Dog parents see their fair share of emergency cases. But here’s the good news: being informed about common emergencies can help you stay calm and take the right actions when your dog needs you most. Here are some situations you should be aware of.
When Your Dog’s Belly Becomes a Ticking Time Bomb
Bloat, or gastric dilatation-volvulus (GDV), is a life-threatening condition in which a dog’s stomach fills with gas and potentially twists on itself. Large, deep-chested breeds are especially prone. Watch for symptoms like a swollen abdomen, unsuccessful attempts to vomit, and restlessness. If you suspect bloat, it’s crucial to get to a vet immediately – this is a true emergency where every minute counts.
When Fun in the Sun Turns Dangerous
Dogs can’t sweat like we do, making them vulnerable to overheating. Signs of heatstroke include excessive panting, drooling, reddened gums, vomiting, and collapse. If you suspect heatstroke, move your dog to a cool area immediately, offer small amounts of water, and use cool (not cold) water to wet their coat. Then, head to the vet right away.
Curiosity Can Be Toxic
Dogs are curious creatures, sometimes to their detriment. Common toxins include chocolate, xylitol (found in sugar-free gum), grapes and raisins, onions, and certain plants. Symptoms of poisoning vary but can include vomiting, diarrhea, seizures, or collapse. If you suspect your dog has ingested something toxic, call your vet or a pet poison helpline immediately.
When Accidents Happen
Whether it’s a car accident, a fall, or a fight with another animal, trauma can lead to serious injuries. Look for signs like limping, bleeding, swelling, or changes in behavior. Even if external injuries aren’t apparent, internal damage could be present. When in doubt, a vet visit is always the safest decision.
When Your Dog’s Brain Short-Circuits
Witnessing your dog have a seizure can be terrifying. During a seizure, clear the area around your dog to prevent injury, and never put your hand near their mouth. Time the seizure if possible. Once it’s over, keep your dog calm and call your vet. If the seizure lasts more than five minutes or your dog has multiple seizures, it’s time for immediate veterinary care.
When Something’s Stuck
If your dog is choking, they may paw at their mouth, gag, or have difficulty breathing. For a conscious dog, you can try gently removing the object if you can see it. If you can’t, or if your dog loses consciousness, perform the canine Heimlich maneuver and rush to the vet.
The Bottom Line: Be Prepared, Not Scared
While these situations are scary, remember that knowledge and quick action can make all the difference. Keep your vet’s number and the nearest emergency vet clinic’s information easily accessible. Consider taking a pet first aid course to feel more confident in handling emergencies.
Remember, you’re your dog’s first line of defense in an emergency. By staying informed and prepared, you’re giving your best friend the best chance at a quick recovery should the unexpected occur. Here’s to happy, healthy adventures with your canine companion!
Post Views: 104
Animal Wellness is North America’s top natural health and lifestyle magazine for dogs and cats, with a readership of over one million every year. AW features articles by some of the most renowned experts in the pet industry, with topics ranging from diet and health related issues, to articles on training, fitness and emotional well being.
Animal Wellness
Source link








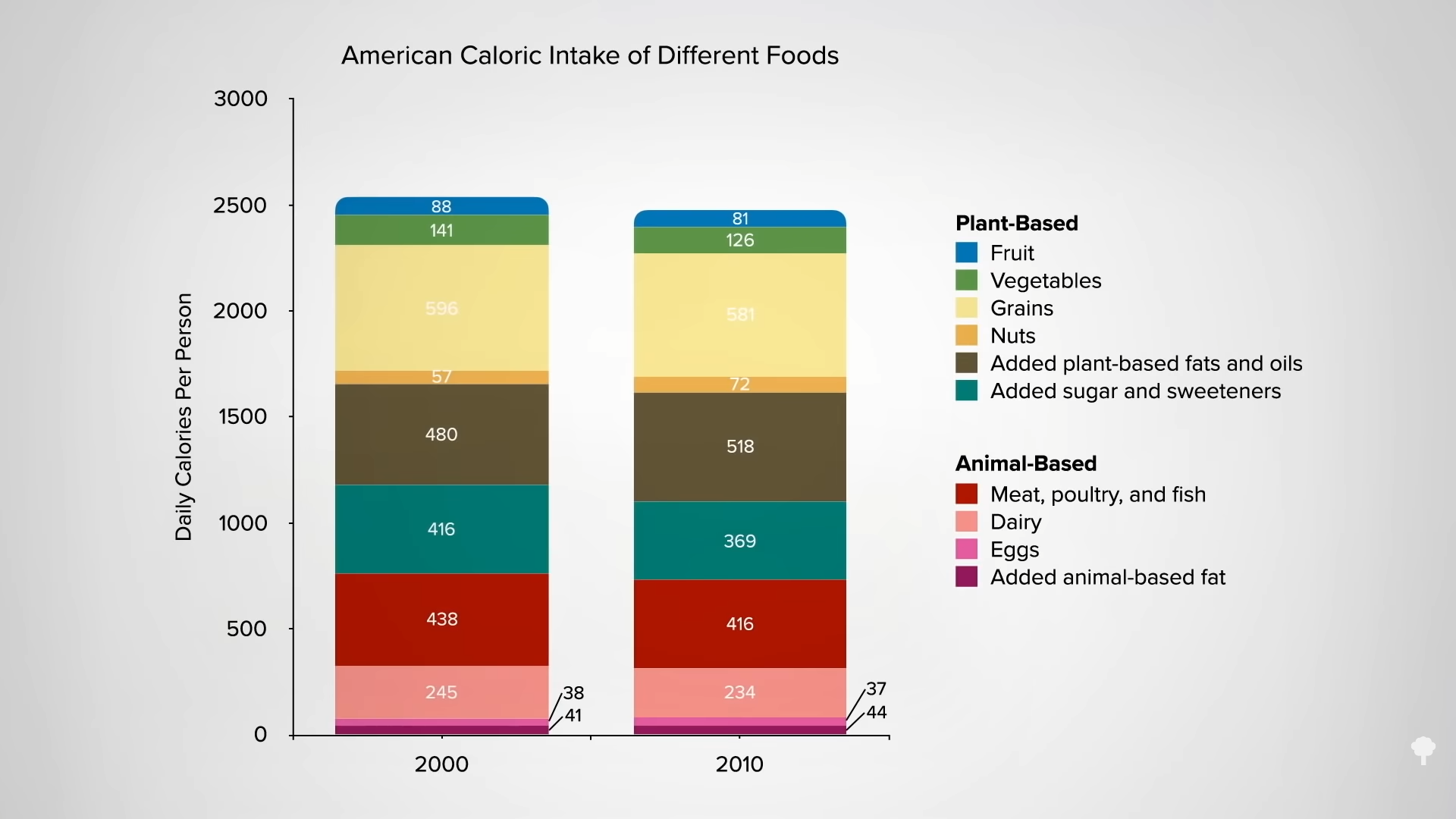 Low-carb diets cut down on refined grains and added sugars, and low-fat diets tend to cut down on added fats and meat, so they both tell people to cut down on donuts. Any diet that does that already has a leg up. I figure a don’t-eat-anything-that-starts-with-the-letter-D diet could also successfully cause weight loss if it caused people to cut down on donuts, danishes, and Doritos, even if it makes no nutritional sense to exclude something like dill.
Low-carb diets cut down on refined grains and added sugars, and low-fat diets tend to cut down on added fats and meat, so they both tell people to cut down on donuts. Any diet that does that already has a leg up. I figure a don’t-eat-anything-that-starts-with-the-letter-D diet could also successfully cause weight loss if it caused people to cut down on donuts, danishes, and Doritos, even if it makes no nutritional sense to exclude something like dill.