Anyone 6 months and older who wants a COVID-19 shot in Colorado can now get one, but the vaccine will only be free for those with the right insurance — at least for now.
Initially, pharmacies couldn’t administer the updated shots in Colorado unless a patient had a prescription. The state allows pharmacists to administer vaccines recommended by the Centers for Disease Control and Prevention’s advisory committee, but not other shots.
Dr. Ned Calonge, chief medical officer for the state health department, responded by issuing a standing order — essentially, a prescription for every resident – allowing them to get vaccinated at retail pharmacies.
But that order doesn’t guarantee insurance will cover the shots or that pharmacies will choose to stock them. Last year, fewer than half of people over 65 nationwide received an updated COVID-19 shot, with uptake dropping further in younger age groups, raising questions about whether health care providers will believe demand is high enough to justify buying the vaccine.
“The standing order provides accessibility. It doesn’t necessarily provide availability,” Calonge said Tuesday.
The Colorado Division of Insurance issued a draft rule last week that would require state-regulated plans to cover COVID-19 vaccines without out-of-pocket costs for people of any age, assuming the division passes it as written. Insurance cards from state-regulated plans typically have CO-DOI printed in the lower left corner.
The state’s rule doesn’t apply to federally regulated plans, which account for about 30% of employer-sponsored insurance plans in Colorado, Calonge said. Typically, however, those plans try to offer competitive benefits, since they mostly serve large employers, he said.
“My hope would be they would want to keep up with other insurers,” he said.
This isn’t the first time that people on state-regulated plans have had benefits not guaranteed for people with federally regulated insurance.
Colorado capped the cost of insulin and epinephrine shots to treat severe allergic reactions in state plans, but couldn’t require the same for plans the state doesn’t oversee. In those cases, it offered an “affordability program” requiring manufacturers to supply the medication at a lower cost for people who aren’t covered by the state caps, Medicare or Medicaid.
At least two Colorado insurers surveyed by The Denver Post said all of their plans will cover COVID-19 vaccines, while others hedged.
Select Health, which sells Medicare and individual marketplace plans in Colorado, said its plans currently cover COVID-19 vaccines without out-of-pocket costs for everyone. Kaiser Permanente Colorado said in a message to members that it will pay for the shot for anyone 6 months or older.
Donna Lynne, CEO of Denver Health, said the health system’s insurance arm is waiting on clarification about when it should cover the vaccines. Denver Health Medical Plan offers multiple plan types, some state-regulated and some under federal rules, she said.
“It’s less of a decision on our part than understanding what the health department and the insurance department are saying,” she said. “You can’t have one insurance company saying they are doing it and one saying they aren’t doing it.”
Anthem said it considers immunizations “medically necessary” if the American Academy of Pediatrics, American Academy of Family Physicians or the CDC’s vaccine advisory committee has recommended them, but didn’t specify whether it would charge out-of-pocket costs for medically necessary vaccines.
If those bodies stated that certain people could get a particular vaccine — but not that they should — Anthem would decide about coverage “on an individual basis,” its website said. The other groups have recommended the shots for people over 18 or under 2, with the option for healthy children in between to get a booster if their parents wish.
The state’s Medicaid program is still waiting for guidance from federal authorities about whose vaccines it can cover, according to the Colorado Department of Health Care Policy and Financing, and Medicare isn’t yet paying for the shots.
For most of the COVID-19 vaccines’ relatively brief existence, they were free and recommended for everyone 6 months and older. In 2024, the federal government stopped paying for them, which meant uninsured people no longer could be sure they could get the shot without paying.
Almost all insurance plans still were required to pay for the shots, though, because the CDC’s Advisory Committee on Immunization Practices recommended them.
In previous years, the committee recommended updated shots within days of the U.S. Food and Drug Administration approving them. In late August, the FDA approved the updated vaccines for people over 65 and those with one of about 30 conditions increasing their risk of severe disease, including asthma, obesity and diabetes.
Doctors still could prescribe the vaccine “off-label” to healthy people, in the same way that they prescribe adult medications for children when an alternative specifically approved for kids isn’t available.
This year, however, the committee won’t meet until Thursday, and may not recommend the shots when it does. Secretary of Health and Human Services Robert F. Kennedy Jr. dismissed all of the committee’s members earlier this year and replaced them with new appointees, most of whom oppose COVID-19 vaccines.
The committee’s decision also will determine whether the Vaccines for Children program can supply the shots for children who are uninsured, covered by Medicaid or are members of American Indian tribes, Calonge said. If the committee decides not to recommend the vaccines, those children likely won’t have another option to get the shots, he said.
When states and the federal government passed laws linking coverage to the committee’s recommendations, they did so expecting that it would also remain an apolitical arbiter of the evidence for vaccinating the population or specific subgroups, said Cathy Bradley, dean of the Colorado School of Public Health.
Now, that premise is in doubt, and states are looking for other ways to ensure access, she said.
Allowing anyone who wants a COVID-19 vaccine to get one from the provider of their choice is an important first step for Colorado, because the vaccines remain effective in preventing severe illness, Bradley said. As the situation develops, the state will likely need to come up with other partial solutions to preserve access, she said.
“It’s a different path for everyone, depending on what your coverage is,” she said.
Sign up for our weekly newsletter to get health news sent straight to your inbox.
Meg Wingerter
Source link
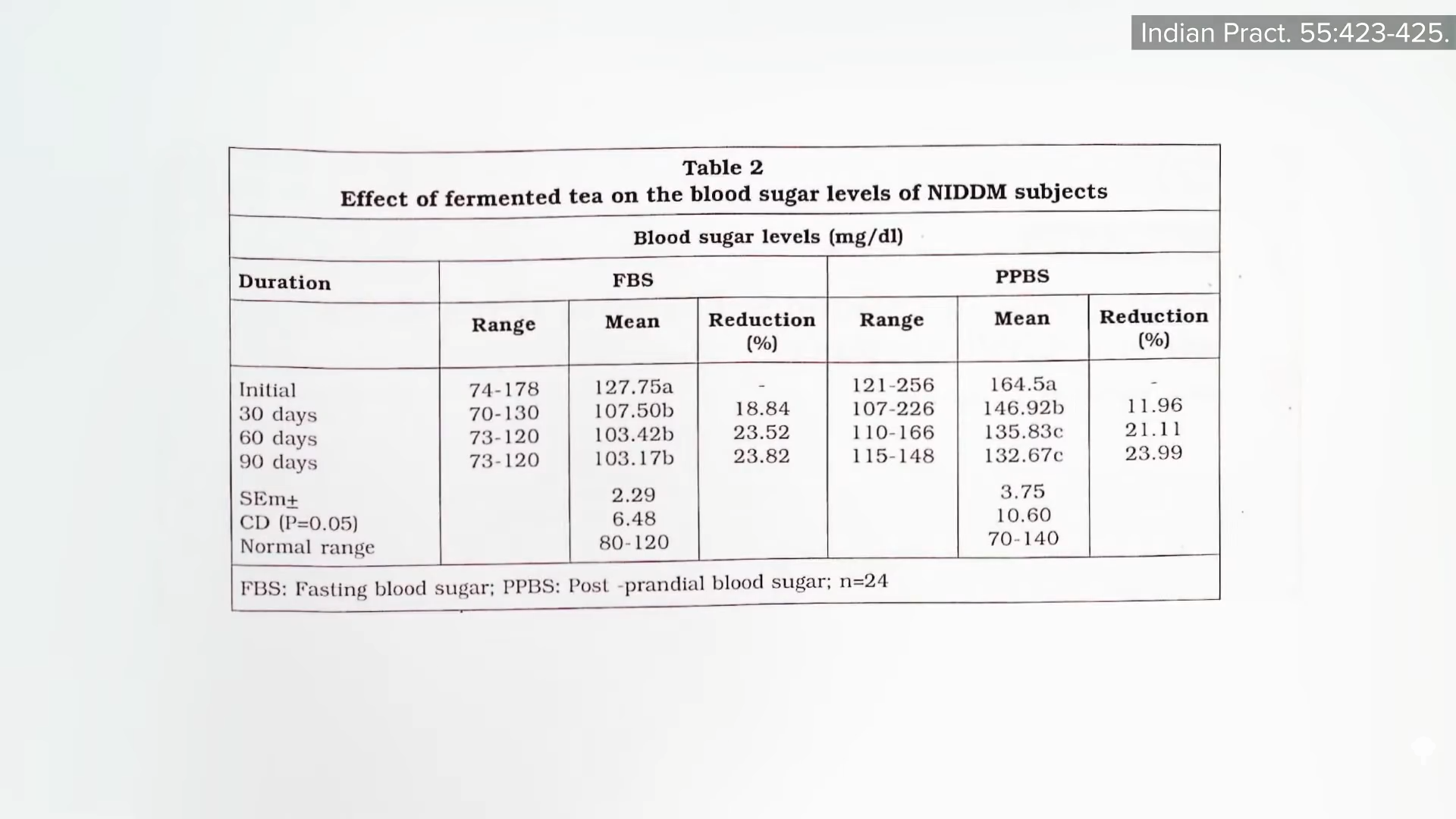
 People with diabetes were
People with diabetes were