Published January 11, 2026 03:00AM
The longevity industry is a loud, billion-dollar machine. Turn on any podcast, and you’re bombarded with 18-step morning routines, expensive “anti-aging” powders, and hacks that promise to rewind your biological clock. It’s enough to make you think that living a long, healthy life requires a PhD and a second mortgage.
But if you strip away the marketing and look at the actual data, the secret to longevity isn’t found in a bottle. It’s found in the produce aisle.
“The idea of ‘superfoods’ is largely a misconception used for marketing purposes,” says Dr. Matt Kaeberlein, a biologist and the CEO of Optispan, a health technology company focused on health span extension. “There is no single food with magical properties. Longevity comes from overall dietary patterns, not nutritional silver bullets.”
True longevity isn’t achieved with a list of hacks. When paired with other healthy living habits, it comes from mastering the boring, unsexy fundamentals that have kept humans alive for millennia.
Let’s explore them.
The Boring Truth About What to Eat
We love the idea of a superfood because it feels like a cheat code—eat this berry, live forever. But some of the most substantial evidence for longevity consistently points to a short list of humble staples, including legumes, whole grains, nuts, fruits, and vegetables.
A 2025 study published in Nature Medicine analyzed over 100,000 adults and found that adhering to a plant-forward diet, specifically one rich in whole grains, fruits, vegetables, and nuts, was associated with significantly better aging outcomes. The researchers noted that there wasn’t one “perfect” diet, but rather several patterns (like the Mediterranean or plant-based diets) that all shared the same DNA of minimally processed plants and healthy fats.
“If you want a single litmus test, look at how much of someone’s diet is minimally processed plant food versus ultra-processed calories,” says Dr. Anant Vinjamoori, Chief Medical Officer at Superpower, a health platform that offers proactive, personalized healthcare. “That split predicts a lot.”
Why do these simple foods work better than high-tech supplements? It’s called the food matrix. “Whole foods deliver a package: fiber, micronutrients, protein, fats, and thousands of bioactive compounds that travel together,” Vinjamoori explains. Supplements can’t replicate that synergy.
Health Fats
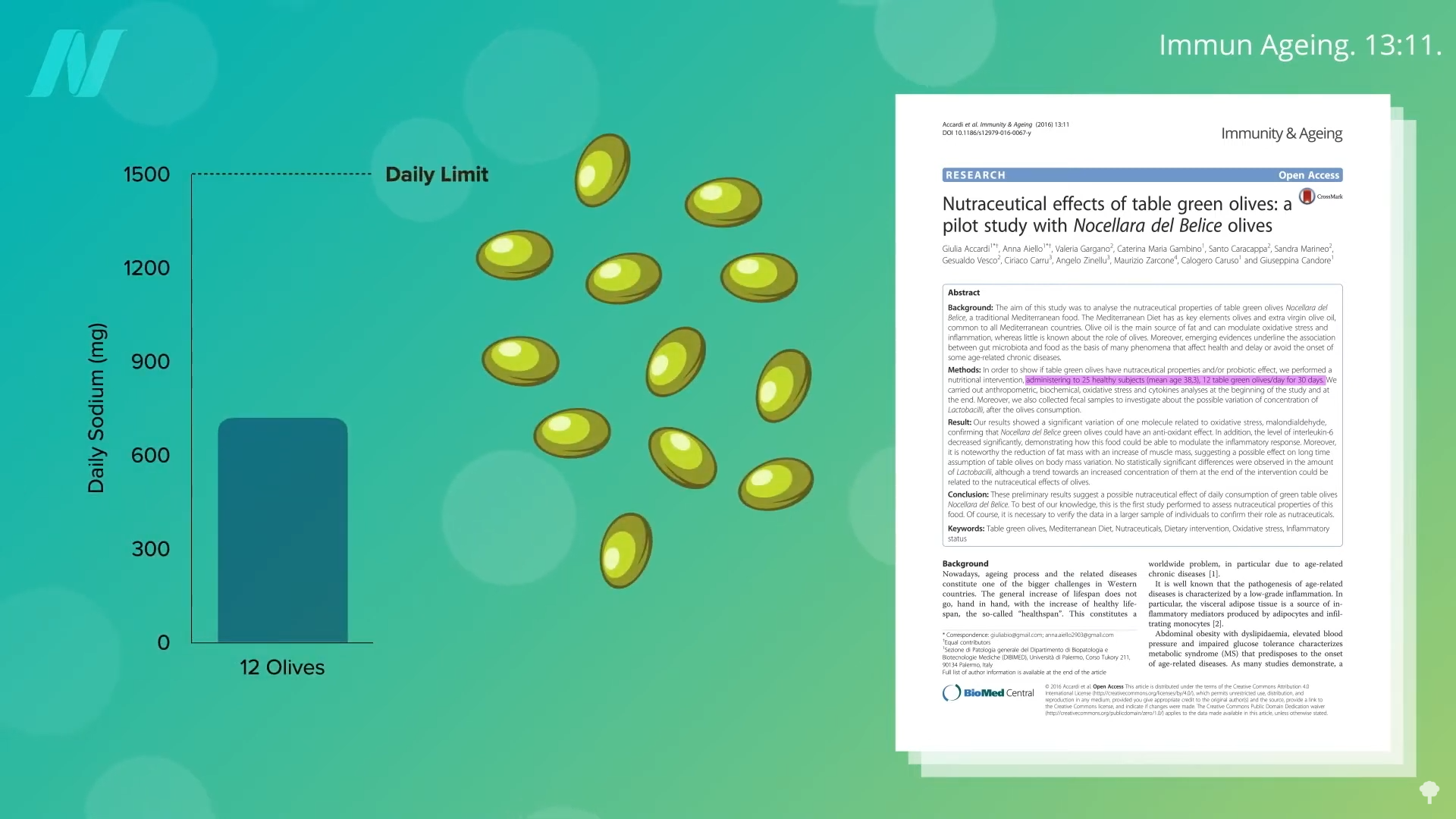
If you’re looking for a place to start, look at foods like almonds and walnuts. “Large cohort studies repeatedly associate regular nut intake with lower cardiovascular risk and reduced all-cause mortality,” says Melanie Murphy Richter, a registered dietitian and longevity expert. Beyond nuts, Richter points to extra-virgin olive oil for its anti-inflammatory properties and plant proteins like beans and lentils, which help keep cellular aging pathways balanced.
Fiber
Even humble fiber, often ignored in favor of flashy nutrients, plays a massive role. Kaeberlein explains that higher fiber intake is consistently linked to better metabolic health and longevity, recommending a target of 30 to 40 grams per day. Vinjamoori agrees, suggesting a simple, actionable goal of adding beans or lentils once a day as a simple move that improves satiety, cardiometabolic risk, and gut health.
Ultimately, the boring staples win because they work together. As Richter notes, “One ingredient can support health, but it cannot replace the whole system.”
Protein
In your twenties you might have eaten protein to build biceps, but in your fifties and beyond, getting enough can help you stay out of a nursing home. As we age, our bodies develop anabolic resistance, meaning we become less efficient at turning protein into muscle. “The same protein dose produces a weaker muscle-building signal,” says Vinjamoori. This is critical because muscle is a longevity organ; losing it puts you on a fast track to frailty and metabolic disease.
Current research, including a 2024 review in Nutrients and data published in PubMed Central, suggests that the standard recommended allowance (0.36 grams for every pound of body weight) is likely too low for optimal aging. Experts now recommend aiming higher to counteract muscle loss. A reasonable rule of thumb, according to Kaeberlein, is 0.6 to 0.9 grams of protein for every pound, combined with regular resistance training. Vinjamoori explains that while general recommendations for older adults often start lower, needs increase significantly if a person is active, recovering from illness, or trying to rebuild strength.
The source and timing of that protein matter just as much as the total amount. Richter notes that from age 18 to 65, protein from plant sources like legumes and beans appears particularly supportive of long-term health and metabolic balance. Furthermore, you shouldn’t hoard your daily intake for a massive steak dinner. “Protein quality, distribution across meals, and pairing with resistance training matter as much as total intake,” says Richter.
The ‘Blue Zone’ Reality Check
We’ve all heard the gospel of the Blue Zones—those mythical regions like Sardinia, Italy, or Okinawa, Japan, where people supposedly forget to die. Families living in these regions have in common lifestyle factors like whole-food/plant-based diets, natural movement, and strong social ties. But before you book a one-way ticket to the Mediterranean, you should know that the data might be a little… dusty.
In 2024, demographer Saul Newman was awarded an Ig Nobel Prize for highlighting a correlation between “supercentenarian” hotspots and regions with poor birth record-keeping or high rates of pension fraud. In other words, some of those 110-year-olds might just be clerical errors.
But just because the numbers are messy doesn’t mean the habits are wrong.
“Leaving aside ongoing debates about which Blue Zones are real, the consistent themes are clear,” says Kaeberlein. Whether or not everyone is hitting triple digits, the populations in these regions consistently display lower rates of chronic disease, and the mechanism isn’t genetic magic, it’s lifestyle.
Research published in the Journal of Gerontology and Geriatrics on Sardinian longevity highlights that the secret is actually a combination of factors, including a plant-forward diet, constant low-level physical activity (like walking and gardening), and strong family bonds. Basically, living in an environment that discourages sitting still and eating processed junk.
The Transferrable Lessons
You don’t need to live in an Italian village to replicate the biological benefits. The research points to a few specific transferables.
Eat a Plain Diet. Across these regions, the menu is remarkably consistent. It is high in whole foods, legumes, and whole grains, and low in ultra-processed foods. A review of longevity diets found that these patterns work by reducing inflammation and improving metabolic health, often mimicking the effects of caloric restriction without the hunger.
Don’t Eat Alone. In North America, we often view food as fuel to be consumed at a desk. In longevity hotspots, meals are social anchors. “Isolation is not a longevity strategy,” warns Vinjamoori. “Social eating matters.” The data supporting this shows that strong social capital is a primary driver of successful aging in these zones, helping to buffer stress and improve mental well-being.
Prioritize Deliciousness. Sustainability is key. As Registered Dietitian Ashley Koff, nutrition course director at the University of California, Irvine says, if your longevity diet tastes like cardboard, you won’t stick to it long enough to see your great-grandkids. “One of the core pillars of longevity eating is ‘better be delicious to me,’” says Koff. The Mediterranean diet works largely because it is enjoyable—rich in fats like olive oil and diverse flavors—making it a pattern people want to maintain for decades.
“The lesson isn’t to copy a specific cuisine,” Kaeberlein says “but to apply those principles within your own cultural context.”
What About Fasting and Supplements?
If you’re hoping a pill or a fasting window will help you retain a heavier lifestyle, the experts say otherwise.
“Fasting and time-restricted eating are not inherently longevity-promoting,” states Kaeberlein. While they can be useful tools to stop you from snacking on junk at midnight, they don’t replace food quality.
As for supplements, “They’re best for correcting a deficiency or treating a defined risk factor,” Vinjamoori says. Unless you have a specific medical need, your money is likely better spent on high-quality groceries. The exceptions worth discussing with your doctor are Omega-3s, Vitamin D, and creatine, which Kaeberlein calls “one of the most evidence-supported supplements” for maintaining muscle and cognitive function.
The Long Game
Longevity isn’t a six-week challenge or a guru-promoted biohacking stack. It’s a practice.
“I genuinely prefer a salmon salad to a cheeseburger and fries,” Kaeberlein admits, noting that taste buds adapt over time.
The best diet for longevity is simply the one you can stick to for the next 50 years. So, start small. Swap a processed snack for an apple. Add a scoop of lentils to your soup. “Do it consistently, then build from there,” Vinjamoori advises.
The goal isn’t just to live longer. It’s to live better—and that starts with what’s on your plate today.