If the microbiome of those eating plant-based diets protects against the toxic effects of TMAO, what about swapping gut flora?
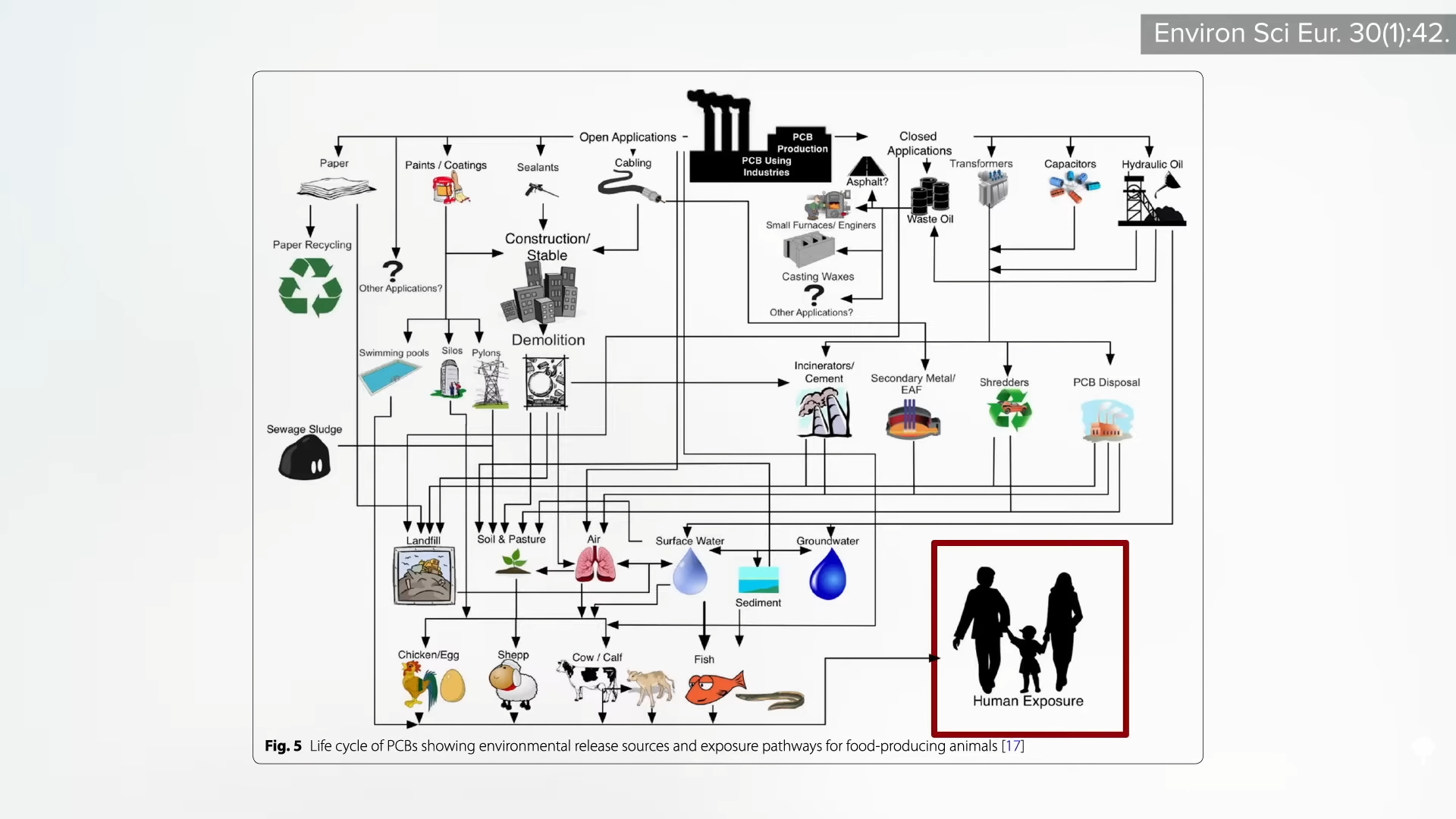
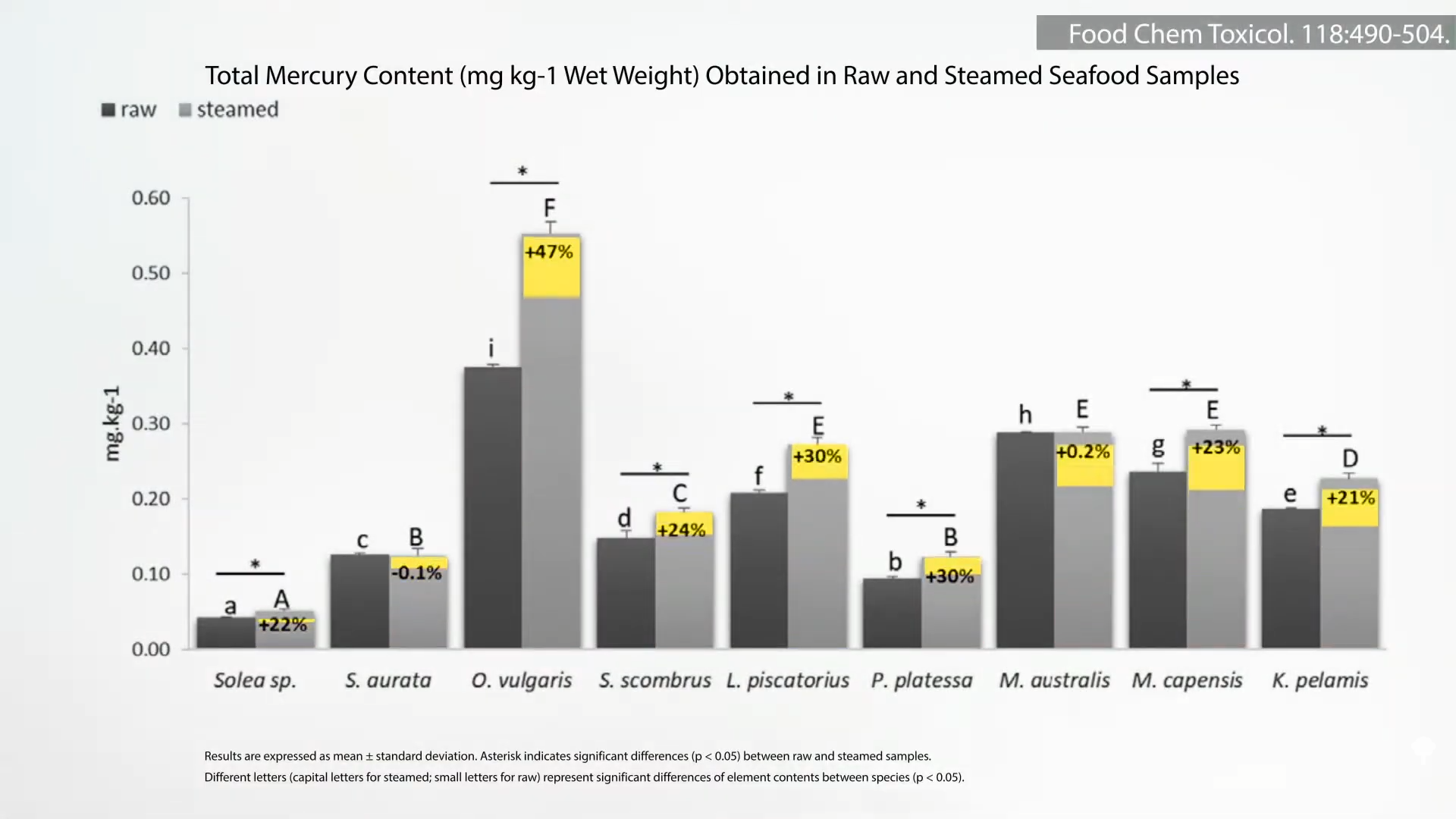
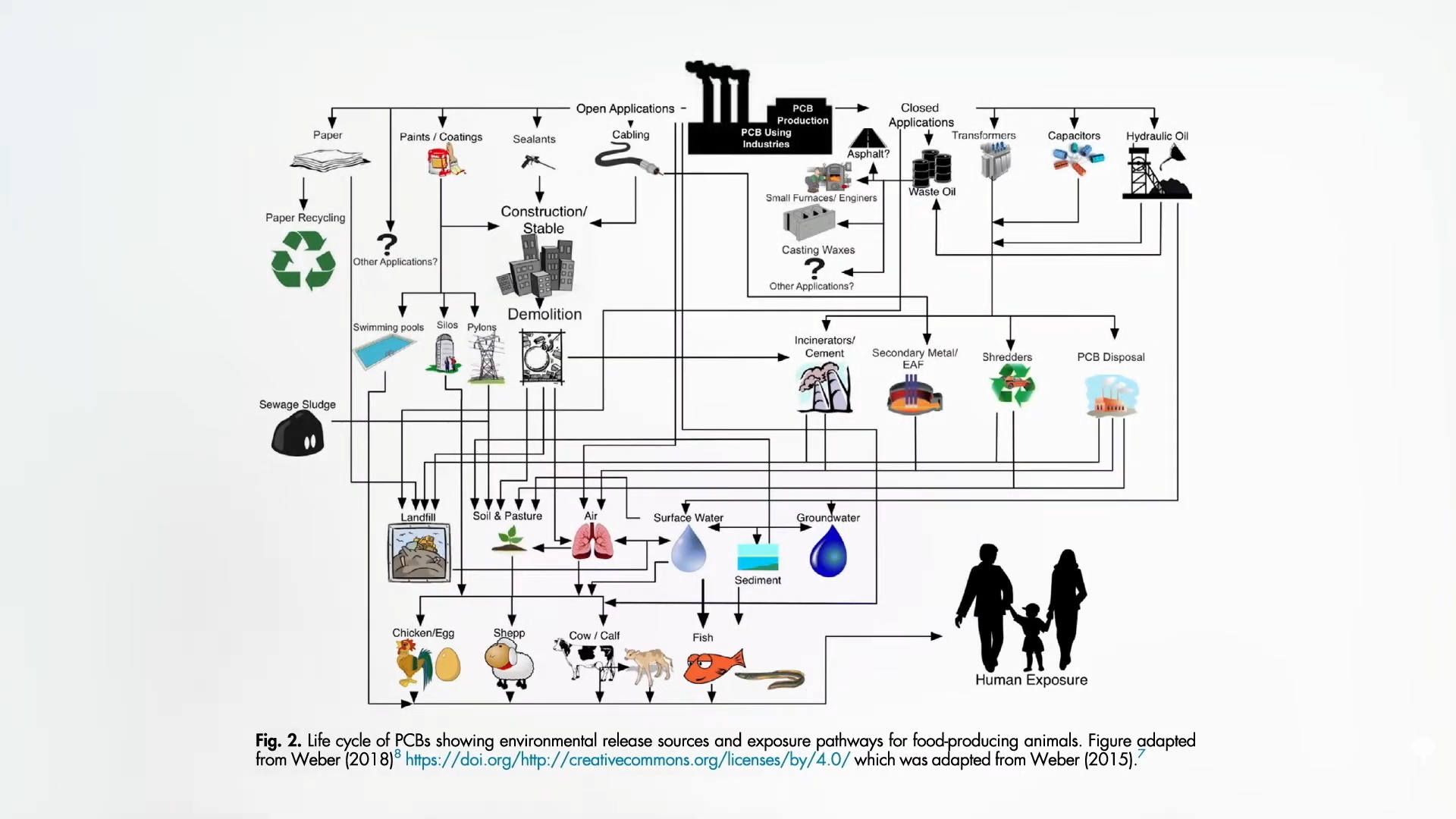
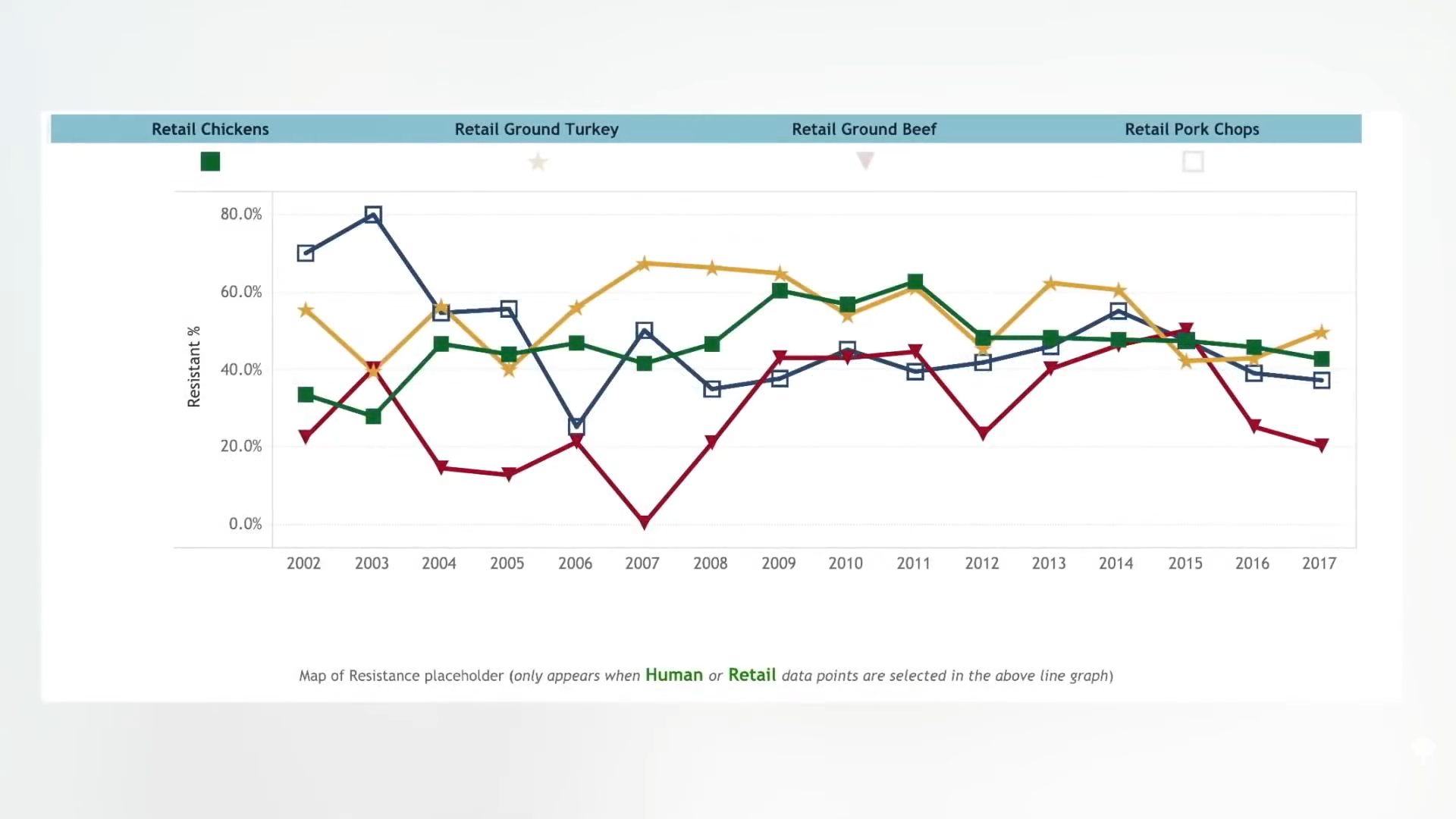
“Almost 2,500 years ago, Hippocrates stated that ‘All disease begins in the gut.’” When we feed our gut bacteria right with whole plant foods, they feed us right back with beneficial compounds like butyrate, which our gut bugs make from fiber. On the other hand, if we feed them wrong, they can produce detrimental compounds like TMAO, which they make from cheese, eggs, seafood, and other meat.
We used to think that TMAO only contributed to cardiovascular diseases, like heart disease and stroke, but, more recently, it has been linked to psoriatic arthritis, associated with polycystic ovary syndrome, and everything in between. I’m most concerned about our leading killers, though. Of the top ten causes of death in the United States, we’ve known about its association with increased risk of heart disease and stroke, killers number one and five, but recently, an association has also been found between blood levels of TMAO and the risks of various cancers, which are our killer number two. The link between TMAO and cancer could be attributed to the inflammation caused by TMAO, but it could also be oxidative stress (free radicals), DNA damage, or a disruption in protein folding.
What about our fourth leading killer, chronic obstructive pulmonary disease (COPD), like emphysema? TMAO is associated with premature death in patients with exacerbated COPD, though it’s suspected that it’s due to them dying from more cardiovascular disease.
The link to stroke is a no-brainer—no pun intended. It is due to the higher blood pressure associated with higher TMAO levels, as well as the greater likelihood of clots forming in those with atrial fibrillation. Those with higher TMAO levels also appear to have worse strokes and four times the odds of death.
Killer number six is Alzheimer’s disease. Can TMAO even get up into our brains? Yes, TMAO is present in human cerebrospinal fluid, which bathes the brain, and TMAO levels are higher in those with mild cognitive dysfunction and those with Alzheimer’s disease dementia. “In the brain, TMAO has been shown to induce neuronal senescence [meaning, deterioration with age], increase oxidative stress, impair mitochondrial function, and inhibit mTOR signaling, all of which contribute to brain aging and cognitive impairment.”
Killer number seven is diabetes, and people with higher TMAO levels are about 50% more likely to have diabetes. Killer number eight is pneumonia, and TMAO predicts fatal outcomes in pneumonia patients even without evident heart disease. Kidney disease is killer number nine, and TMAO is strongly related to kidney function and predicts fatal outcomes there as well. Over a period of five years, more than half of chronic kidney disease patients who started out with average or higher TMAO levels were dead, whereas among those in the lowest third of levels, nearly 90% remained alive.
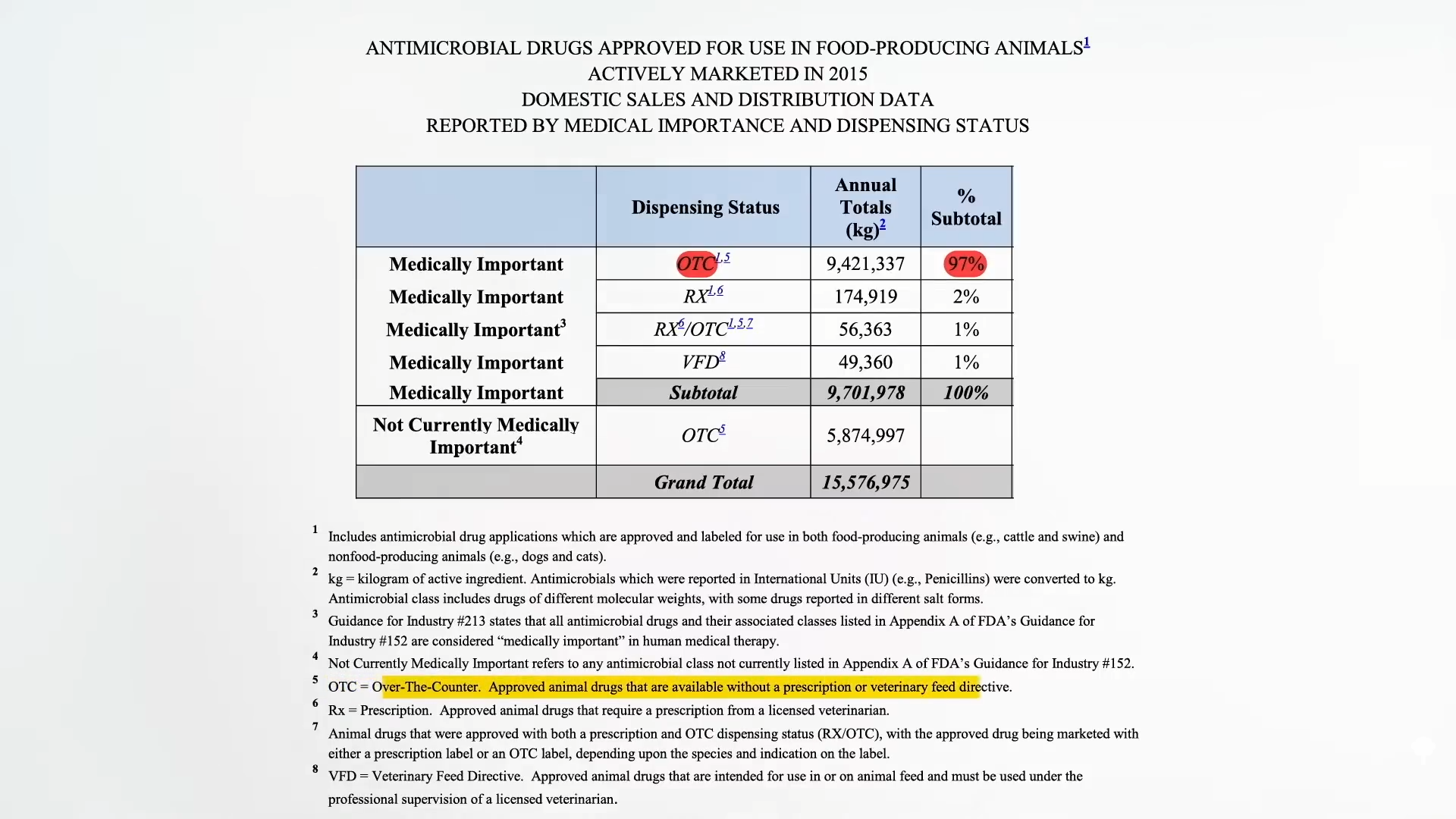
How can we lower the TMAO levels in our blood? Because TMAO originates from dietary sources, we could limit our intake of choline- and carnitine-rich foods. They’re so widespread in foods,” though we’re talking about meat, eggs, and dairy. “Therefore, restriction of foods rich in TMA-containing nutrients may not be practical.” Can we just get a vegan fecal transplant? “Vegan donors provided the investigators with a fresh morning fecal sample…”
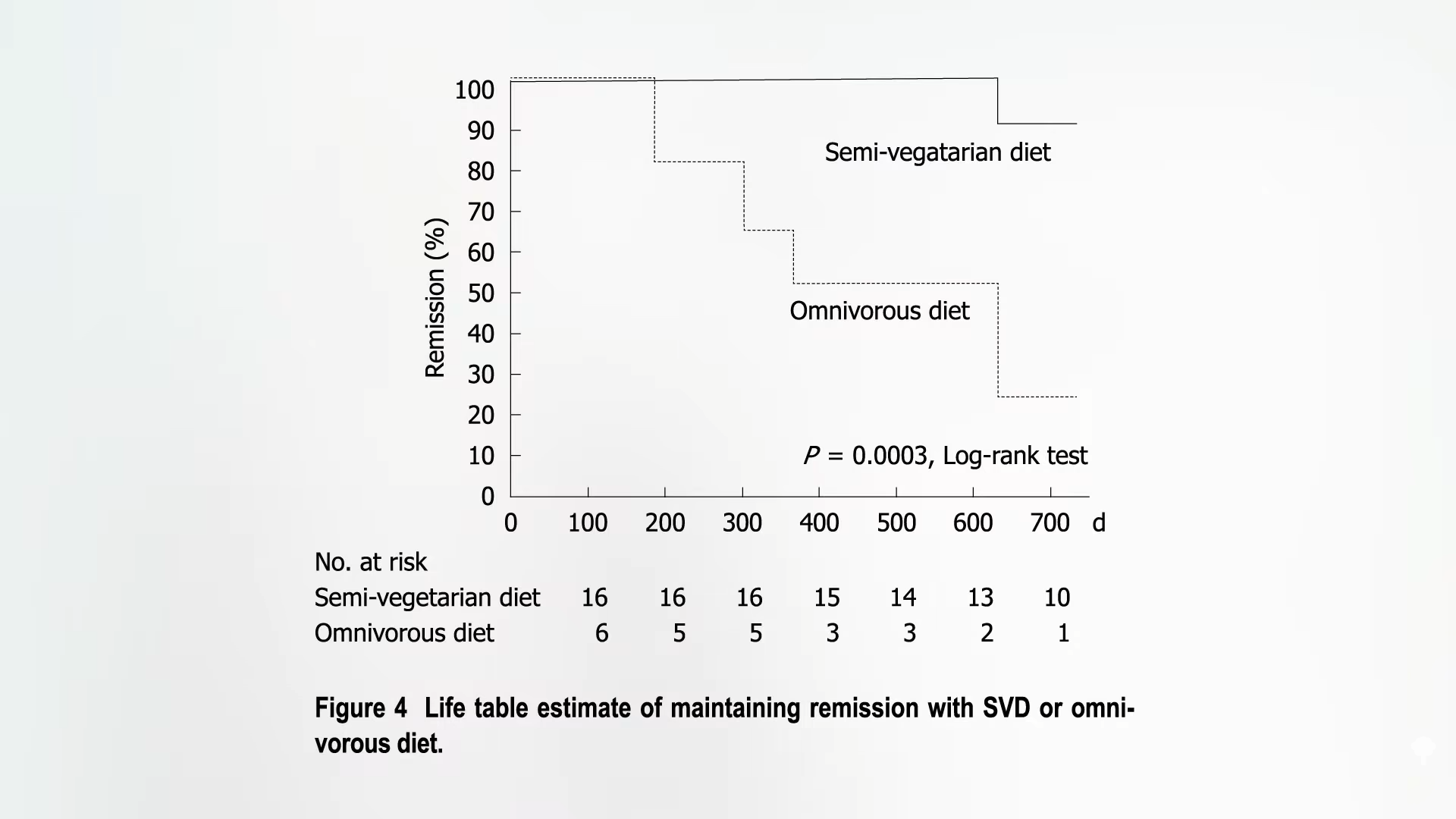
If you remember, if you give a vegan a steak, despite all that carnitine, they make almost no TMAO compared to a meat-eater, presumably because the vegan hasn’t been fostering steak-eating bugs in their gut. See below and at 3:40 in my video Can Vegan Fecal Transplants Lower TMAO Levels?.
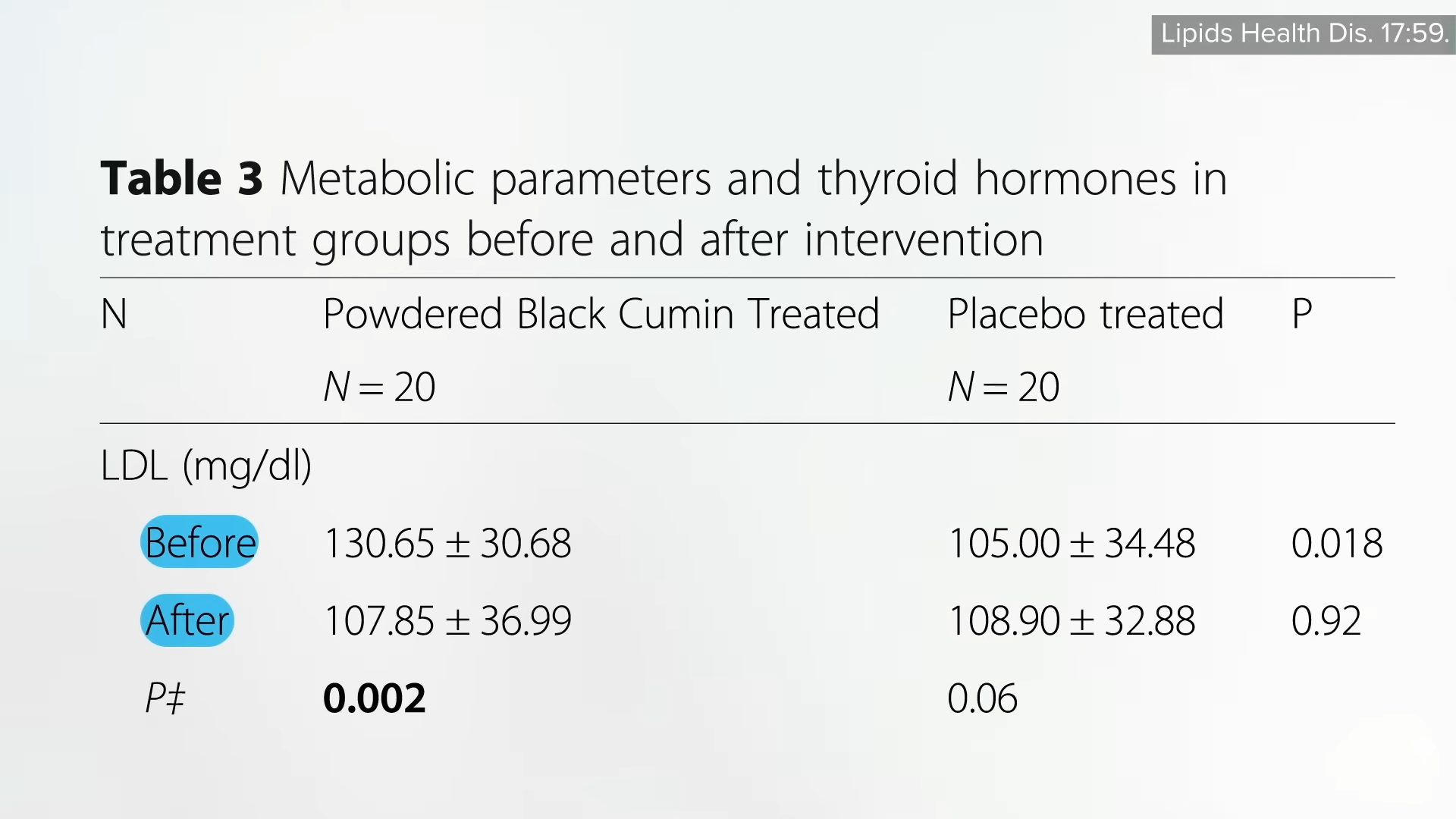
Remarkably, even if you give plant-based eaters the equivalent of a 20-ounce steak every day for two months, only about half start ramping up production of TMAO, showing just how far their gut flora has to change. The capacity of veggie feces to churn out TMAO is almost nonexistent. Instead of eating healthier, what about getting some vegan poop?
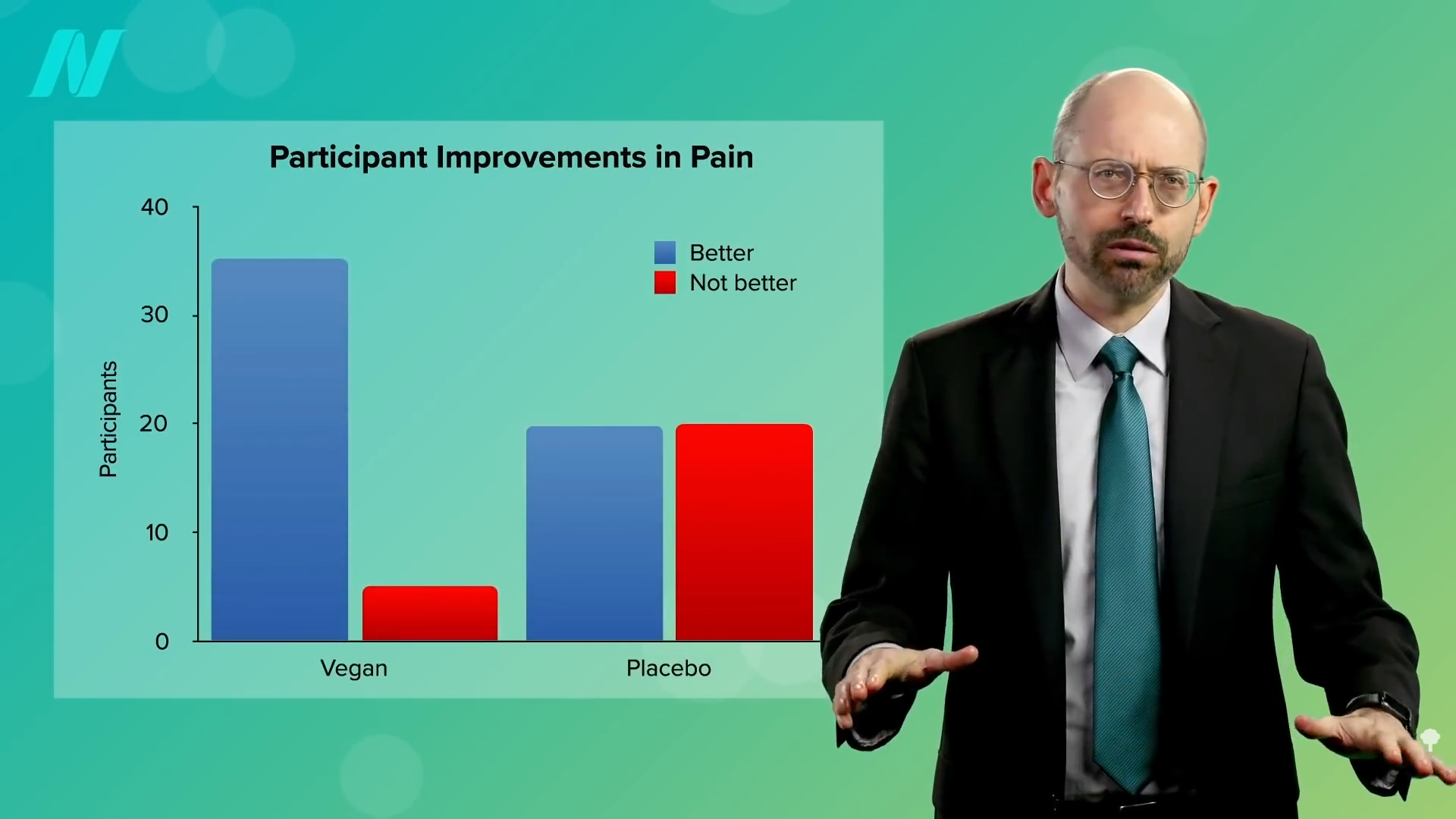
In a double-blind, randomized, controlled trial, research subjects either got vegan poop or their own poop back through a hose snaked down their nose, and it didn’t work.
First of all, the vegans recruited for the study started out making TMAO themselves, in contrast to the other study, where they didn’t make any at all. This may be because the earlier study required the vegans to have been vegan for at least a year, and this study didn’t. So, there wasn’t much of a change in TMAO running through their bodies two weeks after getting the vegan poop, but the vegan poop they got seemed to start out with some capacity to produce TMAO in the first place.
So, the failure to improve after the vegan fecal transplant “could be related to limited baseline microbiome differences and continuation of an omnivorous diet” after the vegan-donor transplant. What’s the point of trying to reset your microbiome if you’re just going to eat meat? Well, the researchers didn’t want to switch people to a plant-based diet since they knew that alone can change our microbiome, and they didn’t want to introduce any extra factors. The bottom line is that it seems there may not be any shortcuts. We may just have to eat a healthier diet.
Doctor’s Note
Want to become a donor? Find out How to Become a Fecal Transplant Super Donor.
For more on TMAO, check out related posts below.
See the microbiome topic page for even more.
Michael Greger M.D. FACLM
Source link