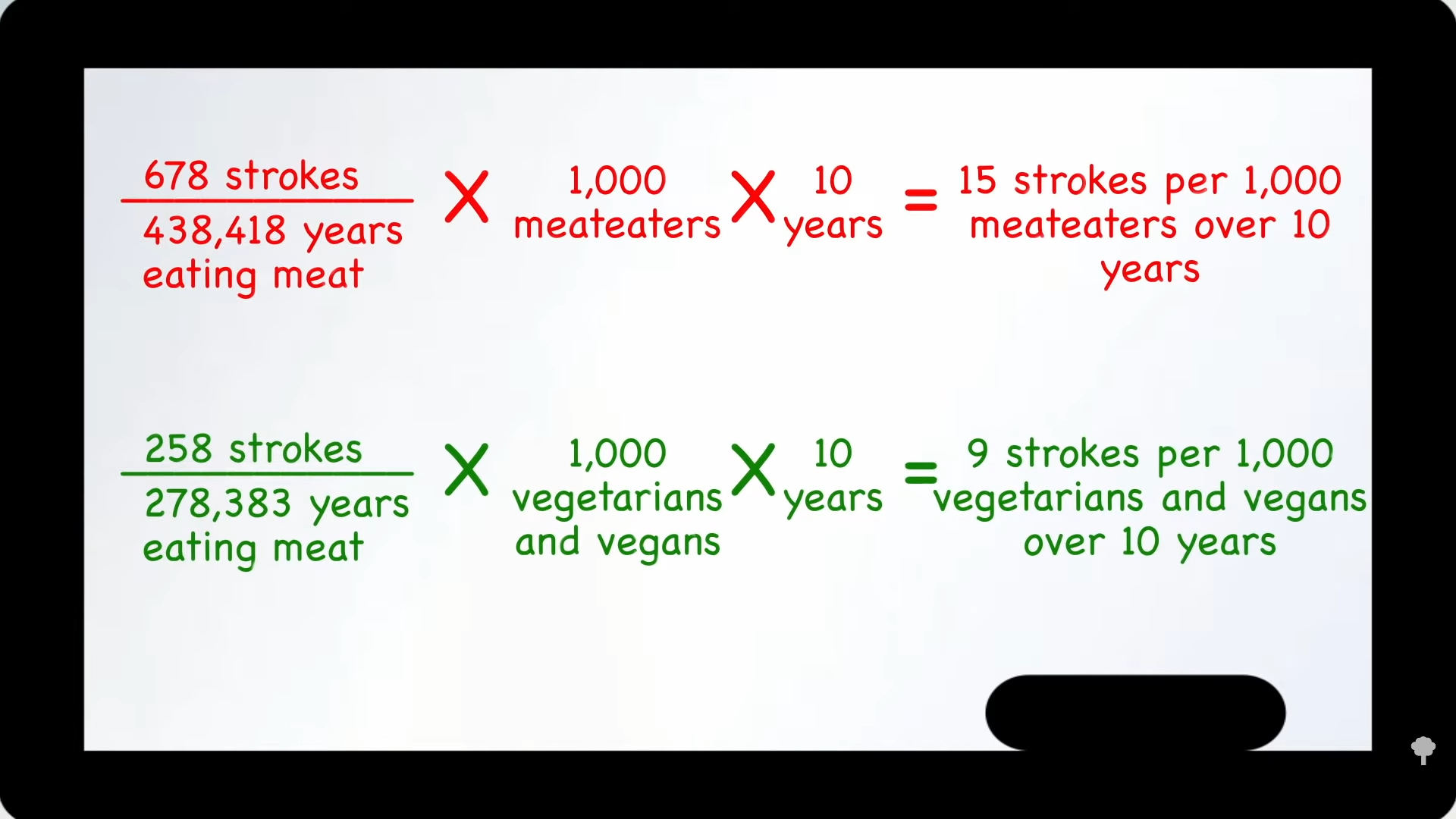
At 12 weeks, about 4 in 10 patients taking baxdrostat reached healthy blood pressure levels, compared with less than 2 in 10 who got a placebo.
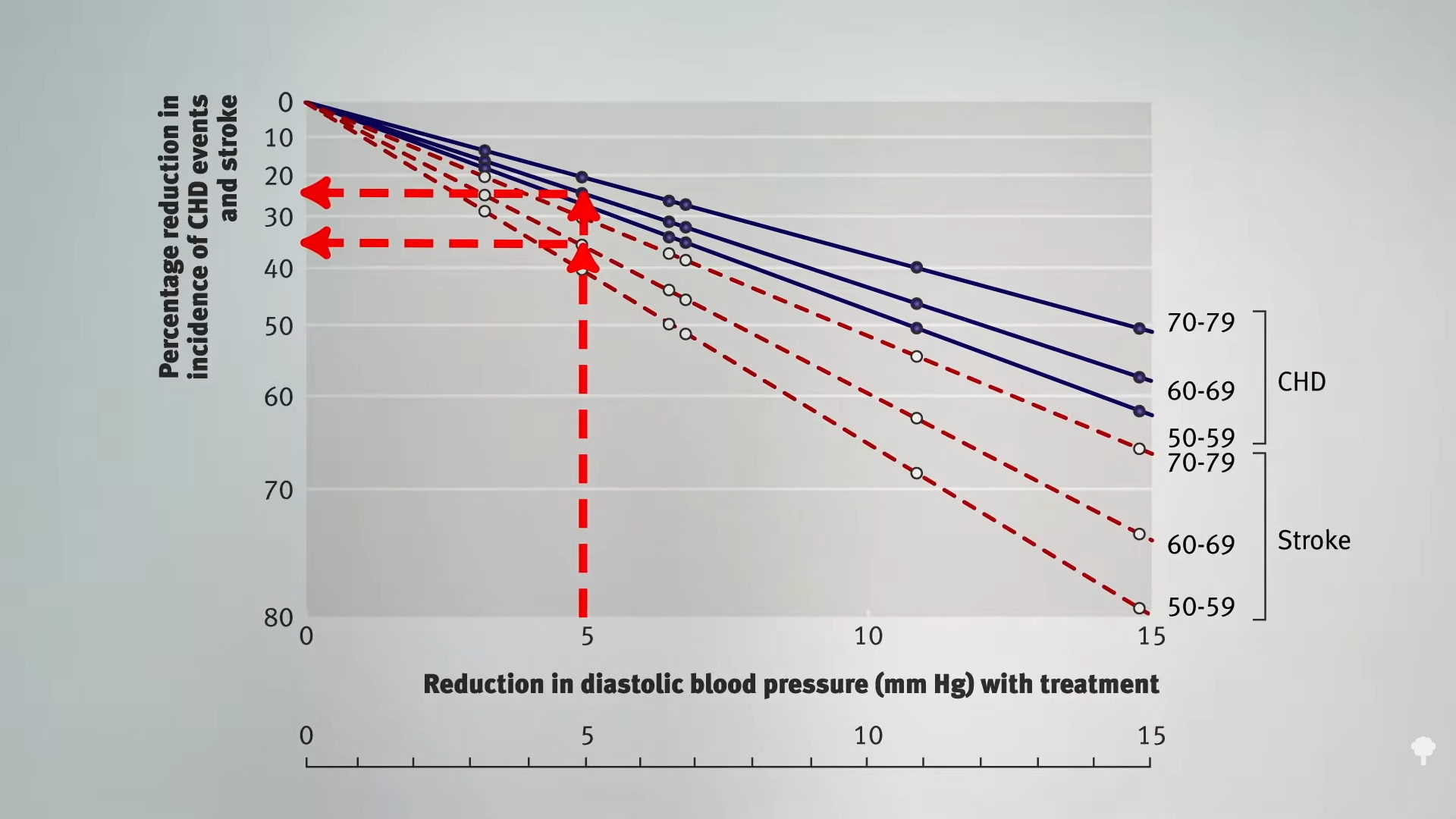
Specifically, participants who got 1 or 2 mg of baxdrostat daily saw their systolic blood pressure – the upper number in the reading – fall around 9 to 10 mm Hg more than those taking a placebo. This reduction, studies show, is large enough to cut cardiovascular risk.
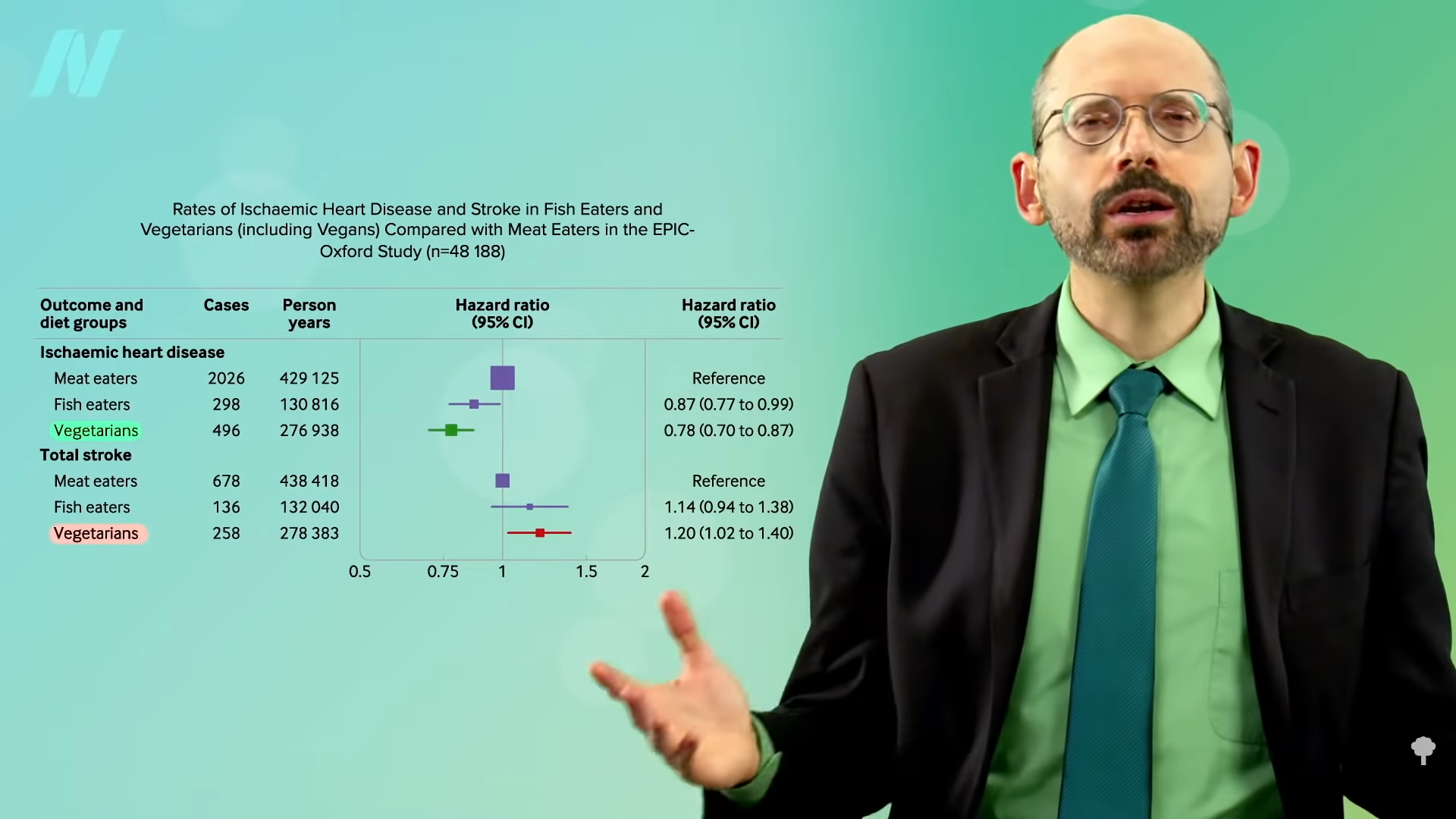
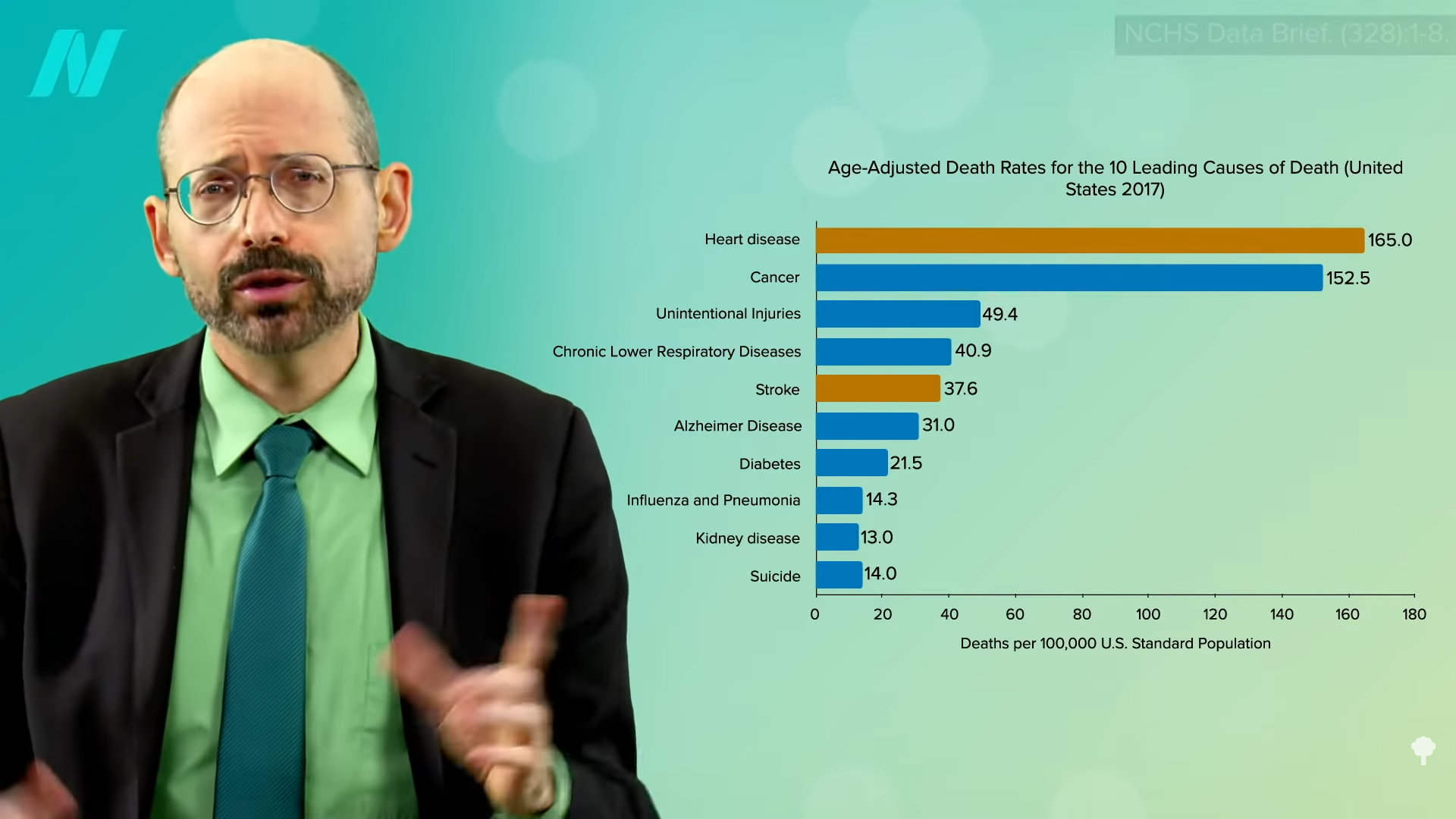
When blood pressure is high, the force of the blood pushes against the walls of their blood vessels, making the heart less efficient: Both the vessels and the heart must work harder, and it’s more difficult to get blood to essential organs and cells. Without treatment, high blood pressure will eventually damage the arteries, raising the risk of conditions like a heart attack, stroke, coronary disease, vascular dementia and cognitive problems.
Heart disease is the No. 1 killer in the world. Lowering blood pressure is the most modifiable way to avoid such a death.
Nearly half of all adults in the U.S. have higher than normal blood pressure, and 1 in 10 people have what doctors call resistant hypertension: Despite being on three or more medications, they are not meeting the goal for blood pressure control.
When a patient has high blood pressure, doctors may need to try a variety of medications to see what works best.
Adding baxdrostat to the list of options could be a big help for patients, according to Dr. Stacey E. Rosen, volunteer president of the American Heart Association, who was not involved with the new research.
“What’s interesting about this medication is that they can really be a wonderful partner, so to speak, with some of the more classically recommended anti-hypertensive medications,” said Rosen, who is also a senior vice president of women’s health and executive director of the Katz Institute for Women’s Health of Northwell Health in New York City.
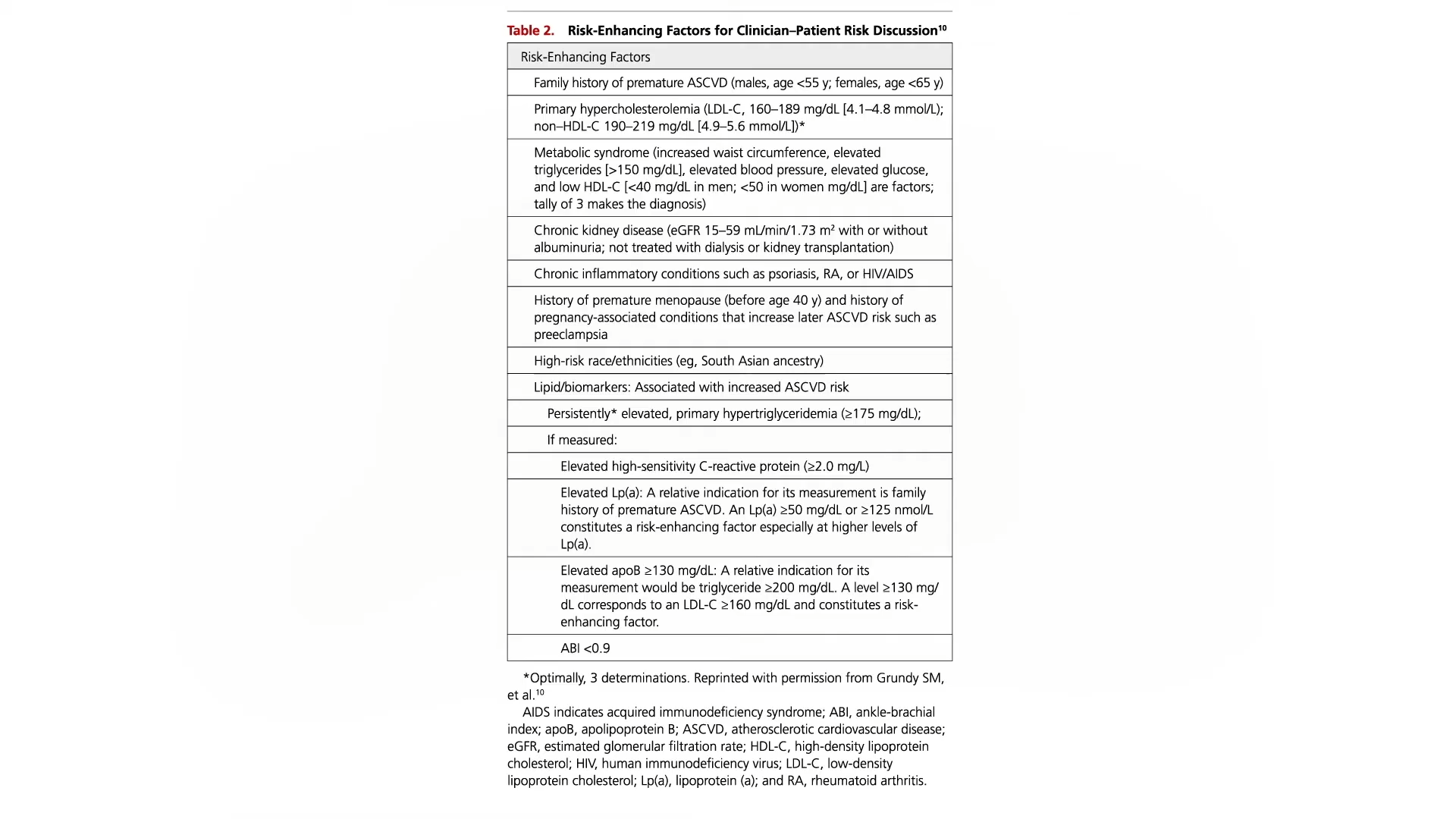
Medication options now on the market control blood pressure in a variety of ways. Some, such as vasodilators, relax and widen arteries and veins to allow blood to get through easier and increase flow. Diuretics primarily work by removing excess fluid and salt from the body by increasing urine production. Centrally acting alpha agonists help prevent the nervous system from responding to stress. ACE inhibitors keep the body from producing angiotensin II, a hormone that makes blood vessels constrict. ARBs, or angiotensin II receptor blockers, help reduce the production of aldosterone, a hormone that promotes salt and water retention. Calcium channel blockers can keep calcium away from the cells of the heart and arteries so they don’t have to work as hard.
Each can have different side effects, including dizziness, rapid or slower heart rate, exhaustion, upset stomach and swelling in the legs.
Baxdrostat’s side effects, the study showed, were mild overall. The most common problem was abnormalities in potassium and sodium levels, but this was rare.
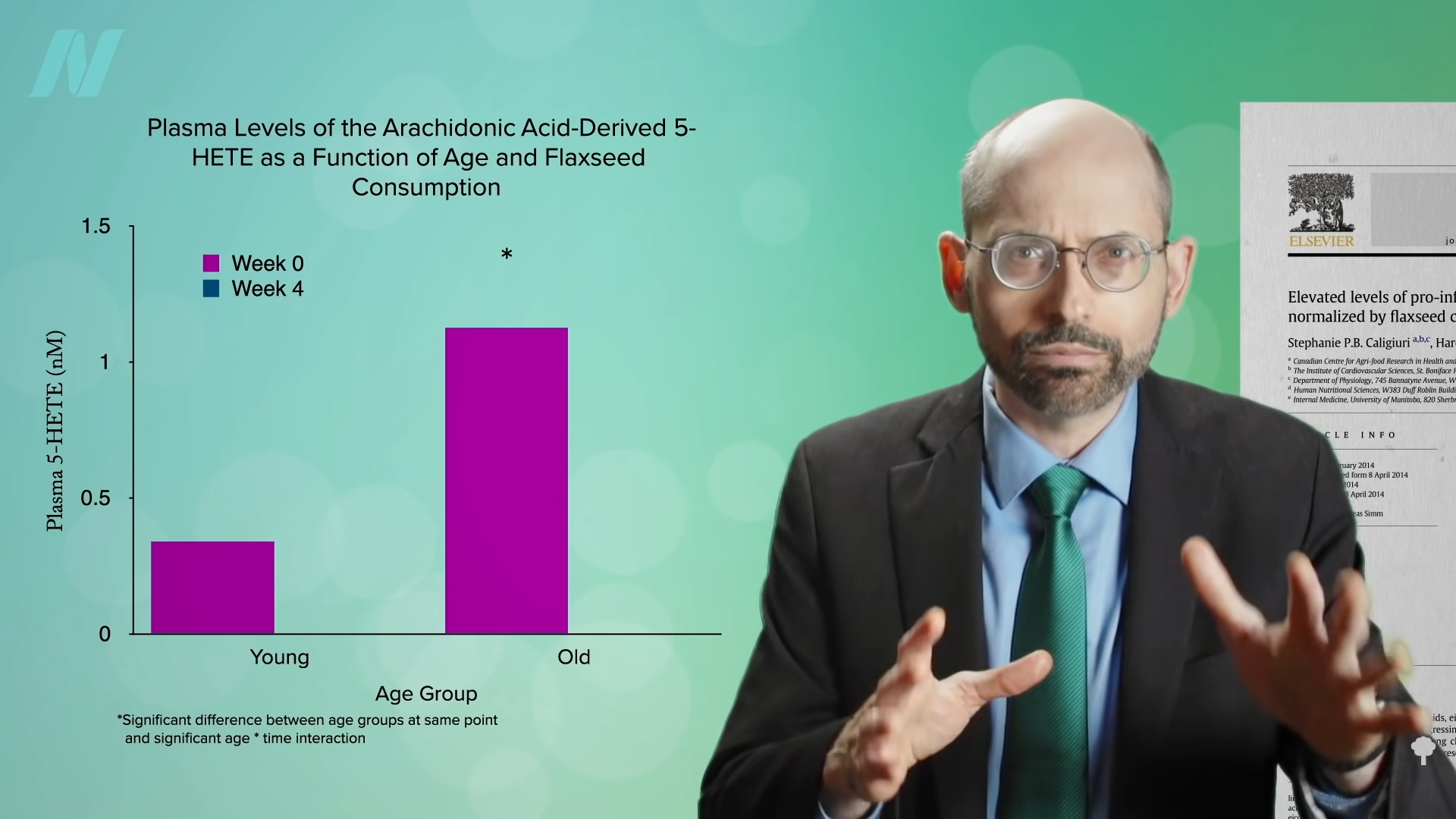
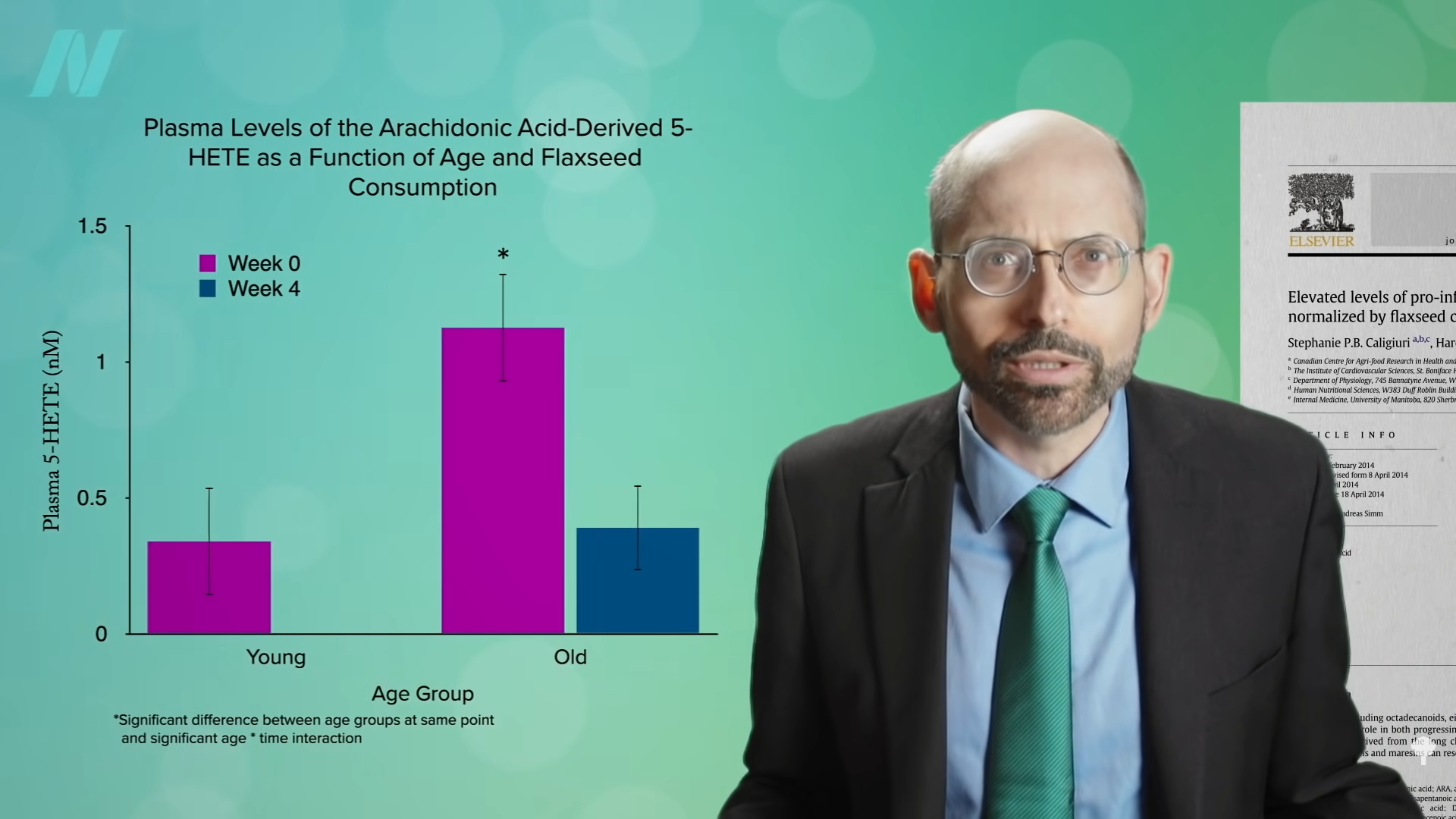
Baxdrostat takes a new approach to managing high blood pressure. It focuses on blocking aldosterone, a hormone created by the adrenal glands that helps kidneys regulate salt and maintain the body’s water balance. Some people produce too much aldosterone, leading their body to retain too much water and salt, pushing up blood pressure.
“We’ve also known for a while now that most of us eat too much salt and in doing that, it raises blood pressure. But we’re also increasingly recognizing that aldosterone may have a direct impact on causing damage to the blood vessels, to the heart, to the kidneys,” said Dr. Jenifer Brown, one of the lead investigators and co-author of the published study.
Brown said she often sees cardiology patients at Brigham and Women’s who may have had a heart event, so she needs to be aggressive in getting their blood pressure under control to prevent another. Some patients may have trouble tolerating other blood pressure medications. For others, the standard medicines just don’t work well. Baxdrostat could be a good complement, she said.
“We really have had the same tools as clinicians for many years,” Brown said. “I would be excited to have an option like this.”
In an editorial accompanying the publication, Dr. Tomasz Guzik, a cardiovascular scientist at the University of Edinburgh, and Dr. Maciej Tomaszewski, a cardiovascular expert at the University of Manchester, write that next steps should be to figure out which patients would best respond to this new medicine and provide longer-term data. If the medication works long-term, they wrote, it could become a “central piller of therapy for difficult-to-control hypertension.”
AstraZeneca said it plans to submit its data to regulatory agencies before the end of 2025.
Source link