Newswise — HOUSTON & POHANG, South Korea – The University of Texas MD Anderson Cancer Center and C-Biomex Ltd. today announced a strategic research collaboration agreement to co-develop CBT-001, a radioligand targeting the CA9 cancer biomarker.
This collaboration brings together MD Anderson’s expertise in translational radiopharmaceutical research with C-Biomex’s differentiated radioligand. The principal investigator for this project is H. Charles Manning, Ph.D., professor of Cancer Systems Imaging and director of the Cyclotron Radiochemistry Facility at MD Anderson. Under the agreement, MD Anderson and C-Biomex plan to conduct preclinical studies of CBT-001 to evaluate its potential for translation into early-phase clinical studies and to support an anticipated Investigational New Drug (IND) application with the Food and Drug Administration (FDA).
“With our global expertise in the design and discovery of differentiated peptide-ligands, Dr. Manning and the team at MD Anderson provide a perfect complement to advance the preclinical and clinical development of CBT-001,” said Cha JunHoe, Ph.D., chief executive officer of C-Biomex. “We hope this collaborative research allows us to move swiftly toward an FDA IND application and, ultimately, to an approved treatment that can benefit patients with a variety of cancers.”
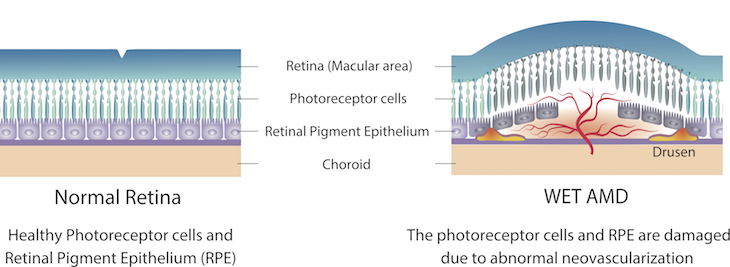
CBT-001 is a radiolabeled isotope (Lutetium-177) attached to a proprietary peptide-ligand targeting CA9 (carbonic anhydrase 9), a biomarker overexpressed in various cancers, including renal, breast and lung cancers. CBT-001’s differentiated early-stage data, generated by C-Biomex in collaboration with the Korea Institute of Radiological and Medical Sciences, represents a strong foundation for this collaborative research.
The key to success with this type of molecule is specific delivery to the tumor and rapid clearance, with minimal accumulation in healthy cells. Through this research, the collaborators will evaluate systemic and tumor-specific uptake of CBT-001 as well as antitumor efficacy and toxicology in preclinical models.
C-Biomex, leveraging its unique CUSTM peptide discovery platform technology, is developing CBT-001 and several next-generation radioligand therapies with optimal characteristics. The collaborators anticipate this research will help to inform future preclinical and early-stage clinical investigations of these next-generation therapies.
“We are pleased to align our broadly engaged theranostics research team at MD Anderson with our colleagues at C-Biomex to advance the development of CBT-001,” Manning said. “We have seen encouraging early data with this radioligand, and we look forward to collaborative work as we seek to bring impactful new treatment options to our patients in need.”
Under the terms of the agreement, C-Biomex will provide research support funding, and MD Anderson is eligible to receive certain royalties and payments based on a range of future development milestones.
Read this press release in the MD Anderson Newsroom.
-30-
About C-Biomex
C-Biomex, a private preclinical-stage biopharmaceutical company founded in 2017, is focused on developing innovative radioligand therapies with its proprietary platform technology, CUSTM (Chemistry-based Ultra-Sensitive peptide discovery). C-Biomex’s peptides have demonstrated exceptional tumor binding and selectivity with fast clearance through the renal system. The company is innovating peptides to bring better radioligand therapies to patients with cancer.
About MD Anderson
The University of Texas MD Anderson Cancer Center in Houston ranks as one of the world’s most respected centers focused on cancer patient care, research, education and prevention. The institution’s sole mission is to end cancer for patients and their families around the world, and, in 1971, it became one of the nation’s first National Cancer Institute (NCI)-designated comprehensive cancer centers. MD Anderson is No. 1 for cancer in U.S. News & World Report’s “Best Hospitals” rankings and has been named one of the nation’s top two hospitals for cancer since the rankings began in 1990. MD Anderson receives a cancer center support grant from the NCI of the National Institutes of Health (P30 CA016672).
University of Texas MD Anderson Cancer Center
Source link