As temperatures and humidity soar outside, what’s happening inside the human body can become a life-or-death battle decided by just a few degrees.
The critical danger point outdoors for illness and death from relentless heat is several degrees lower than experts once thought, say researchers who put people in hot boxes to see what happens to them.
With much of the United States, Mexico, India and the Middle East suffering through blistering heat waves, worsened by human-caused climate change, several doctors, physiologists and other experts explained to The Associated Press what happens to the human body in such heat.
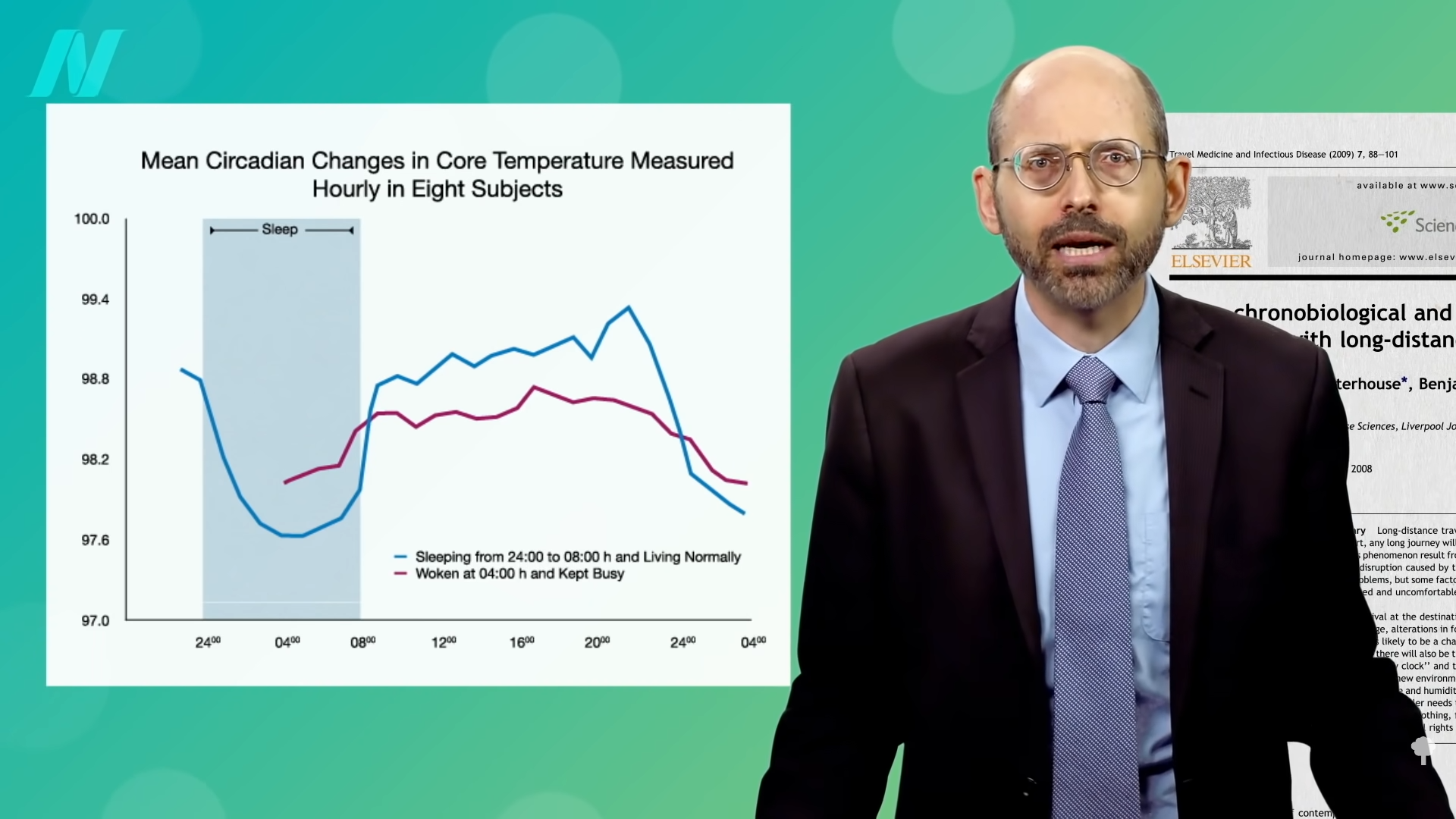
The body’s resting core temperature is typically about 98.6 degrees Fahrenheit (37 degrees Celsius).
That’s only 7 degrees (4 Celsius) away from catastrophe in the form of heatstroke, said Ollie Jay, a professor of heat and health at the University of Sydney in Australia, where he runs the thermoergonomics laboratory.
Dr. Neil Gandhi, emergency medicine director at Houston Methodist Hospital, said during heat waves anyone who comes in with a fever of 102 or higher and no clear source of infection will be looked at for heat exhaustion or the more severe heatstroke.
“We routinely will see core temperatures greater than 104, 105 degrees during some of the heat episodes,” Gandhi said. Another degree or three and such a patient is at high risk of death, he said.
Heat kills in three main ways, Jay said. The usual first suspect is heatstroke — critical increases in body temperature that cause organs to fail.
When inner body temperature gets too hot, the body redirects blood flow toward the skin to cool down, Jay said. But that diverts blood and oxygen away from the stomach and intestines, and can allow toxins normally confined to the gut area to leak into circulation.
“That sets off a cascade of effects,” Jay said. “Clotting around the body and multiple organ failure and, ultimately, death.”
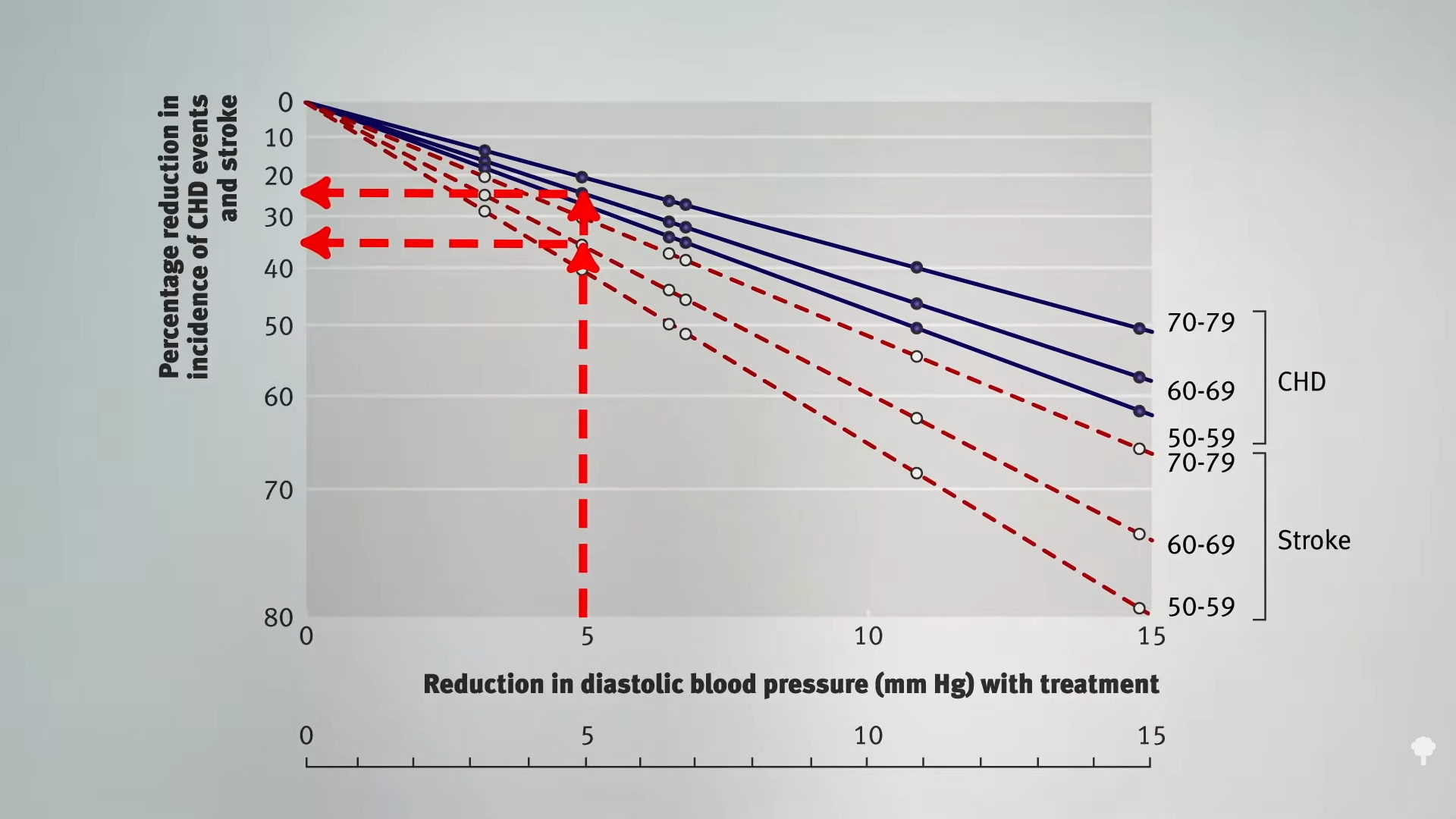
But the bigger killer in heat is the strain on the heart, especially for people who have cardiovascular disease, Jay said.
It again starts with blood rushing to the skin to help shed core heat. That causes blood pressure to drop. The heart responds by trying to pump more blood to keep you from passing out.
“You’re asking the heart to do a lot more work than it usually has to do,” Jay said. For someone with a heart condition “it’s like running for a bus with dodgy (hamstring). Something’s going to give.”
The third main way is dangerous dehydration. As people sweat, they lose liquids to a point that can severely stress kidneys, Jay said.
Many people may not realize their danger, Houston’s Gandhi said.
Dehydration can progress into shock, causing organs to shut down from lack of blood, oxygen and nutrients, leading to seizures and death, said Dr. Renee Salas, a Harvard University professor of public health and an emergency room physician at Massachusetts General Hospital.
“Dehydration can be very dangerous and even deadly for everyone if it gets bad enough — but it is especially dangerous for those with medical conditions and on certain medications,” Salas said.
Dehydration also reduces blood flow and magnifies cardiac problems, Jay said.
Heat also affects the brain. It can cause a person to have confusion, or trouble thinking, several doctors said.
“One of the first symptoms you’re getting into trouble with the heat is if you get confused,” said University of Washington public health and climate professor Kris Ebi. That’s little help as a symptom because the person suffering from the heat is unlikely to recognize it, she said. And it becomes a bigger problem as people age.
One of the classic definitions of heat stroke is a core body temperature of 104 degrees “coupled with cognitive dysfunction,” said Pennsylvania State University physiology professor W. Larry Kenney.
Some scientists use a complicated outside temperature measurement called wet bulb globe temperature, which takes into account humidity, solar radiation and wind. In the past, it was thought that a wet-bulb reading of 95 Fahrenheit (35 Celsius) was the point when the body started having trouble, said Kenney, who also runs a hot box lab and has done nearly 600 tests with volunteers.
His tests show the wet-bulb danger point is closer to 87 (30.5 Celsius). That’s a figure that has started to appear in the Middle East, he said.
And that’s just for young healthy people. For older people, the danger point is a wet bulb temperature of 82 (28 degrees Celsius), he said.
“Humid heat waves kill a lot more people than dry heat waves,” Kenney said.
When Kenney tested young and old people in dry heat, young volunteers could function until 125.6 degrees (52 degrees Celsius), while the elderly had to stop at 109.4 (43 degrees Celsius). With high or moderate humidity, the people could not function at nearly as high a temperature, he said.
“Humidity impacts the ability of sweat to evaporate,” Jay said.
Heatstroke is an emergency, and medical workers try to cool a victim down within 30 minutes, Salas said.
The best way: Cold water immersion. Basically, “you drop them in a water bucket,” Salas said.
But those aren’t always around. So emergency rooms pump patients with cool fluids intravenously, spray them with misters, put ice packs in armpits and groins and place them on a chilling mat with cold water running inside it.
Sometimes it doesn’t work.
“We call it the silent killer because it’s not this kind of visually dramatic event,” Jay said. “It’s insidious. It’s hidden.”
___
This story has corrected to “humidity,” rather than “temperature” in a mention of how people’s function is affected by humidity.
___
Read more of AP’s climate coverage at http://www.apnews.com/climate-and-environment
___
Follow Seth Borenstein on X at @borenbears
______
The Associated Press’ climate and environmental coverage receives financial support from multiple private foundations. AP is solely responsible for all content. Find AP’s standards for working with philanthropies, a list of supporters and funded coverage areas at AP.org.






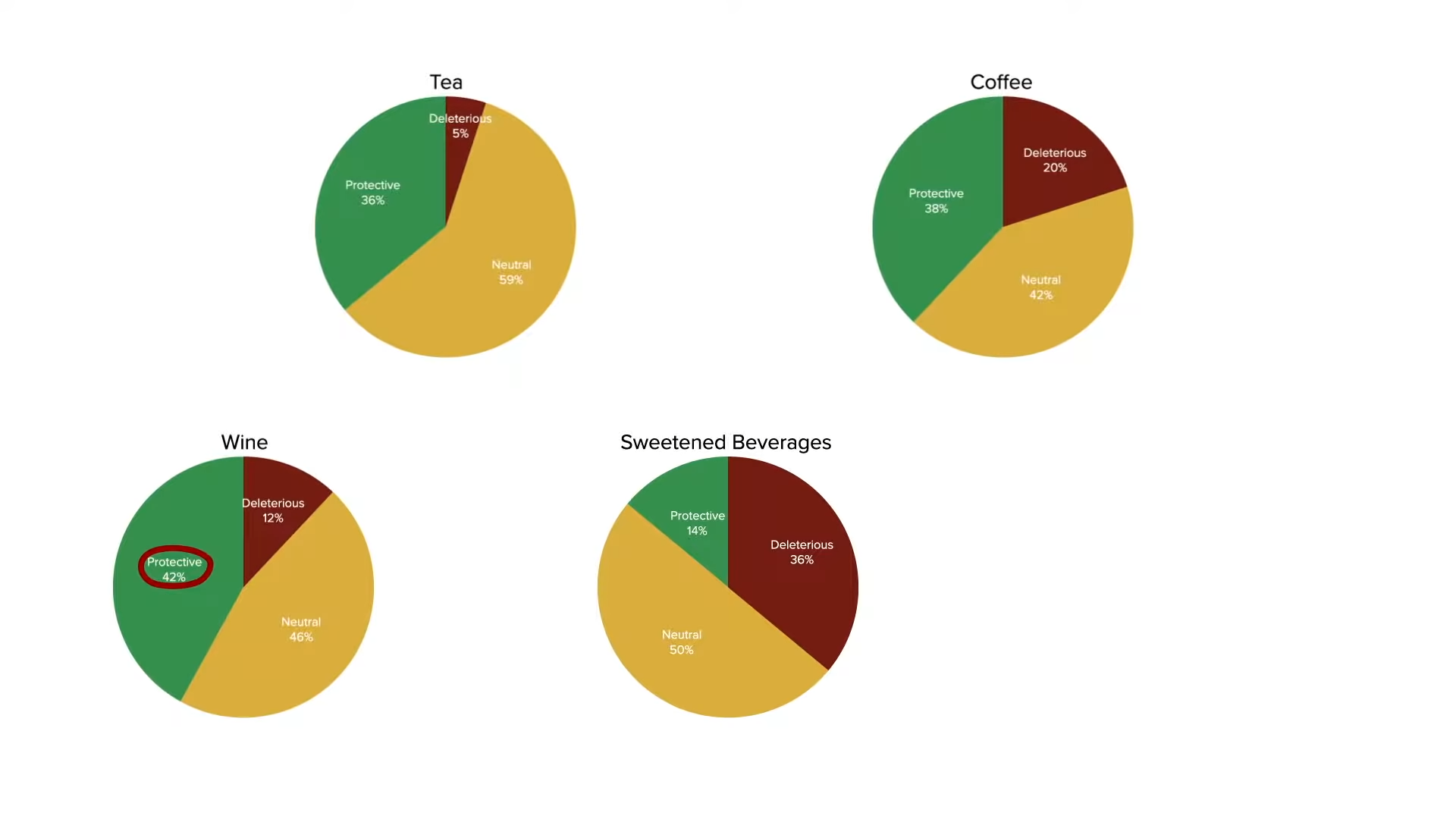
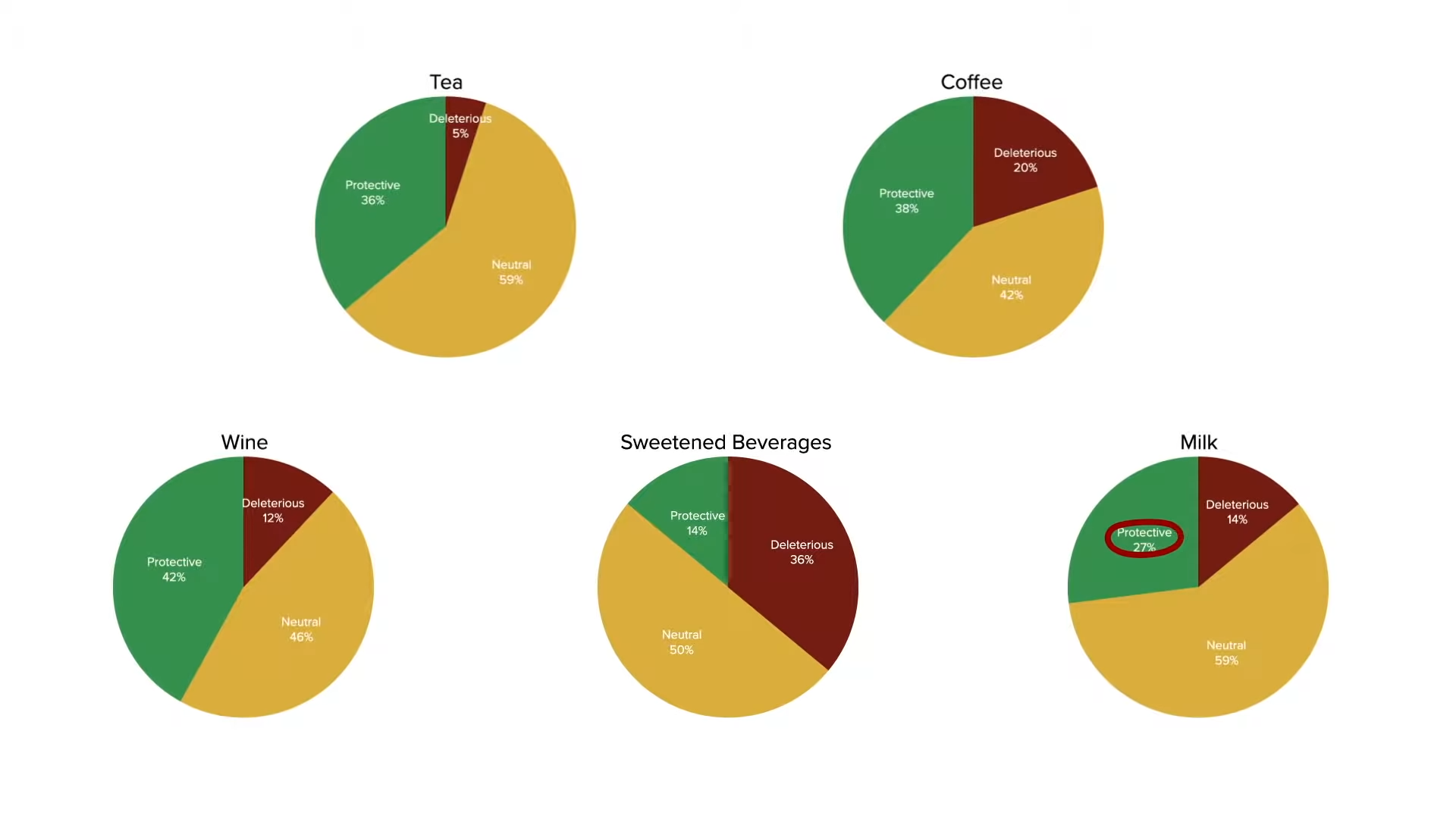


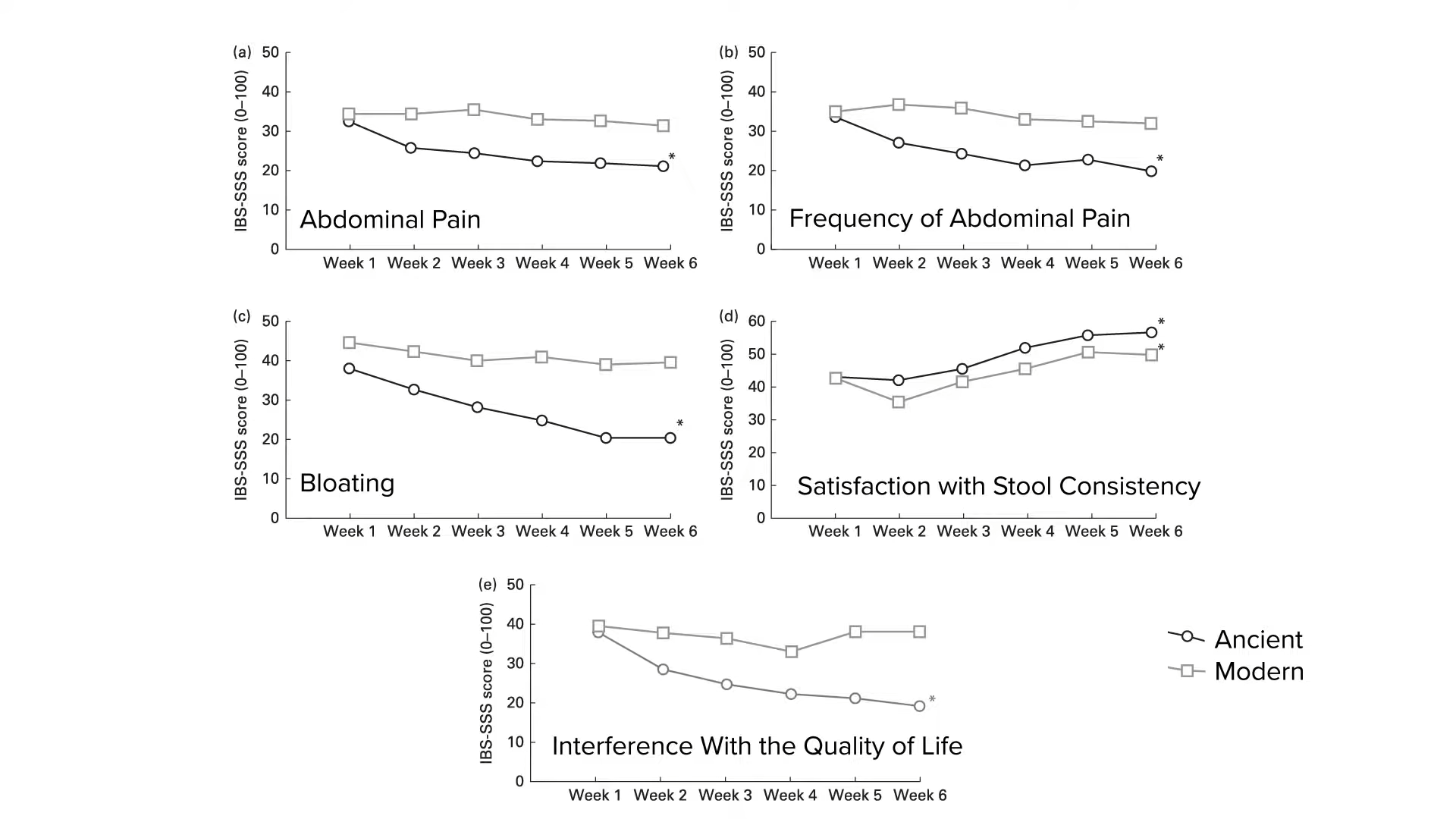


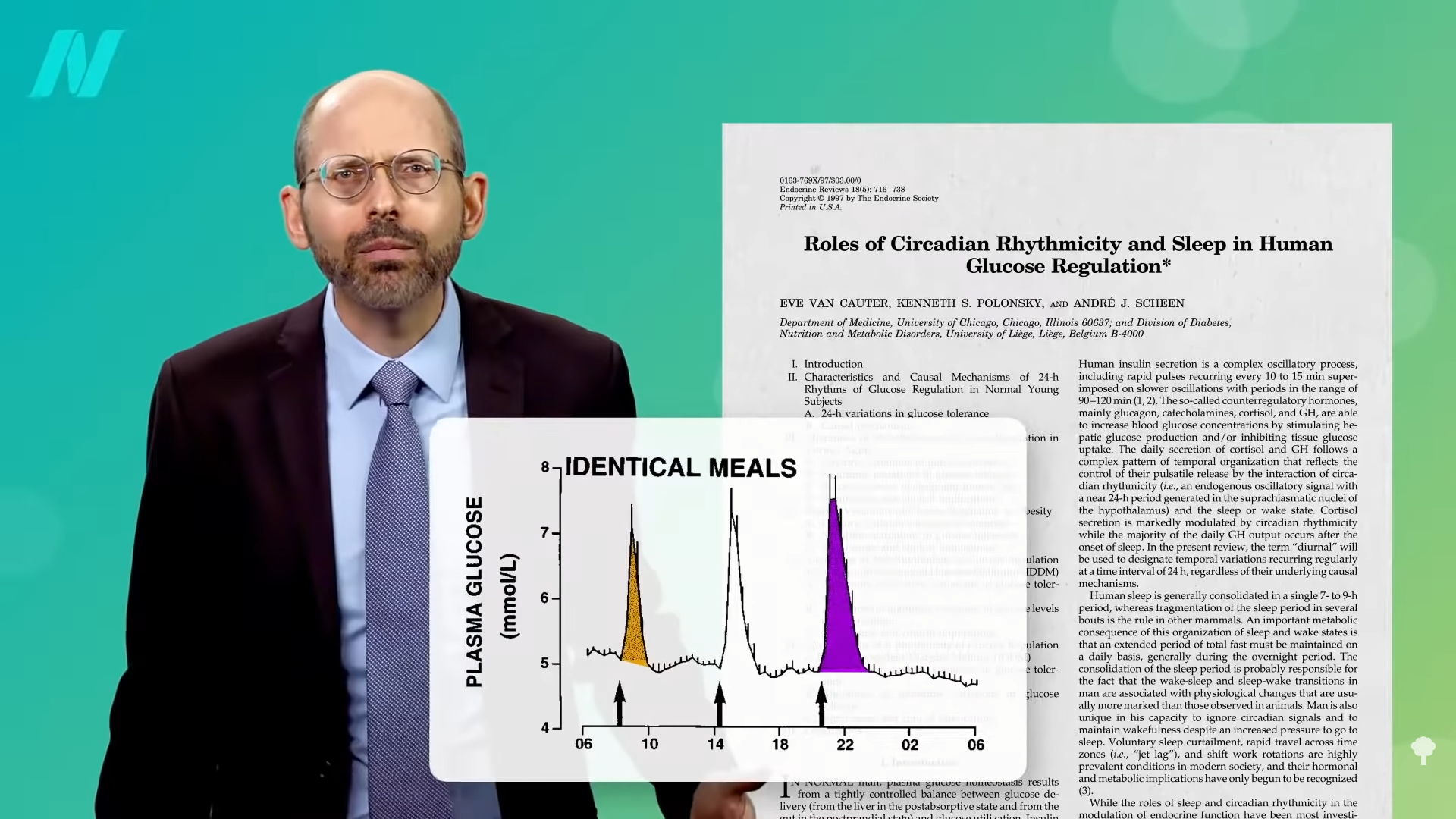
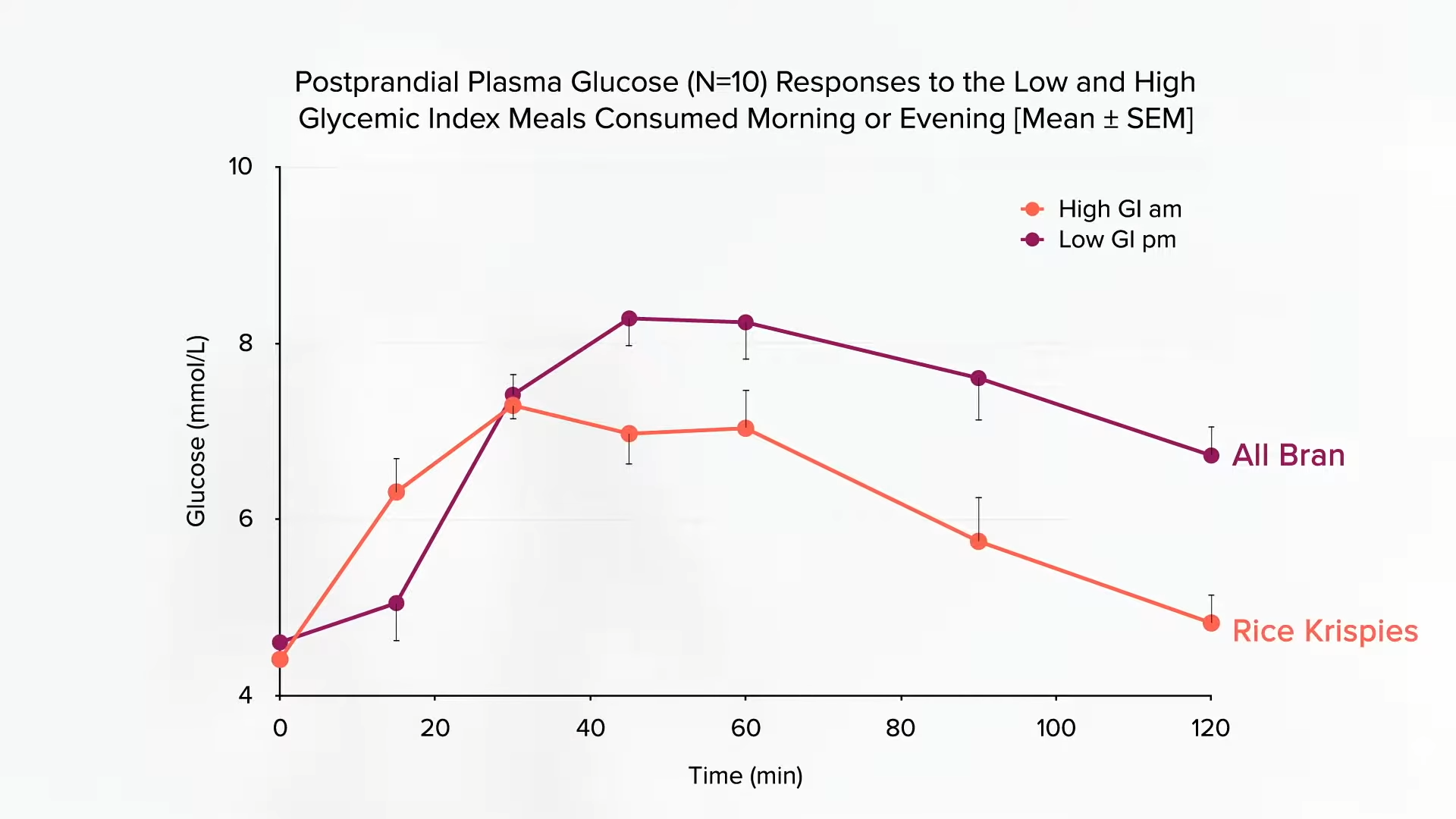
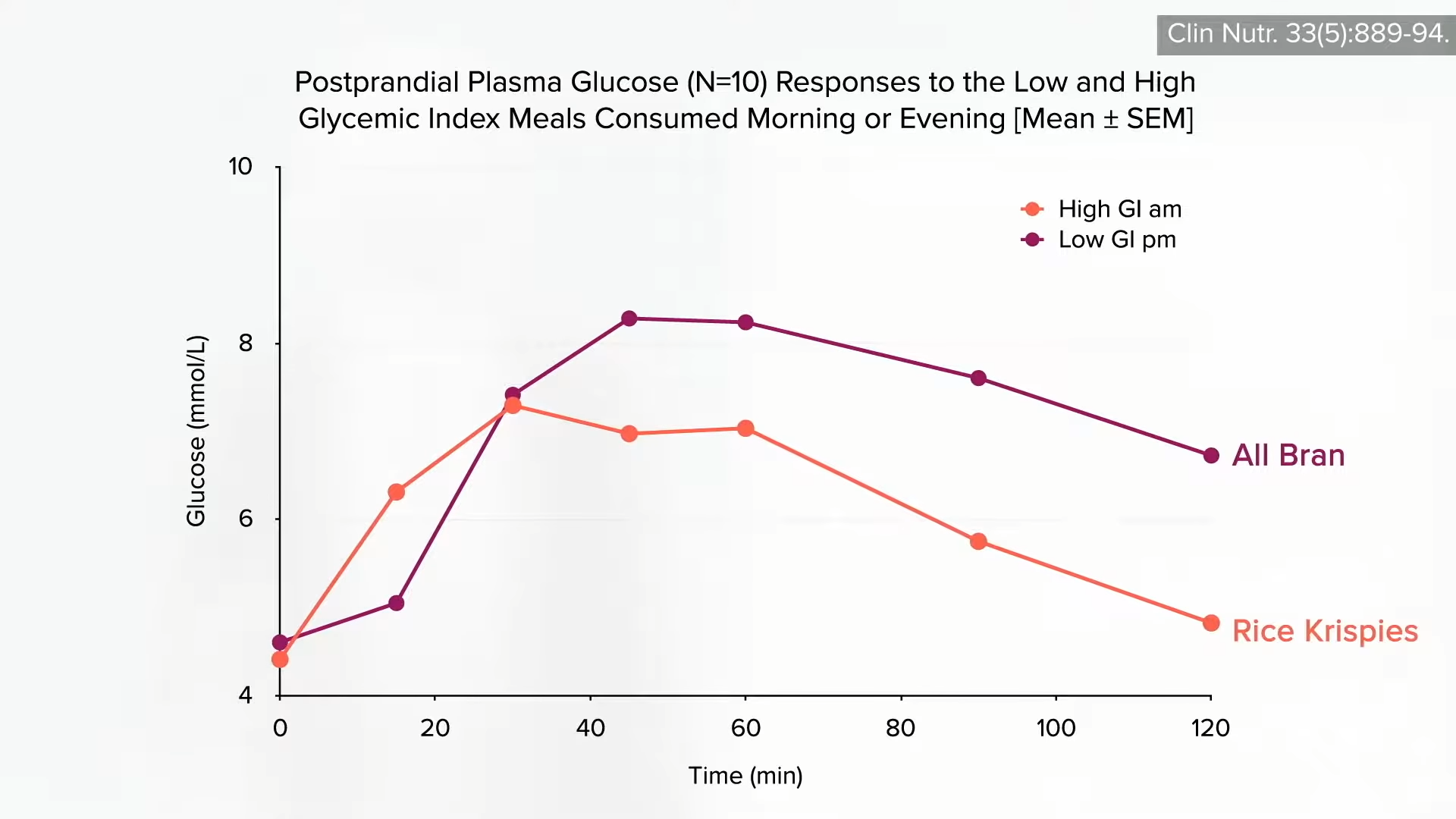


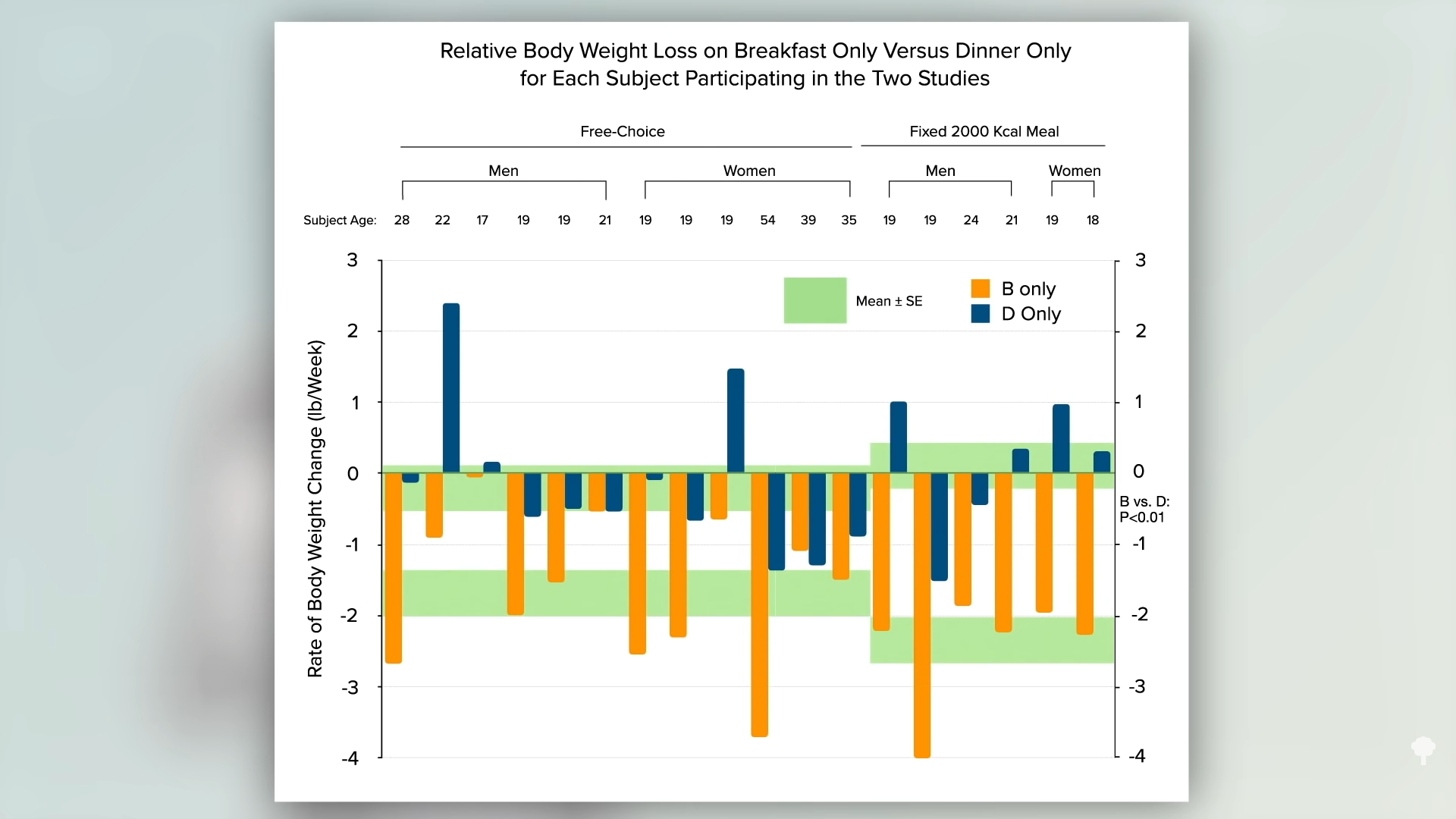


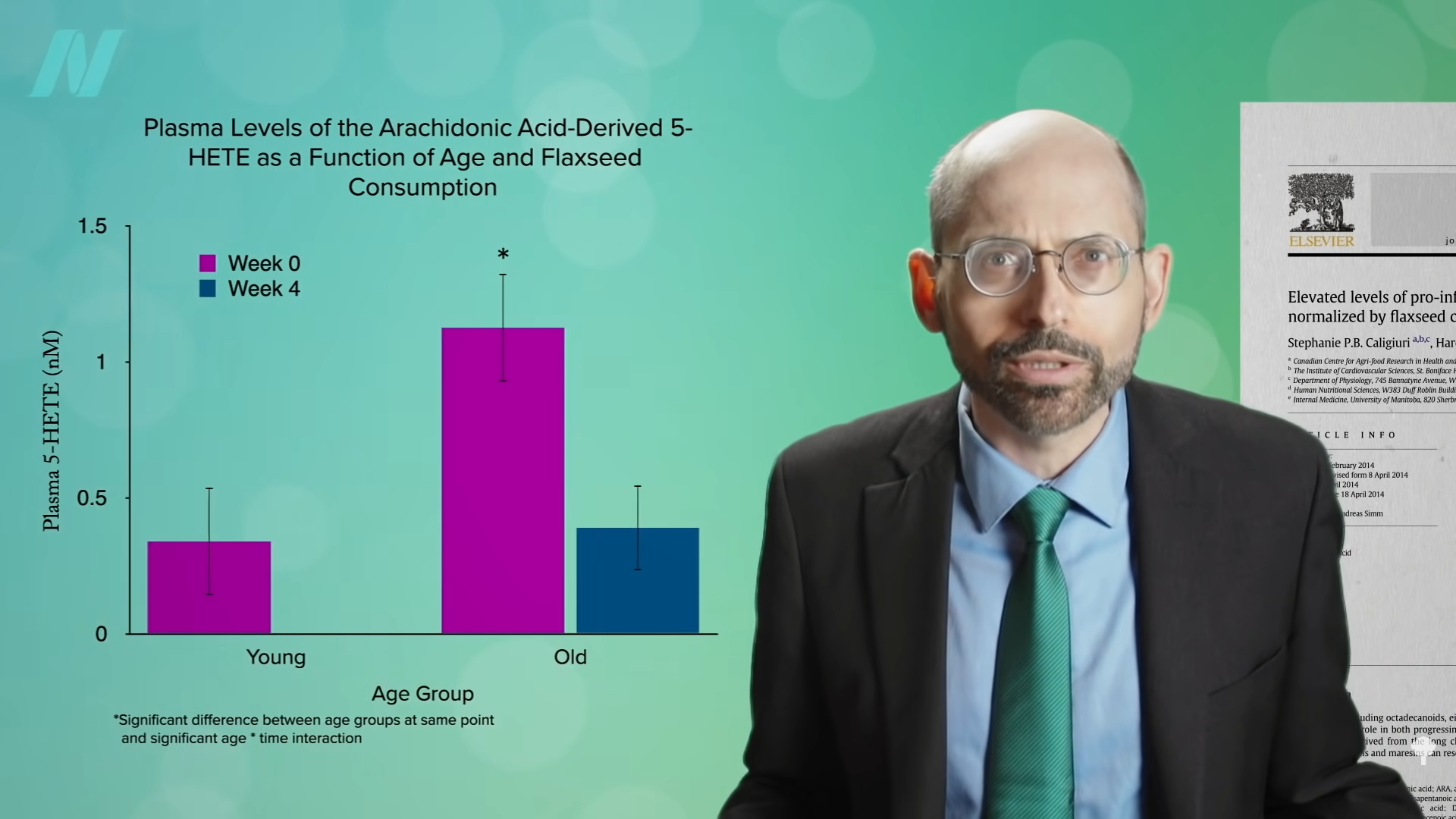



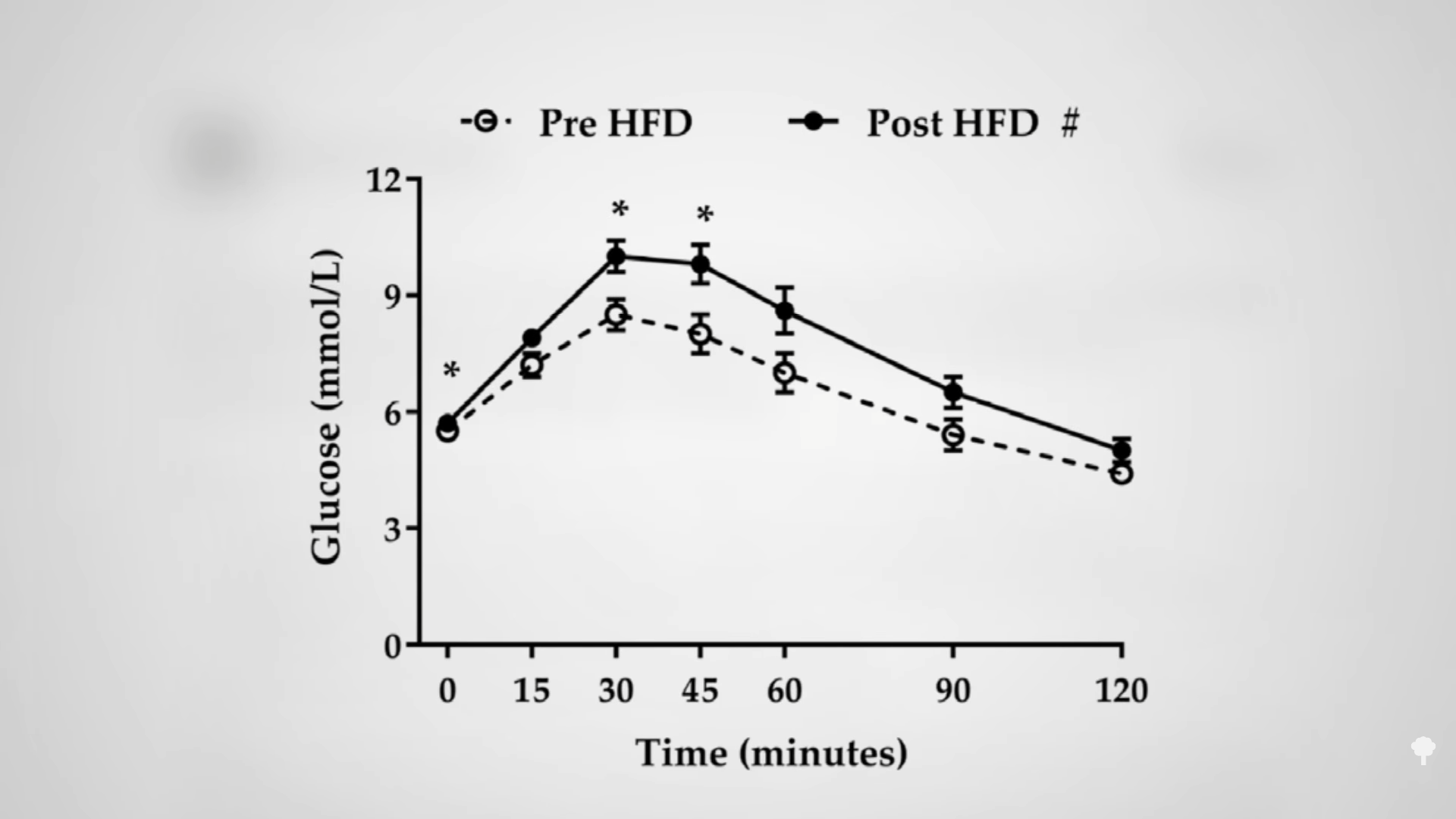
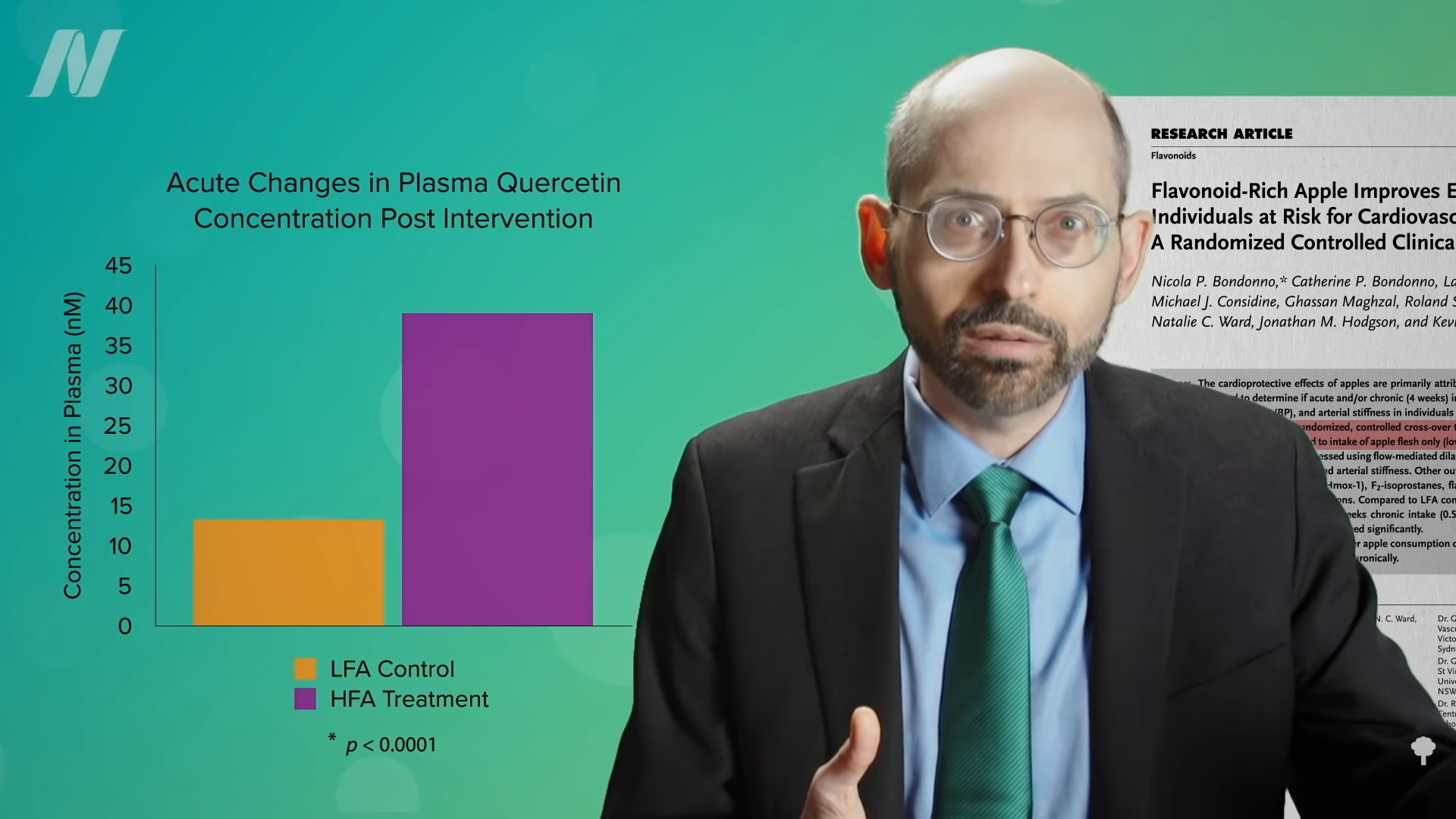 Even compared to spinach? As you can see in the graph below and at 3:14 in my
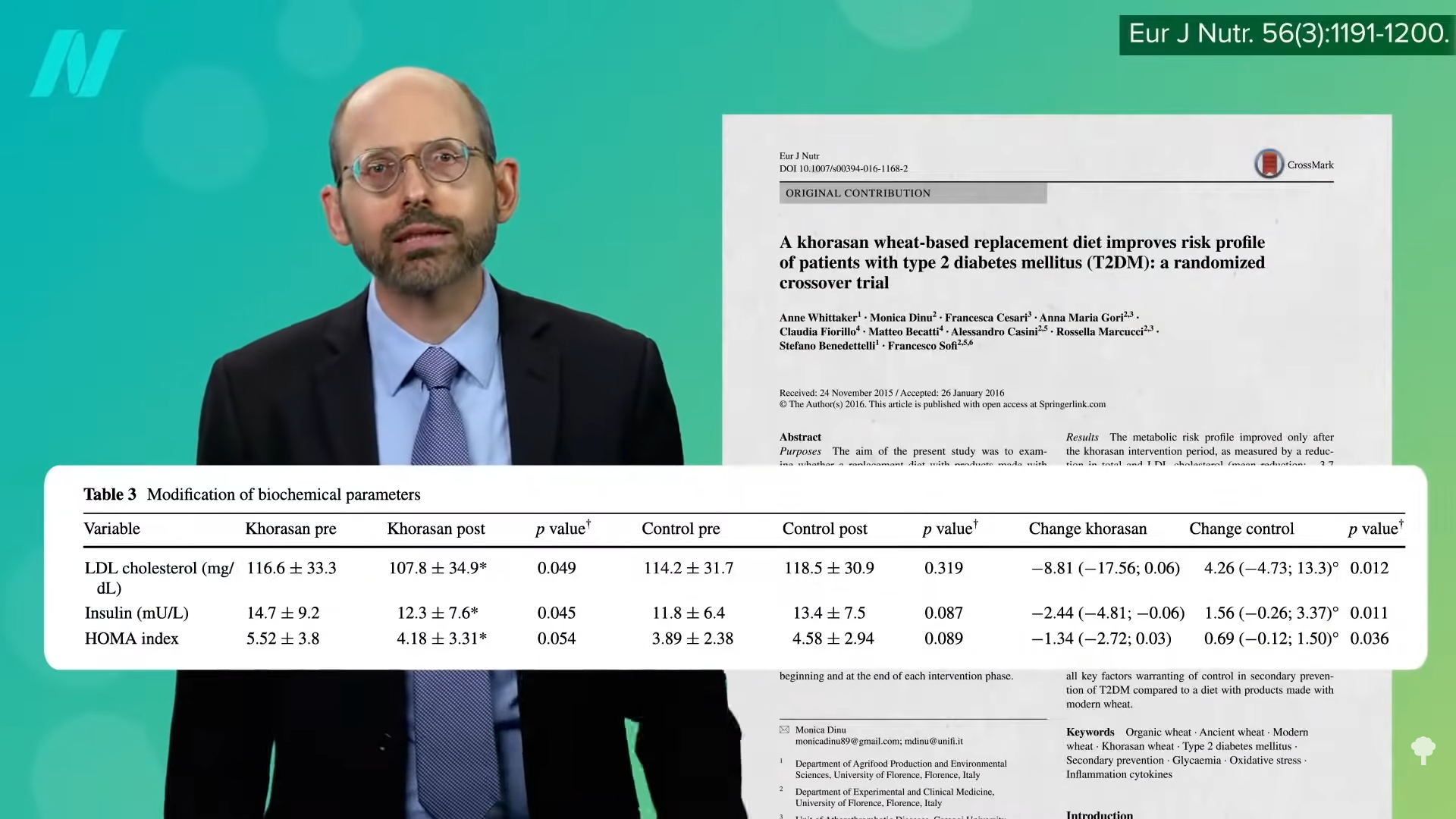
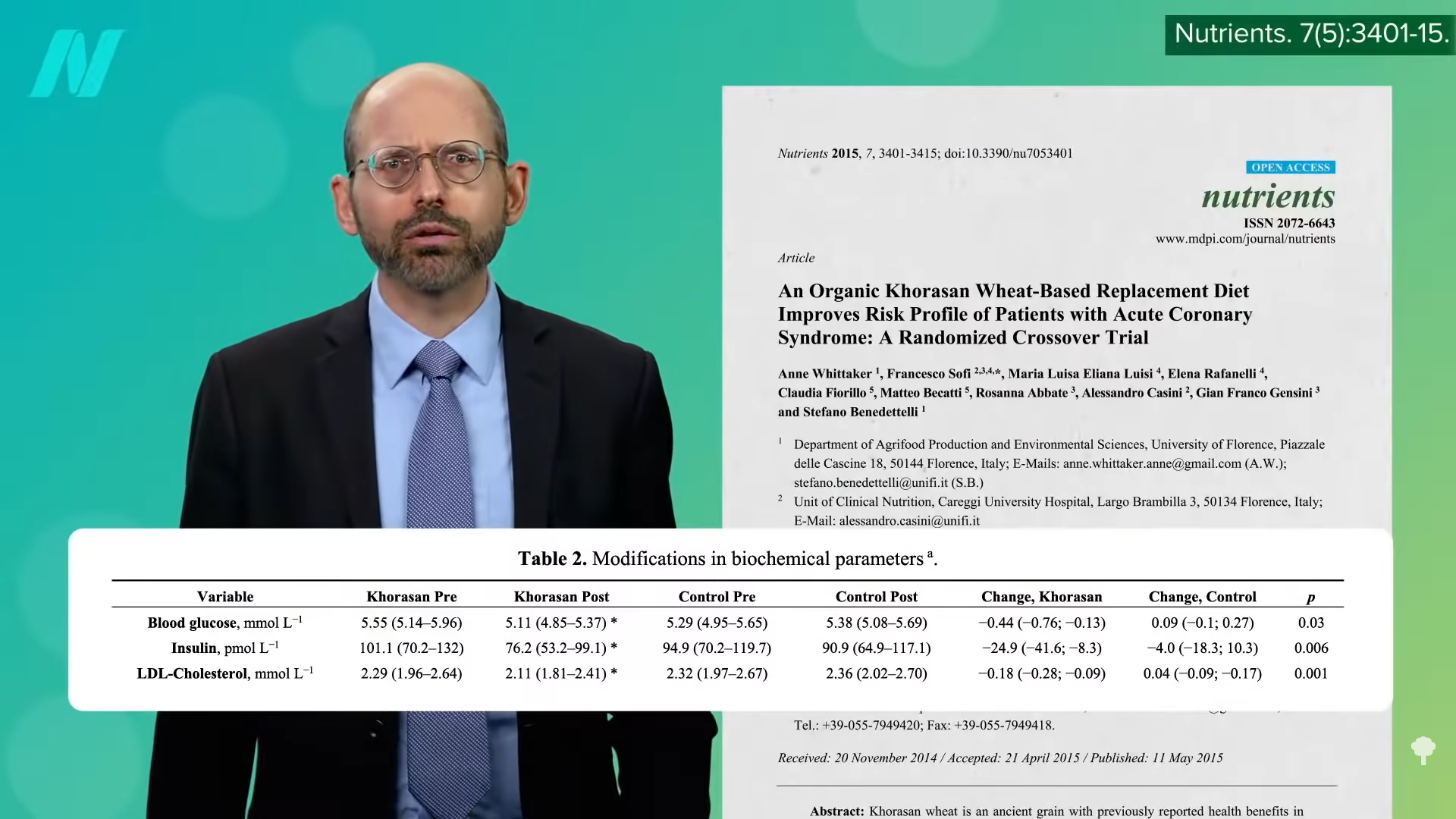
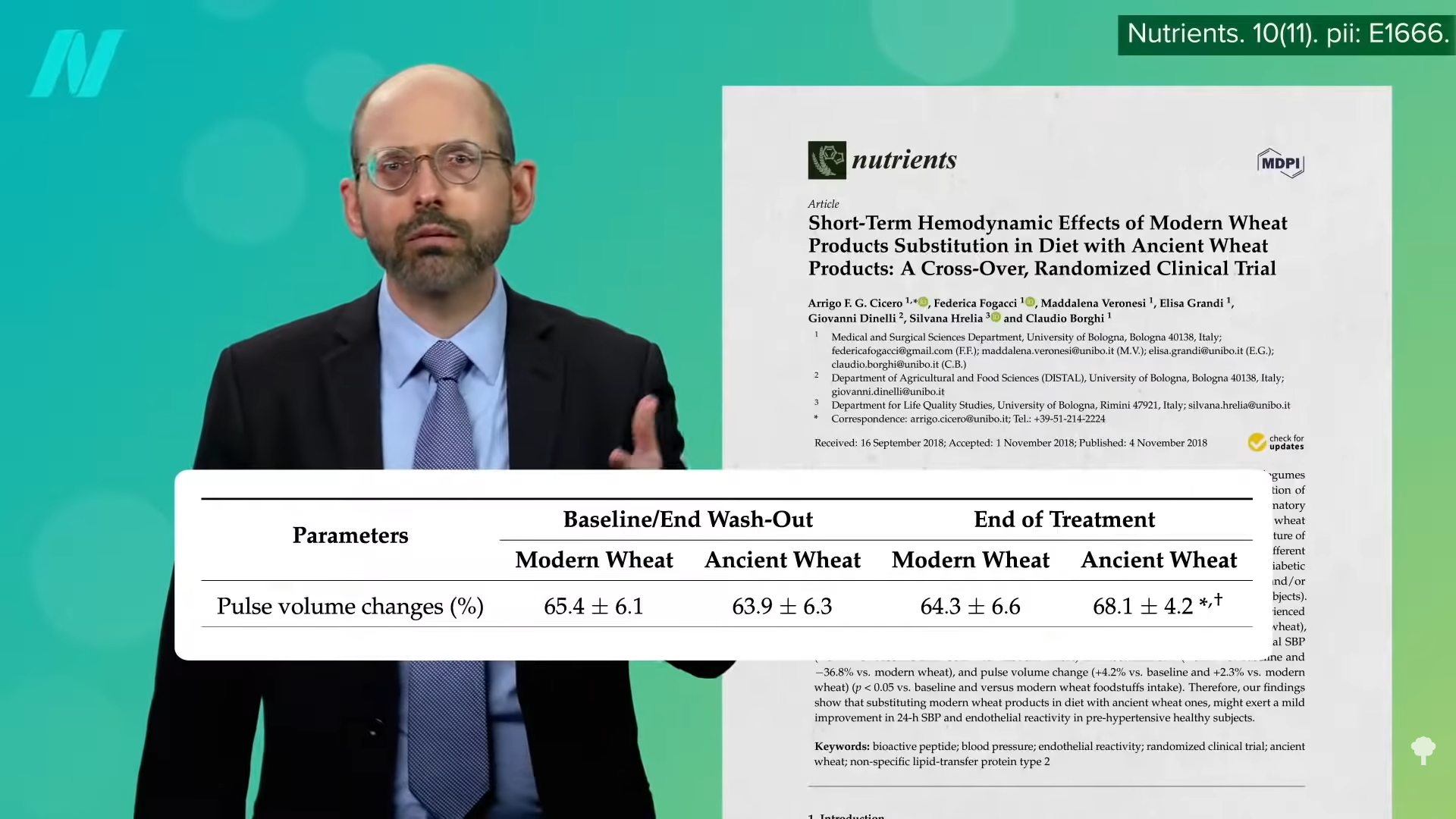
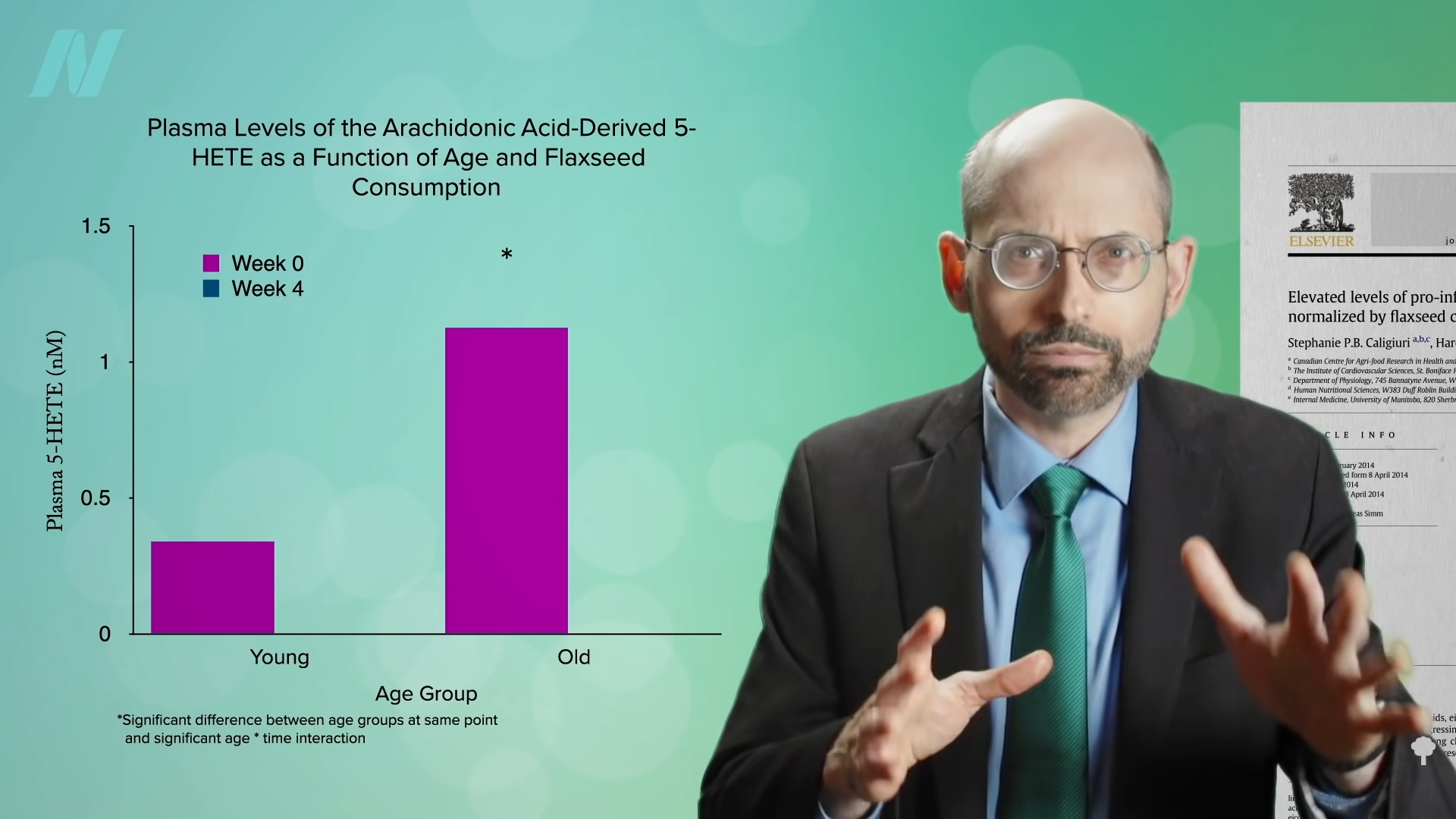
Even compared to spinach? As you can see in the graph below and at 3:14 in my 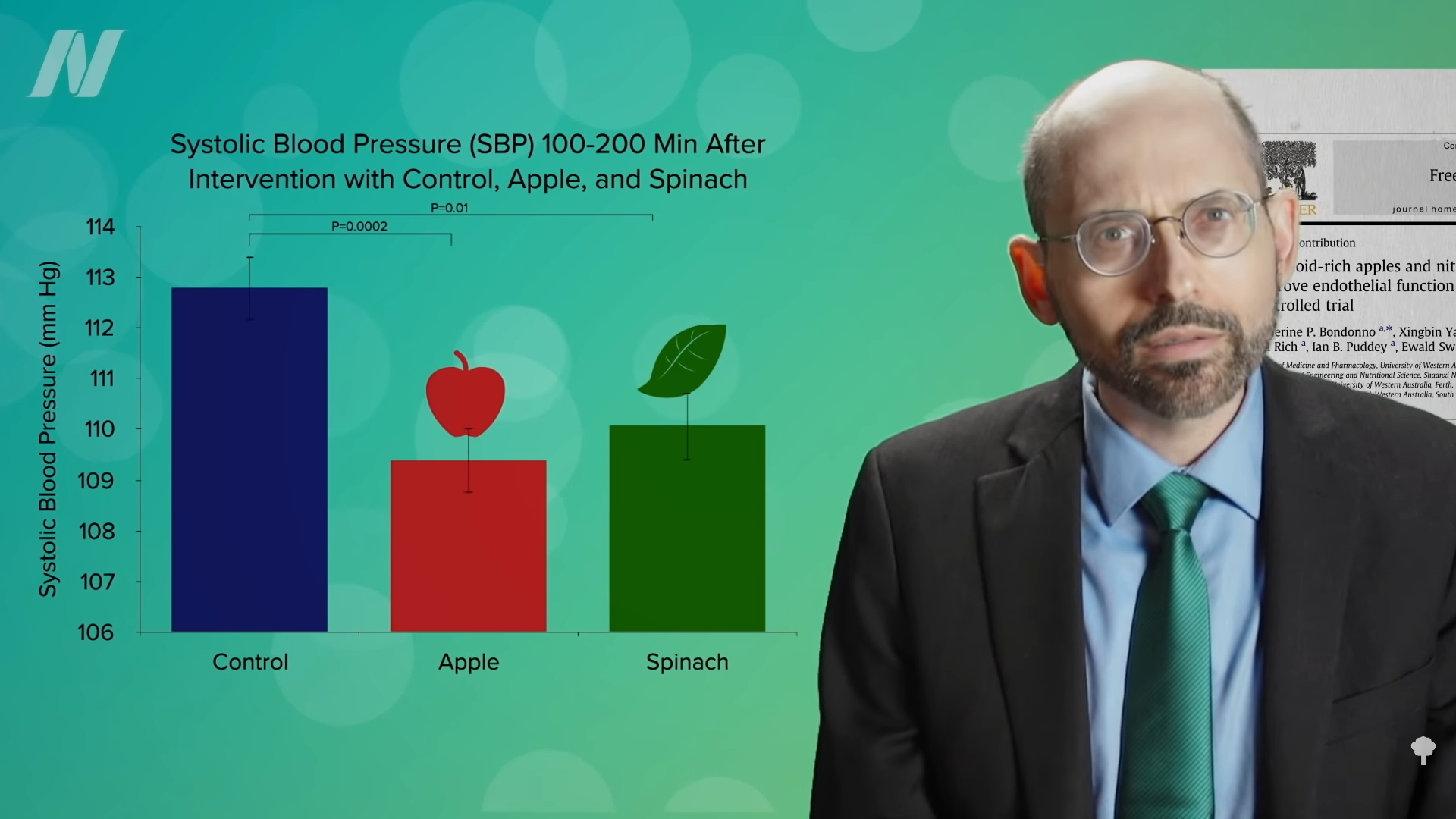 What’s nice about these results is that we’re talking about whole foods, not some supplement or extract. So, easily, “this could be translated into a natural and low-cost method of reducing the cardiovascular risk profile of the general population.”
What’s nice about these results is that we’re talking about whole foods, not some supplement or extract. So, easily, “this could be translated into a natural and low-cost method of reducing the cardiovascular risk profile of the general population.” 

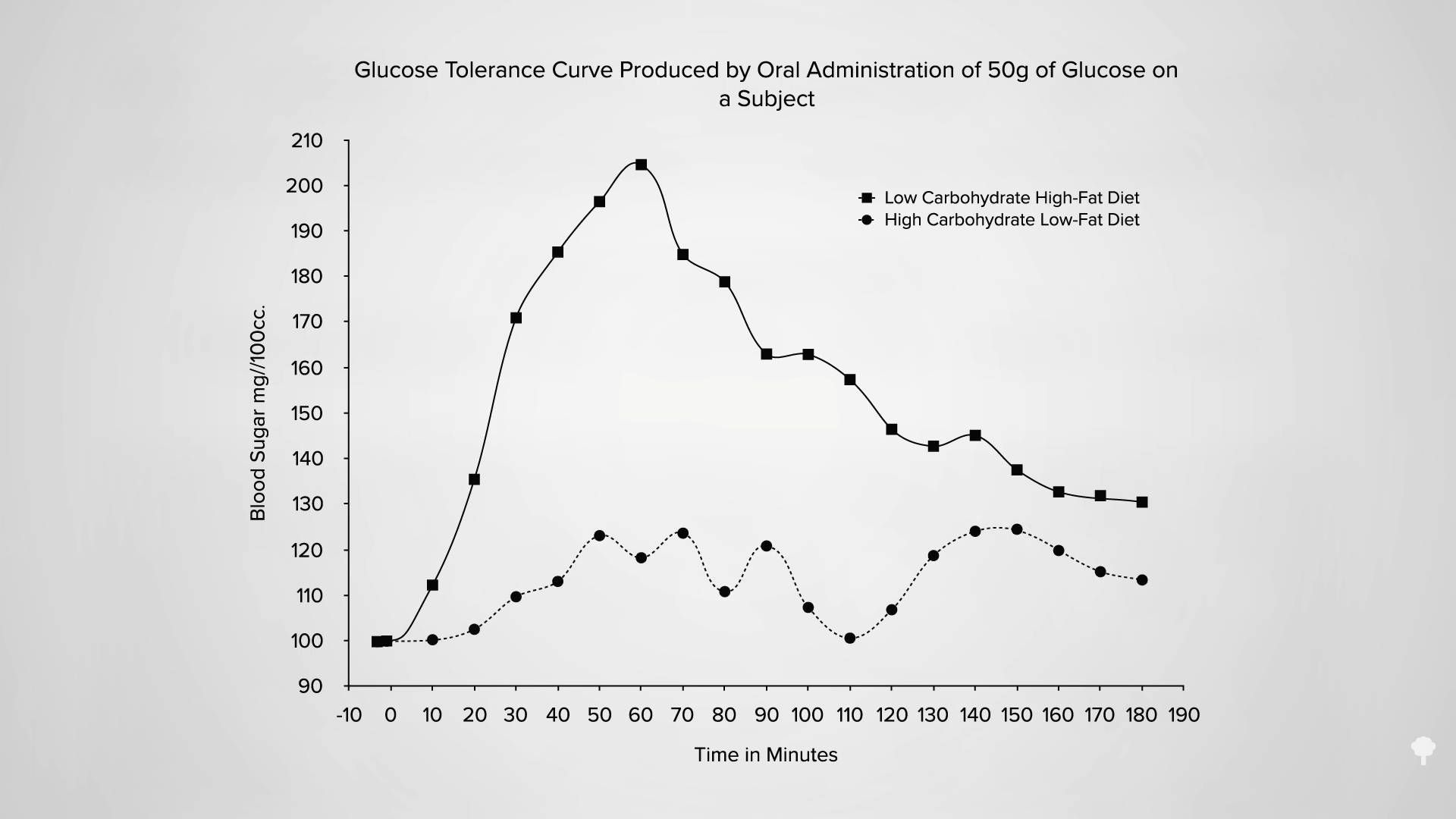
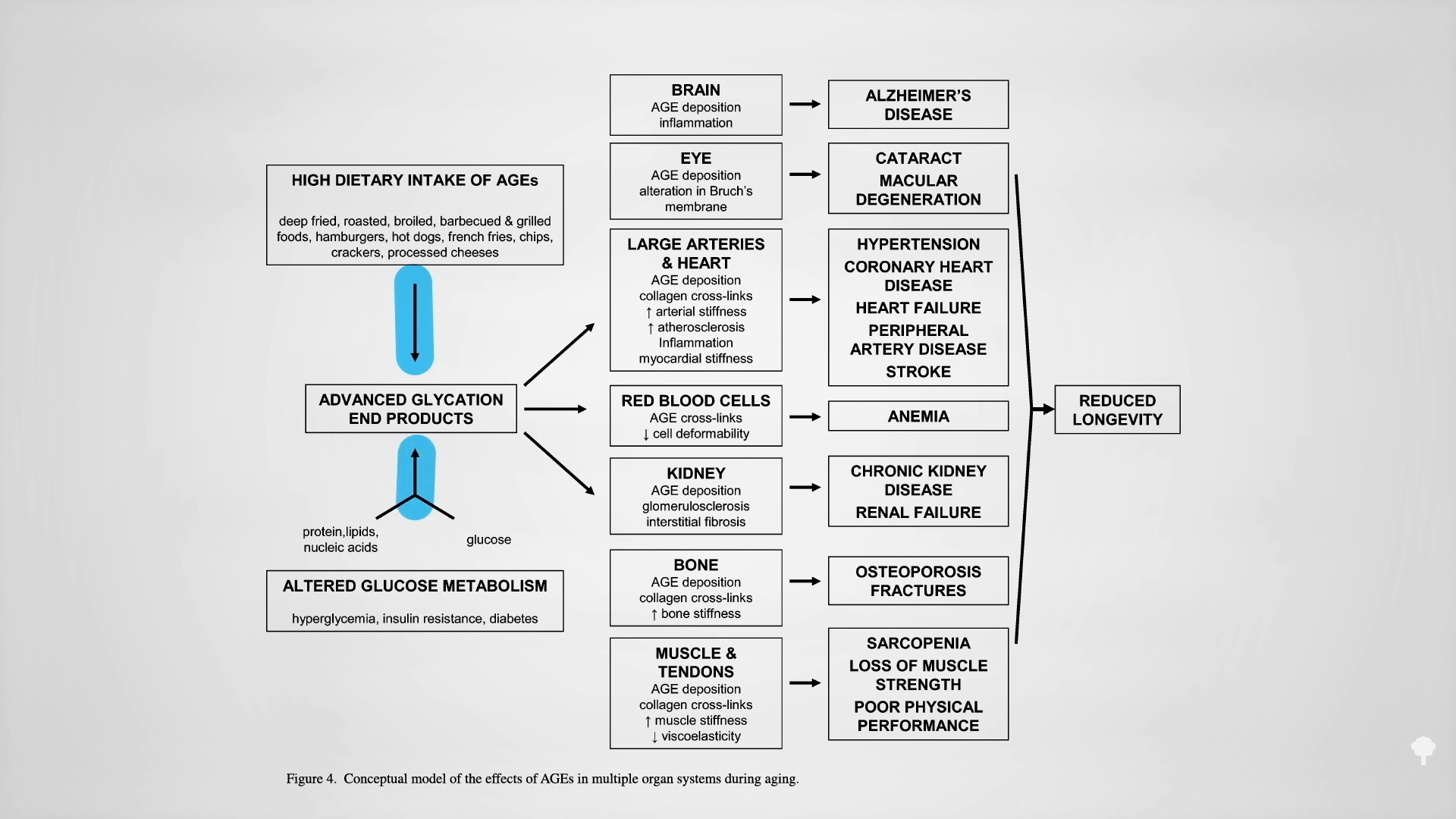
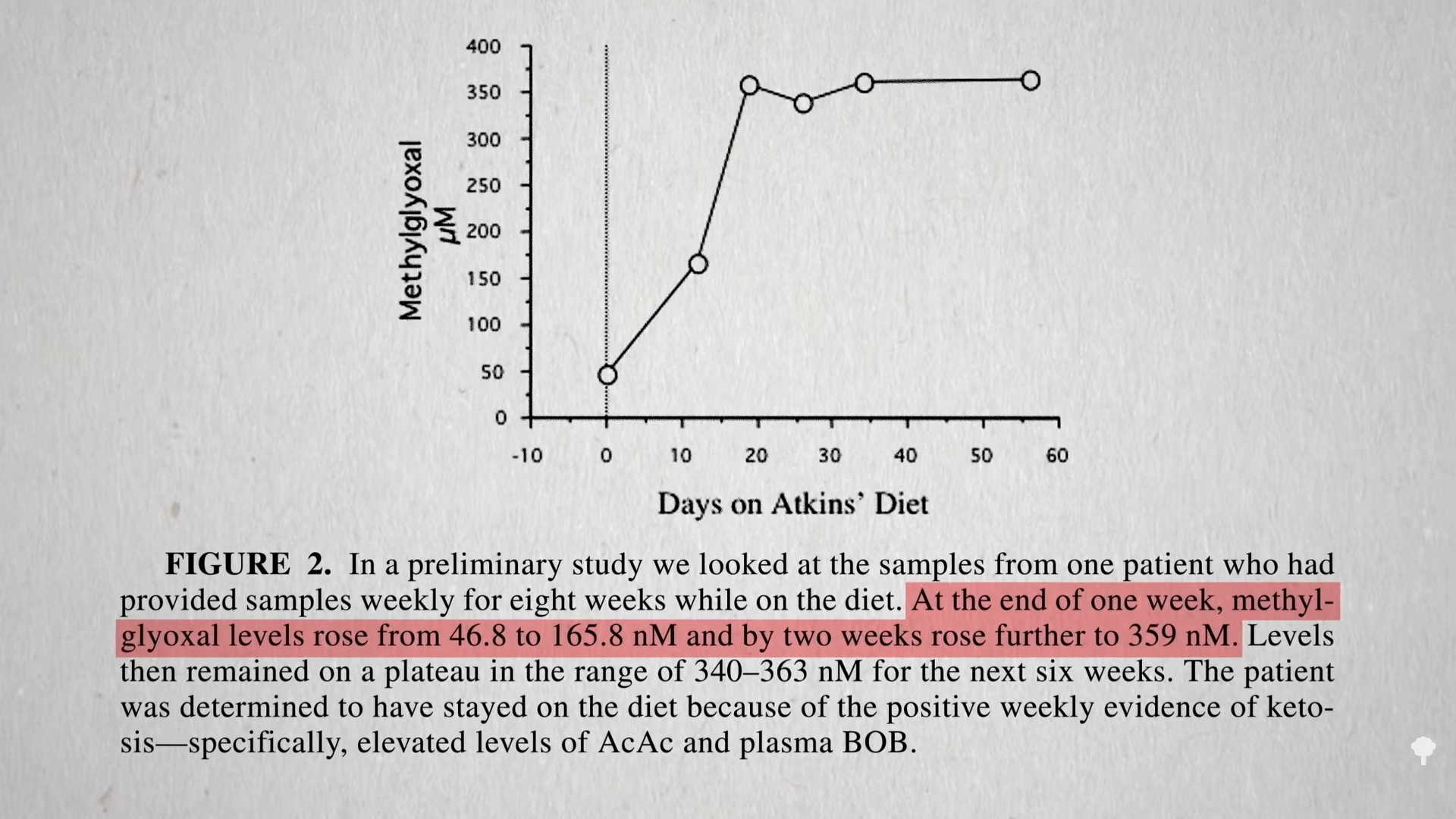
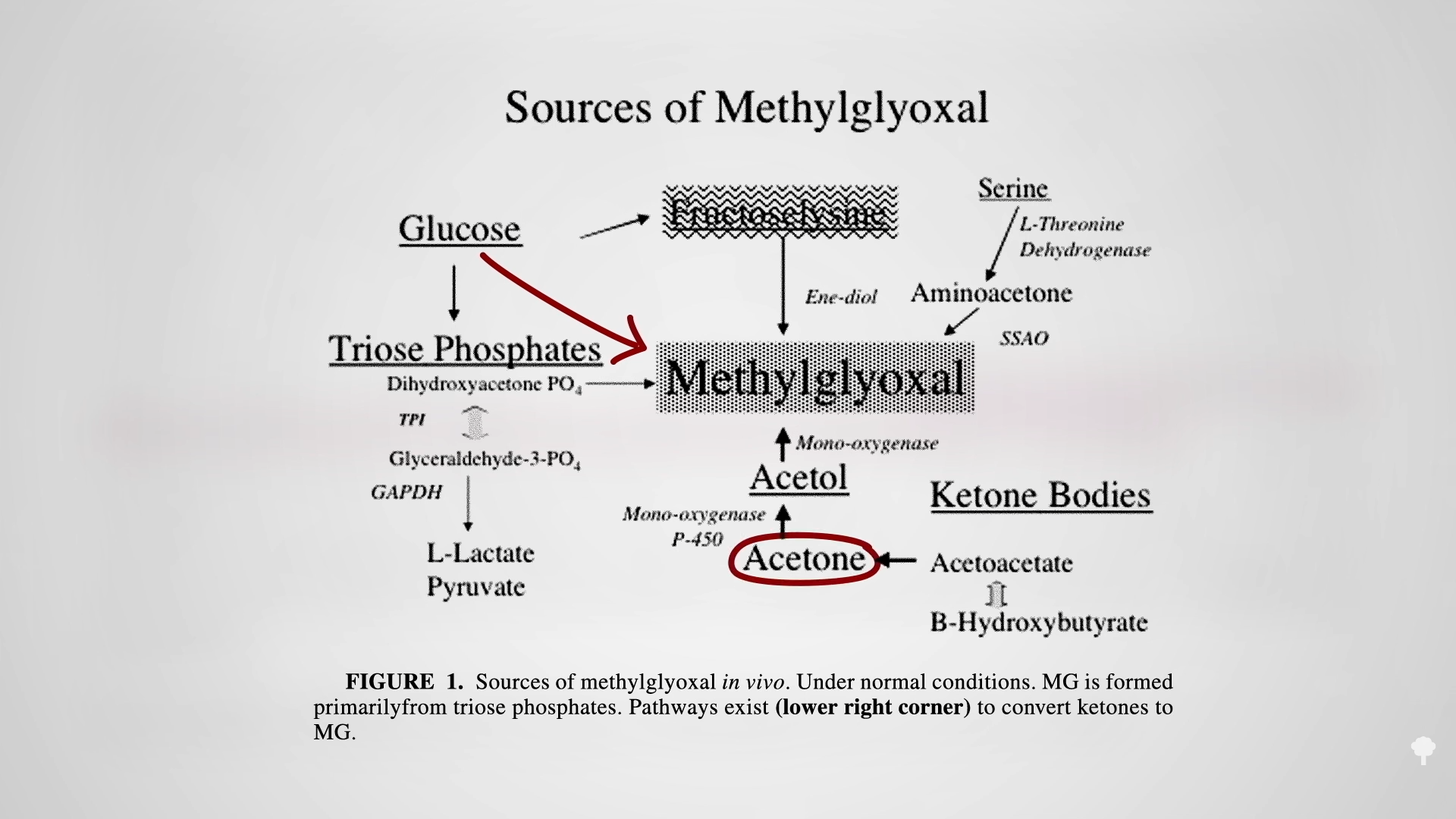
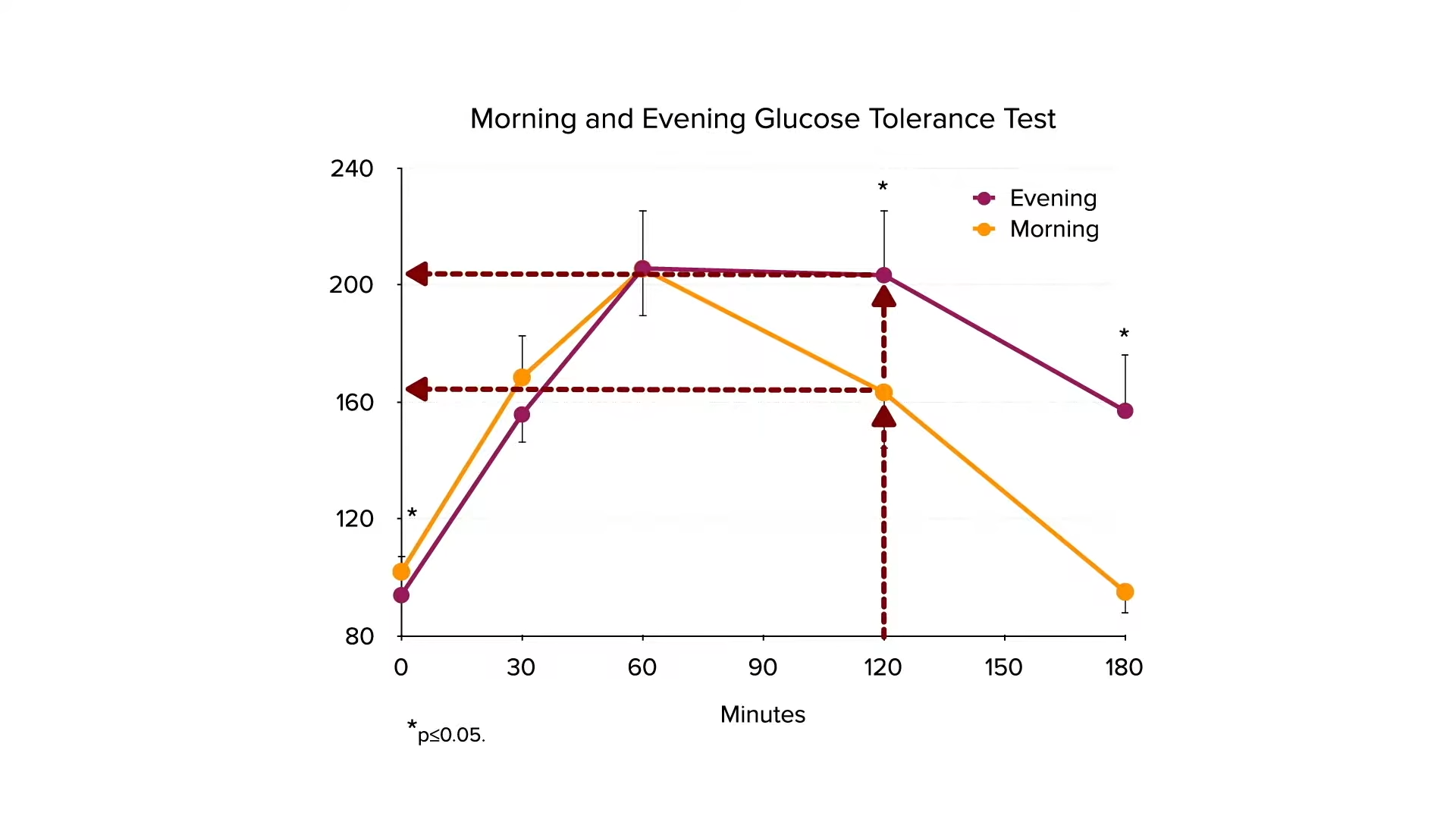
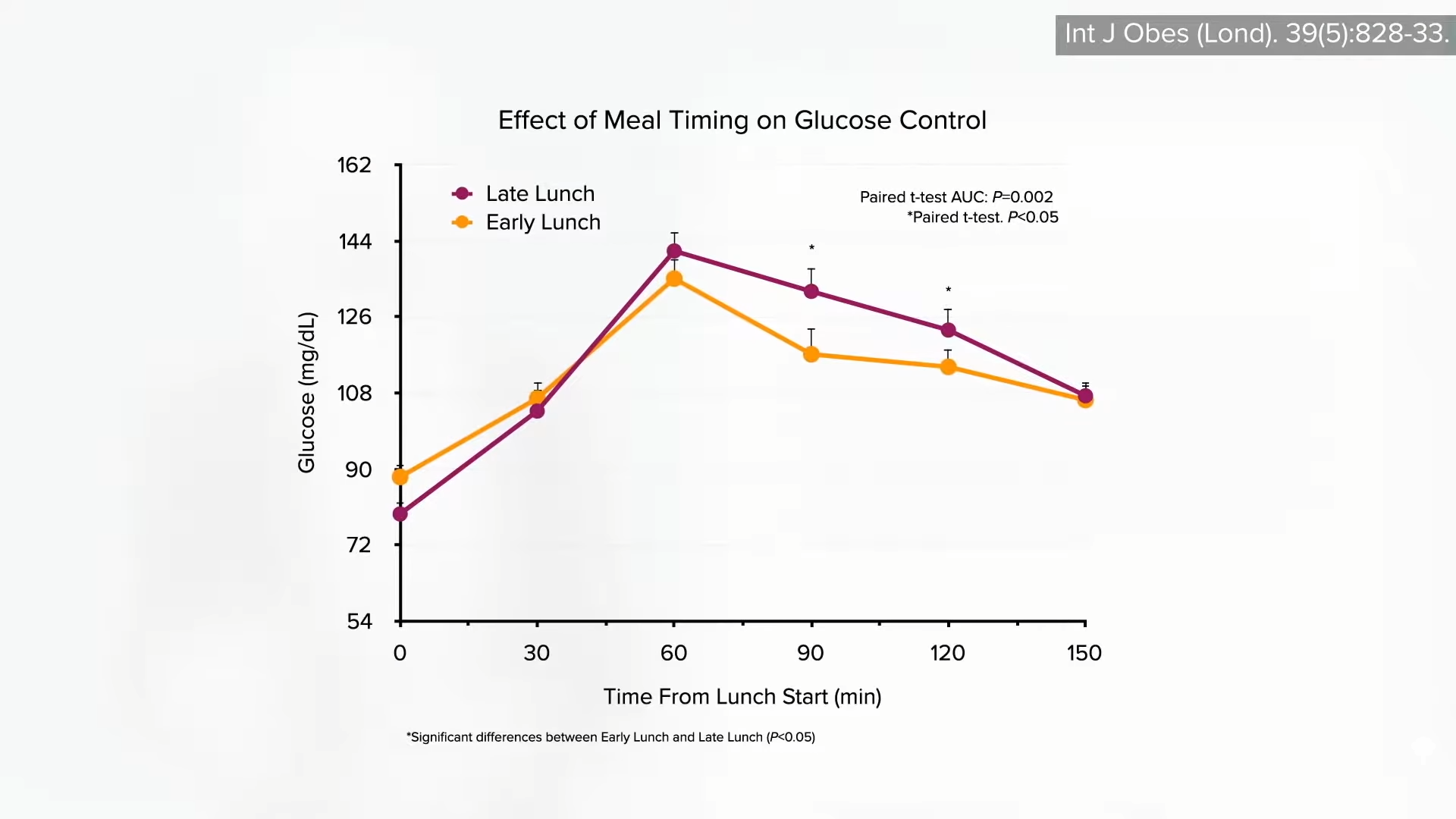
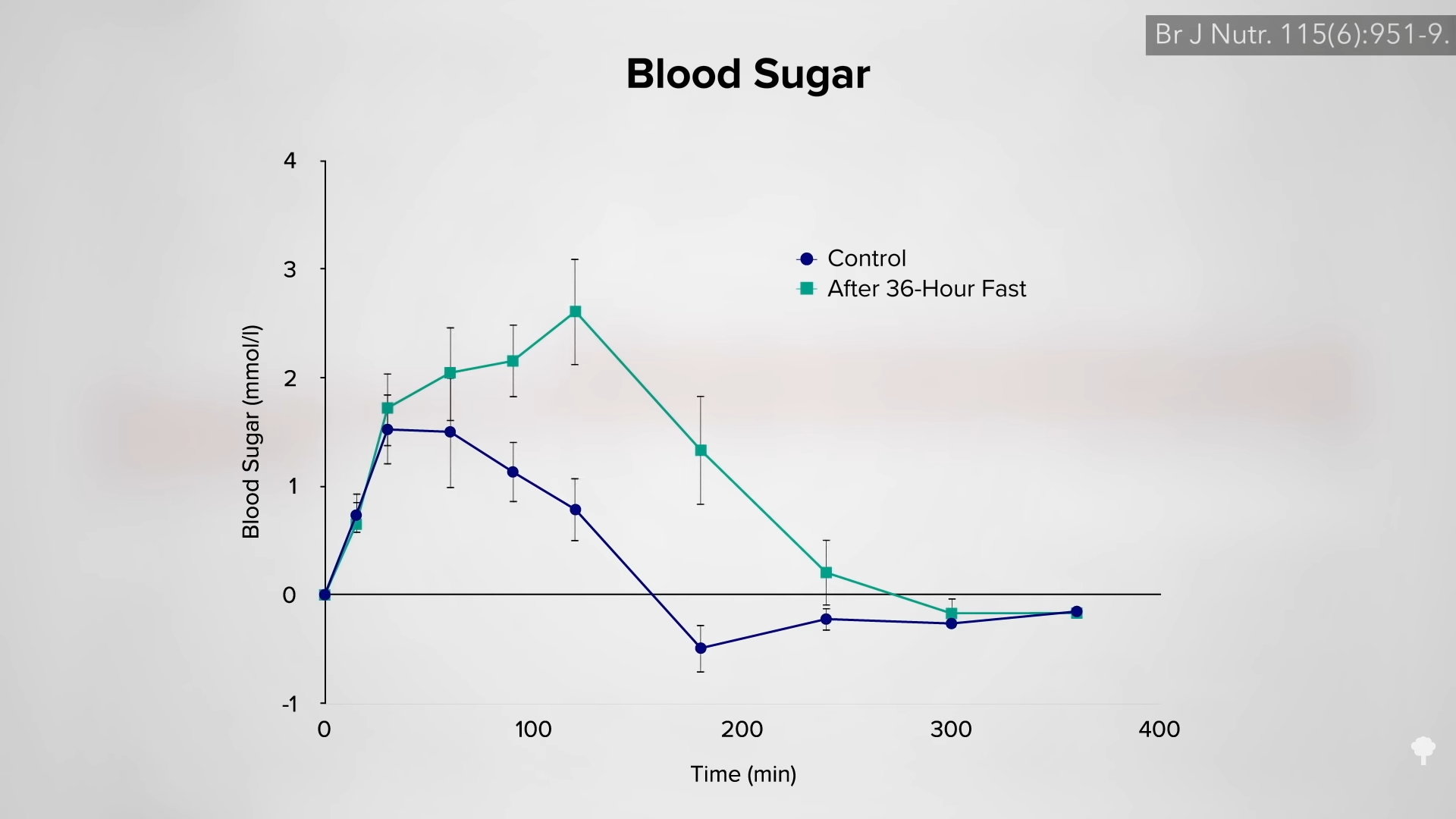
 The irony doesn’t stop there. One of the reasons people with diabetes suffer such nerve and artery damage is due to an inflammatory metabolic toxin known as methylglyoxal, which forms at high blood sugar levels. Methylglyoxal
The irony doesn’t stop there. One of the reasons people with diabetes suffer such nerve and artery damage is due to an inflammatory metabolic toxin known as methylglyoxal, which forms at high blood sugar levels. Methylglyoxal