[ad_1]
What were the results of a randomized, double-blind, placebo-controlled trial of a daily half teaspoon of powdered black cumin in Hashimoto’s patients?
“Autoimmune thyroiditis, also known as Hashimoto’s thyroiditis, is an organ-specific autoimmune disorder,” where our body attacks our own thyroid gland, often leading to hypothyroidism due to destruction and scarring of the gland itself. We know there’s a genetic component, since identical twins are more likely to share the disease than fraternal twins. “However, even with identical twins, the concordance rate was only about 50%, emphasizing that important factors such as the environment play a role in disease pathogenesis.” Indeed, even if your identical twin, who has basically your exact same DNA, has the disease, there’s only like a flip of a coin’s chance you’ll get it. Genes load the gun, but the environment may pull the trigger.
More than 90 synthetic chemicals were noted to show disruption of hormonal balance or thyroid dysfunction.” However, only a few such ‘pollutants show evidence that they contribute to autoimmune thyroid disease.” These include polyaromatic hydrocarbons. Smokers get a lot of them from cigarettes, but in nonsmokers, exposure comes almost entirely from food, as you can see below and at 1:18 in my video Diet for Hypothyroidism: A Natural Treatment for Hashimoto’s Disease.
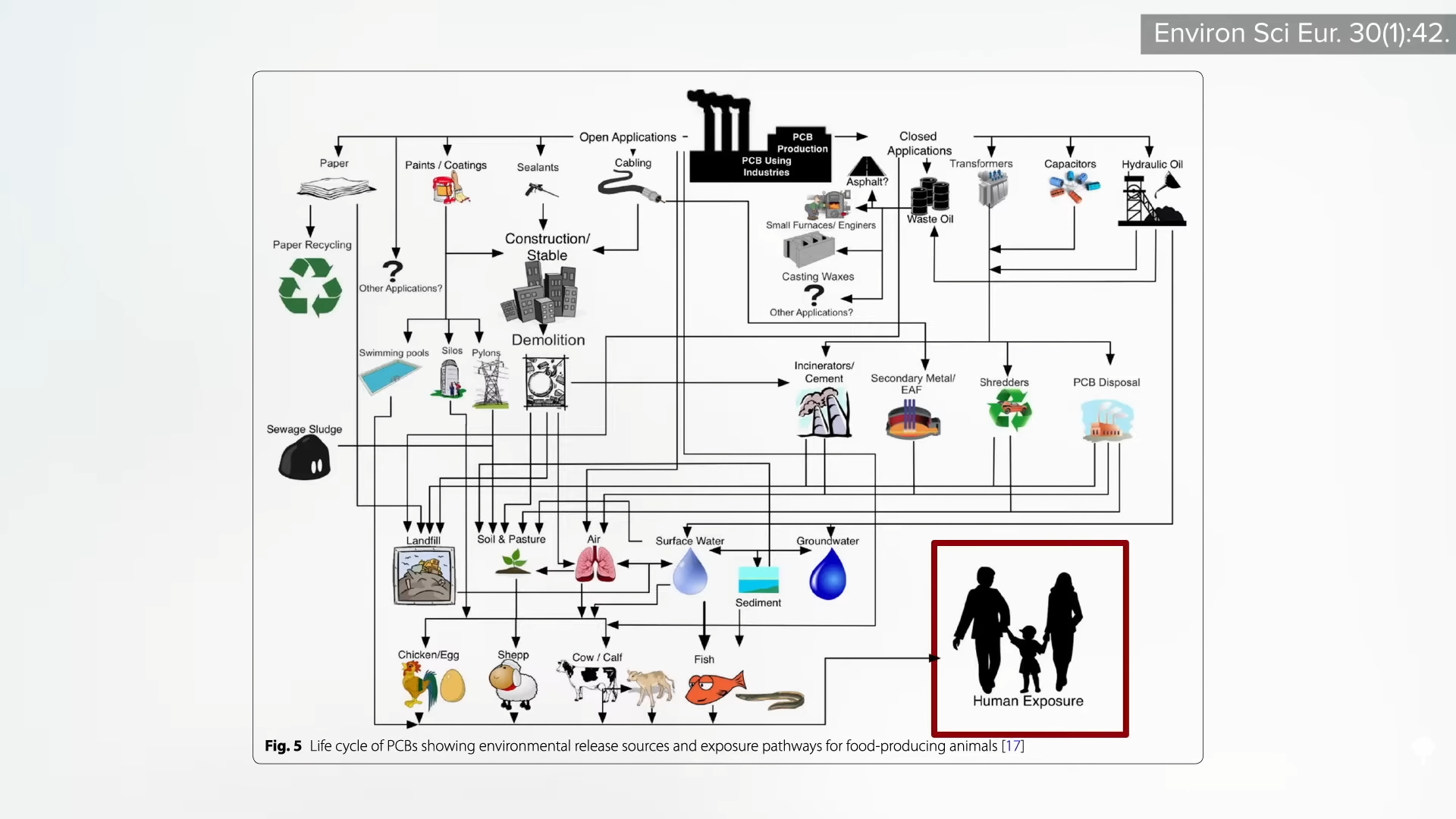
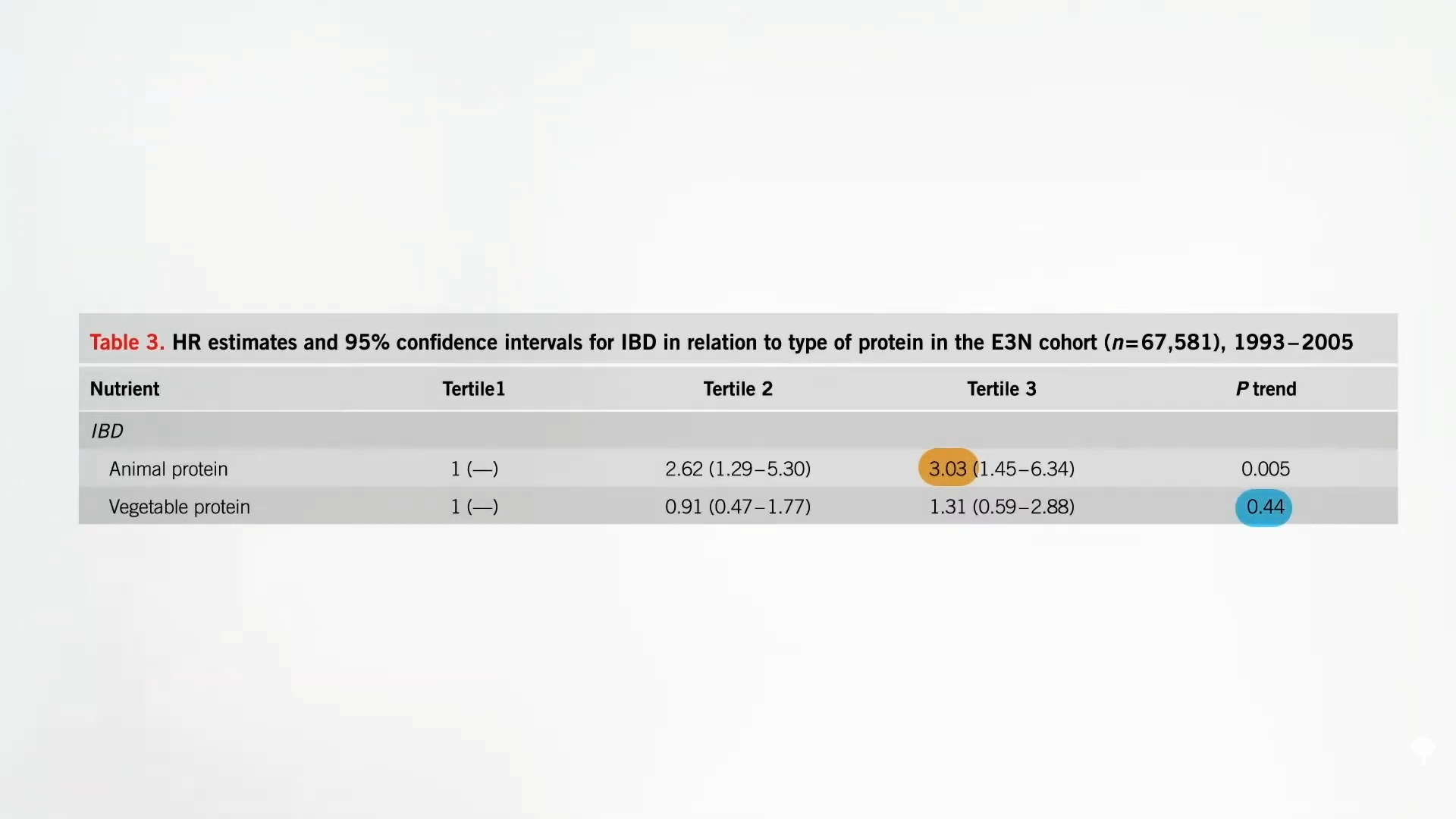
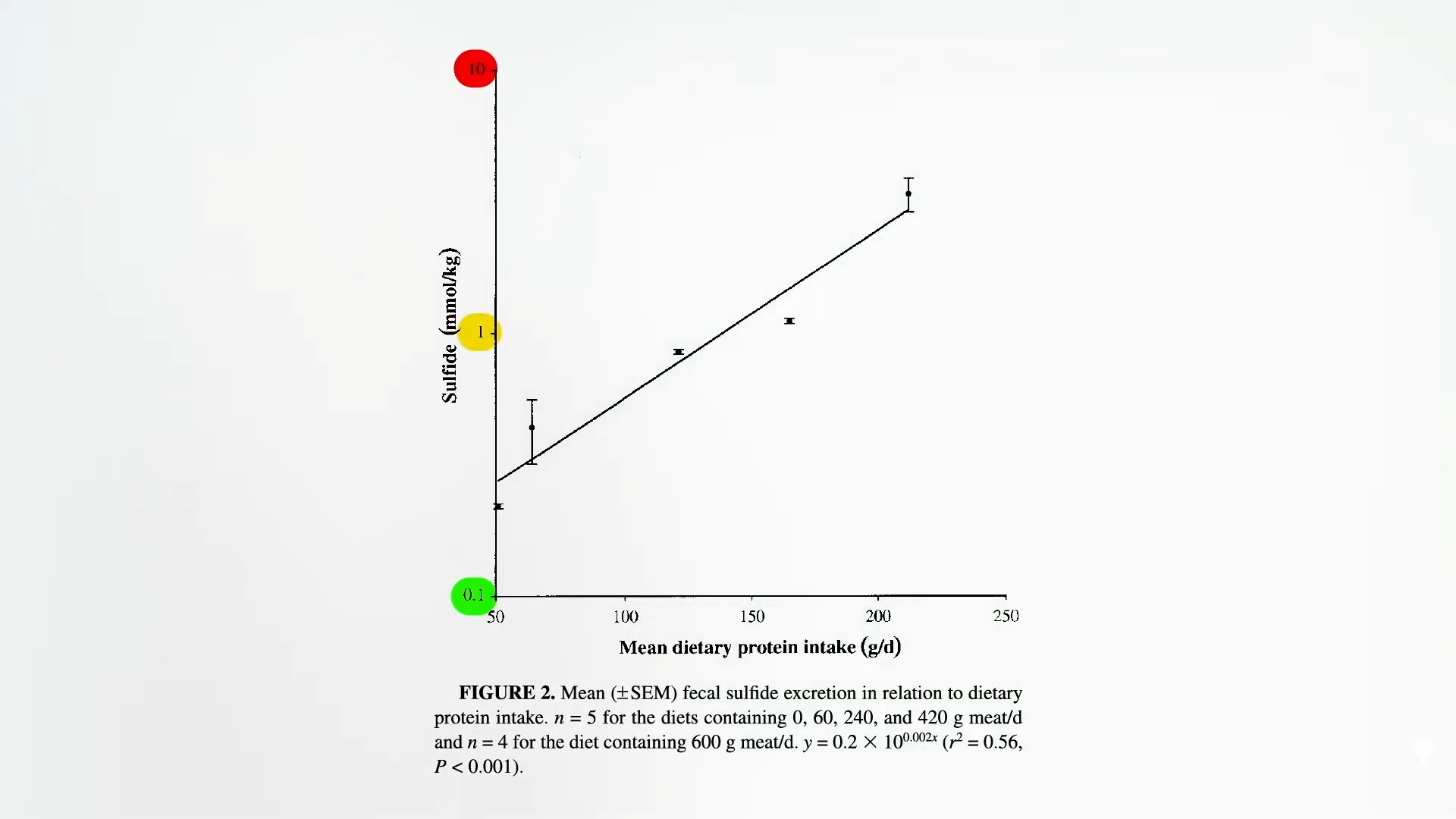
Polycyclic aromatic hydrocarbons are primarily formed when muscle meats, such as beef, pork, fish, or chicken, are cooked using high-temperature methods, such as grilling. PBBs, polybrominated biphenols, are a type of flame-retardant chemical no longer manufactured in the United States, but are still found in the aquatic food chain. PCBs, polychlorinated biphenols, are used in a number of industrial processes and end up in people’s bodies, again, largely through the consumption of fish, but also eggs and other meats, as seen here and at 1:41 in my video.
So, one might suspect those eating plant-based diets would have lower rates of hypothyroidism, and, indeed, despite their lower iodine intake, vegan diets tended to be protective. But they’ve never been put to the test in an interventional trial. A modification of the Paleolithic diet has been tried in Hashimoto’s patients, but it didn’t appear to improve thyroid function. What did, though, is Nigella Sativa. That name should sound familiar to anyone who’s read my book How Not to Diet or watched my live Evidence-Based Weight Loss presentation. Nigella Sativa is the scientific name for black cumin, which is just a simple spice that’s also used for a variety of medicinal purposes.
In one study, Hashimoto’s patients received a half teaspoon of powdered black cumin every day for eight weeks in a randomized, double-blind, placebo-controlled trial. Not only was there a significant reduction in body weight, which is why I profiled it in my book, but the black cumin also significantly reduced the thyroid-stimulating hormone, a sign that thyroid function was improving. It even lowered the level of autoimmune anti-thyroid antibodies, as well as increased blood levels of thyroid hormone T3 in these Hashimoto’s patients. In addition, there was a significant drop in Interleukin 23, a proinflammatory cell signal thought to help promote the autoimmune inflammation of the thyroid, which “further confirms the anti-inflammatory nature of the plant.” And what were the side effects? There was a 17 percent drop in “bad” LDL cholesterol, as shown below and at 3:19 in my video.
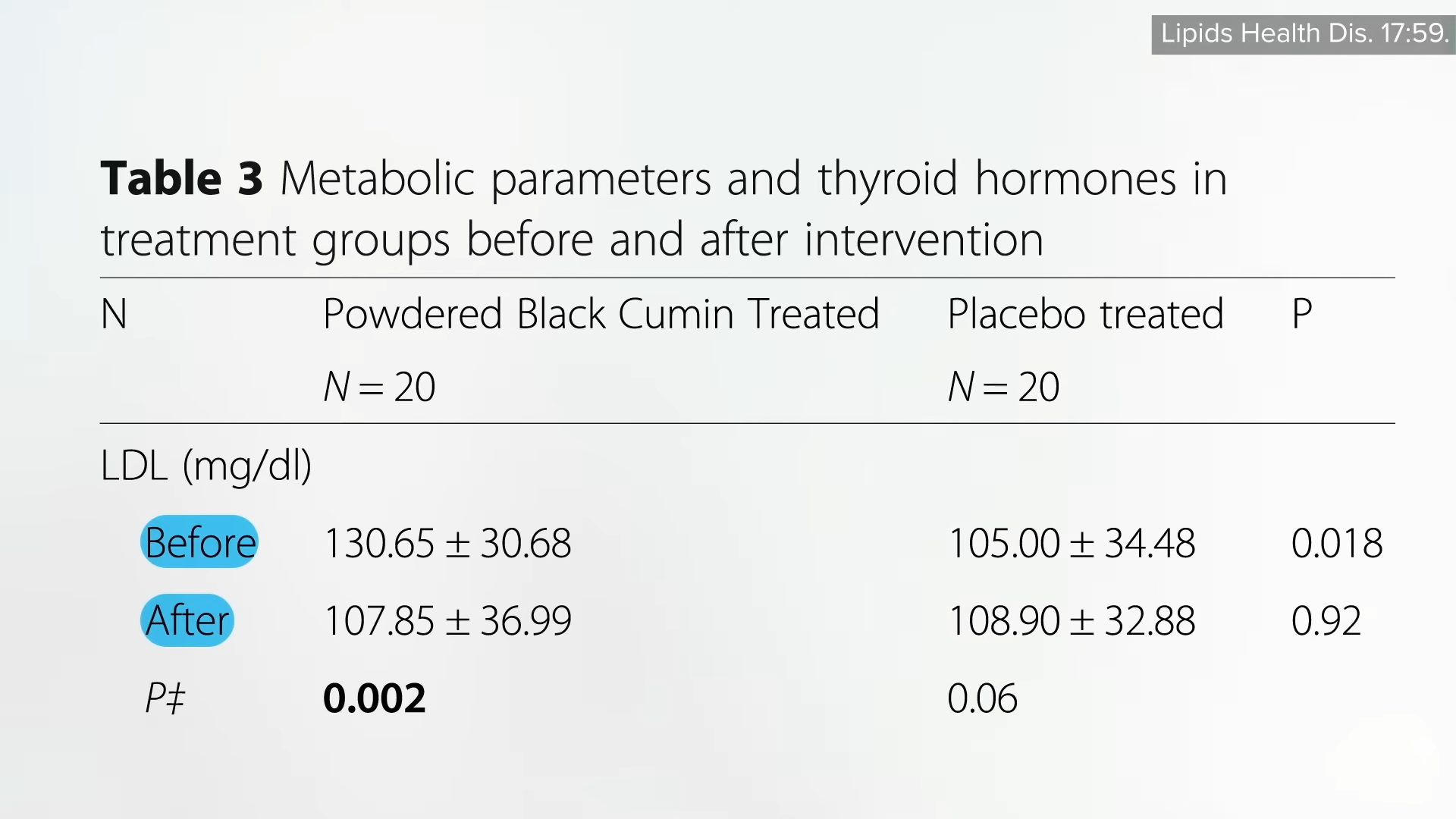
Given the fact that patients with Hashimoto’s may be at particularly high risk of developing heart disease, this is exactly the kind of side effects we’d want. “Considering these health-promoting effects of N. Sativa [black cumin], it can be considered as a therapeutic approach in the management of Hashimoto-related metabolic abnormalities.”
A similar trial failed to find a benefit, though. Same dose, same time frame, but no significant changes in thyroid function. In contrast with the previous study, though, the study participants were not all Hashimoto’s patients, but rather hypothyroid for any reason, and that may have diluted the results. And it’s possible that telling patients to take the black cumin doses with their thyroid hormone replacement therapy may have interfered with its absorption, which is an issue similar to other foods and drugs, and why patients are normally told to take it on an empty stomach. Since there are no downsides—it’s just a simple spice—I figure, why not give it a try? The worst that can happen is you’ll have tastier food.
Doctor’s Note:
I get a lot of questions about thyroid function, and I am glad to have been able to do this series. If you missed any of the other videos, see the related posts below.
For more on black cumin, see my book How Not to Diet and my presentation Evidence-Based Weight Loss.
[ad_2]
Michael Greger M.D. FACLM
Source link



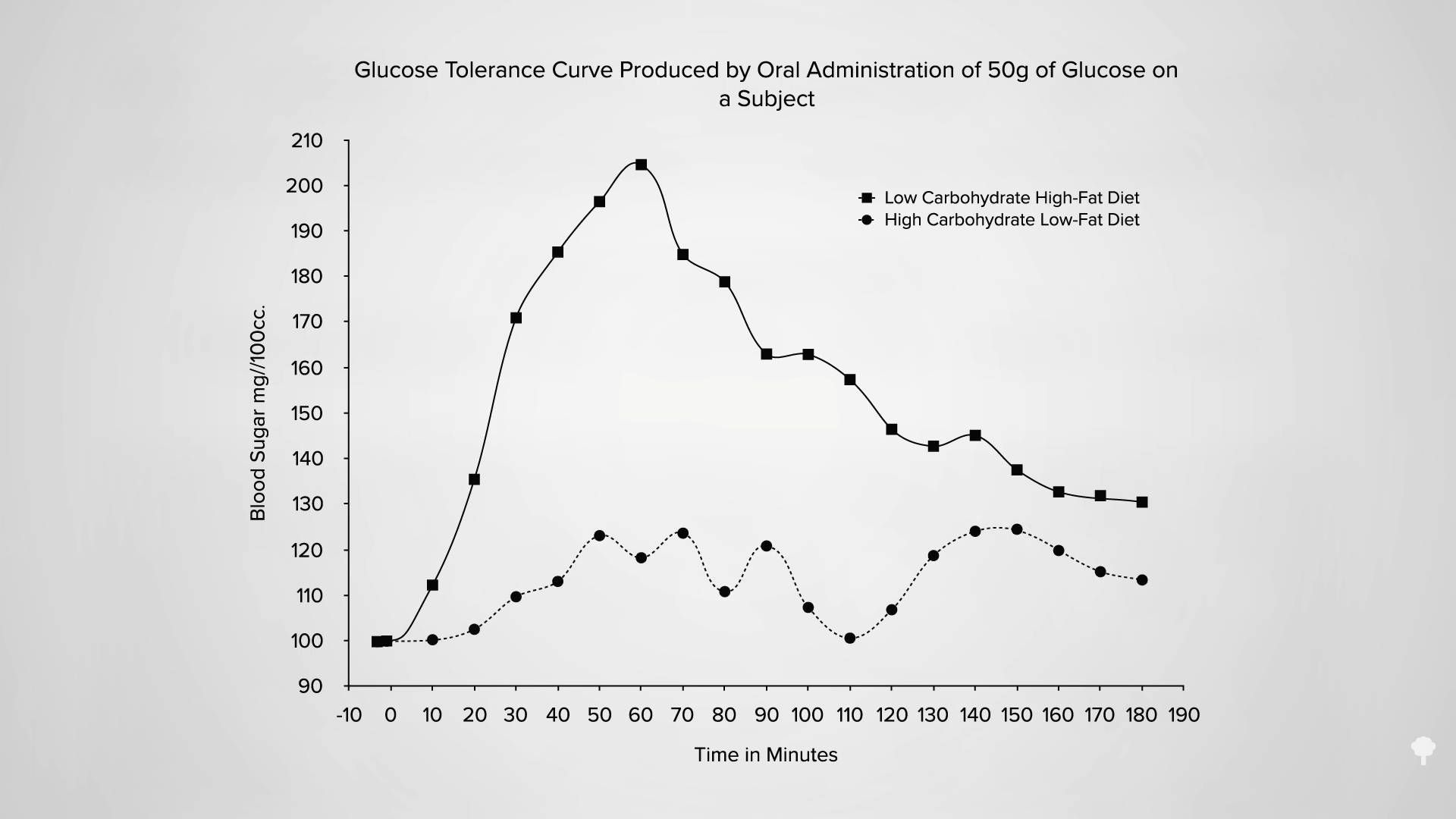
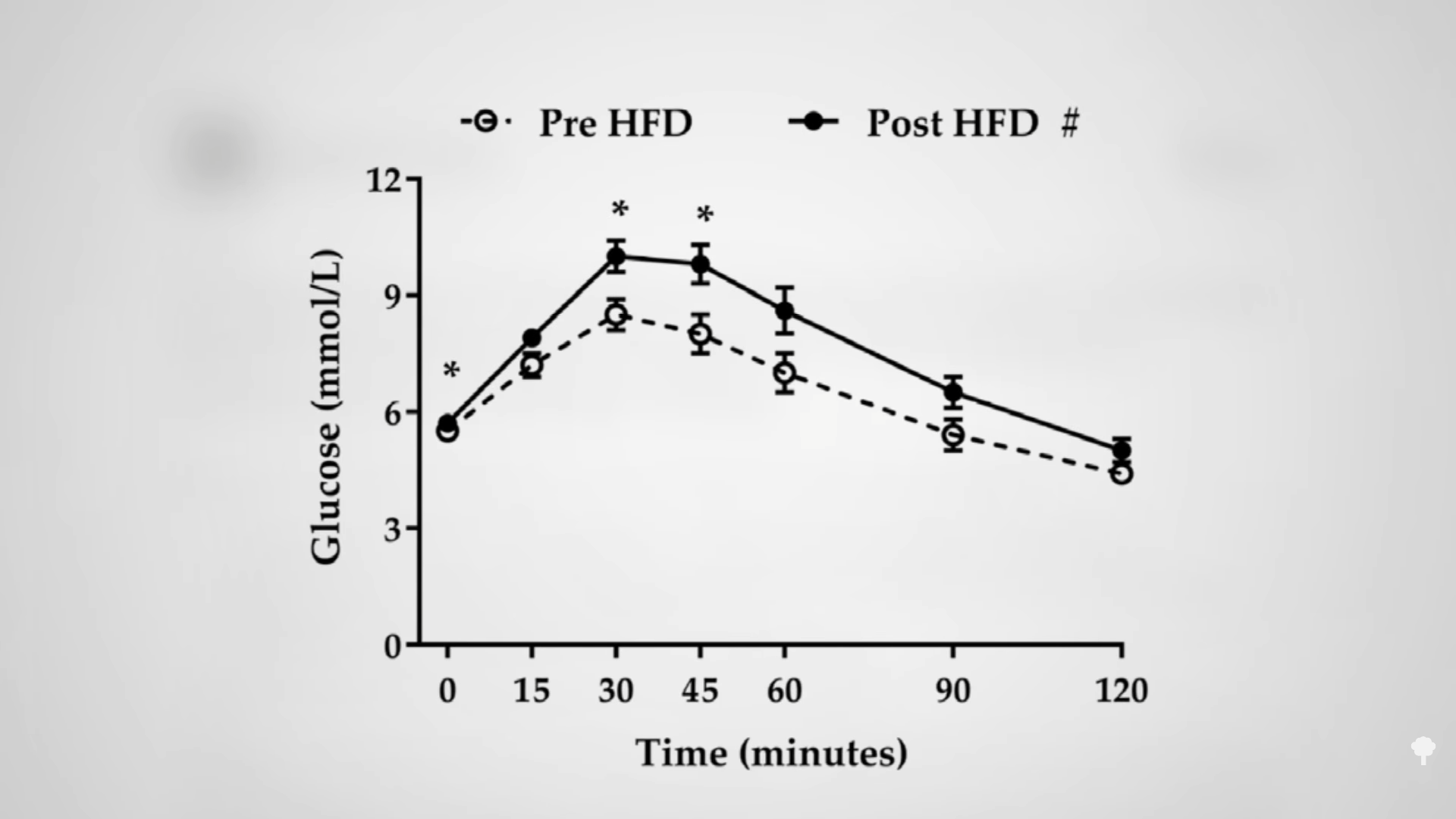
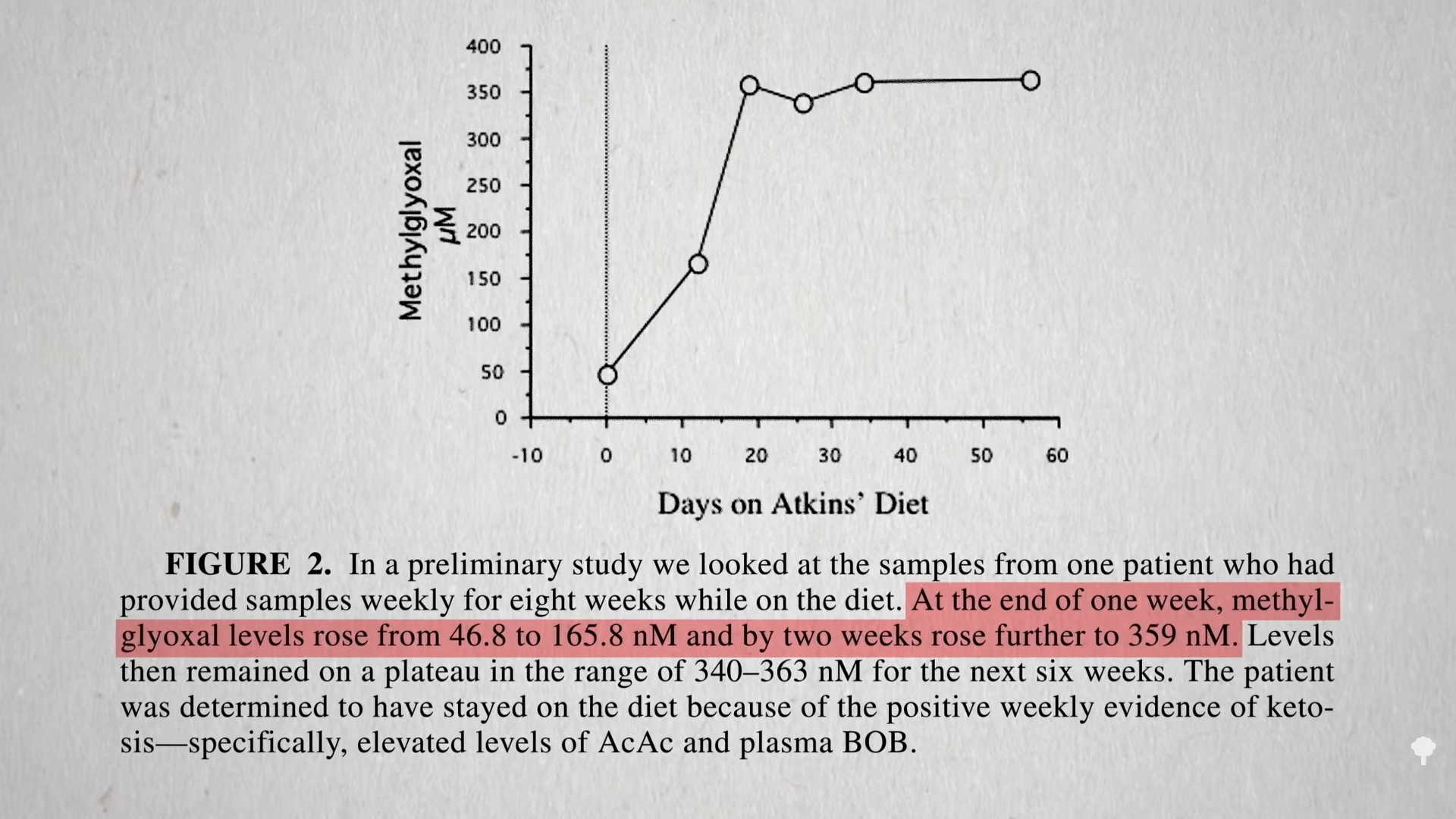
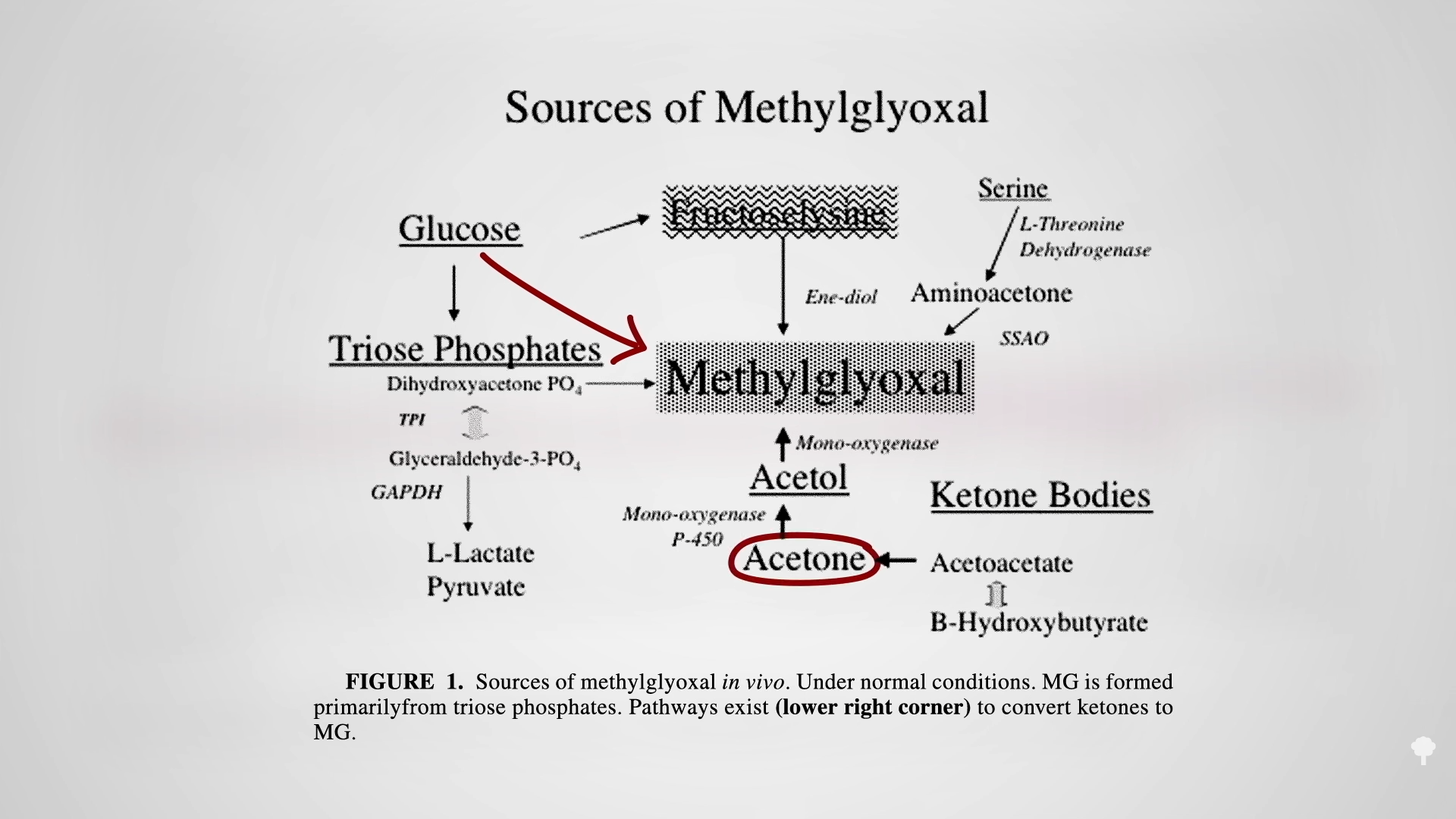
 The irony doesn’t stop there. One of the reasons people with diabetes suffer such nerve and artery damage is due to an inflammatory metabolic toxin known as methylglyoxal, which forms at high blood sugar levels. Methylglyoxal
The irony doesn’t stop there. One of the reasons people with diabetes suffer such nerve and artery damage is due to an inflammatory metabolic toxin known as methylglyoxal, which forms at high blood sugar levels. Methylglyoxal 

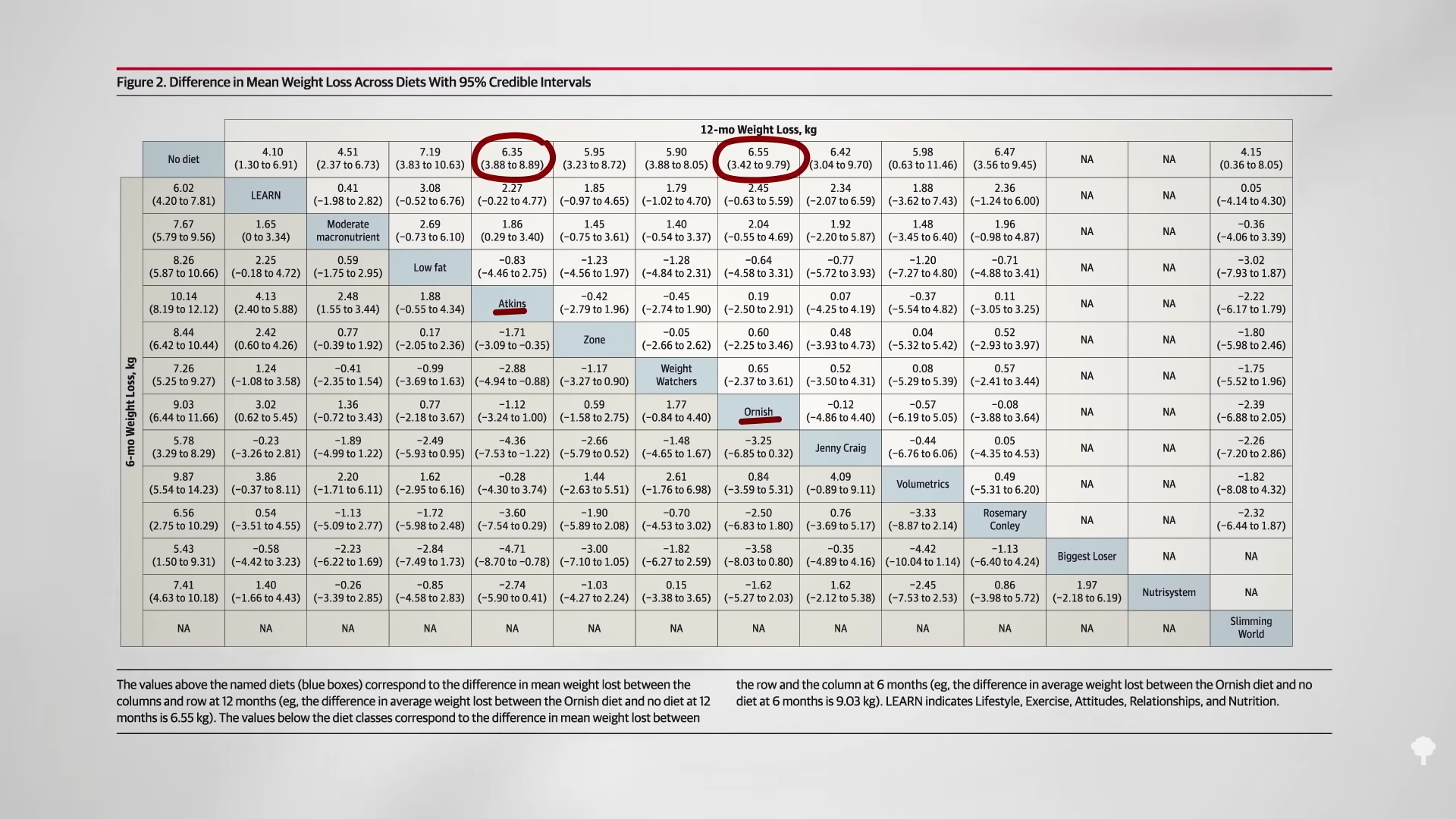


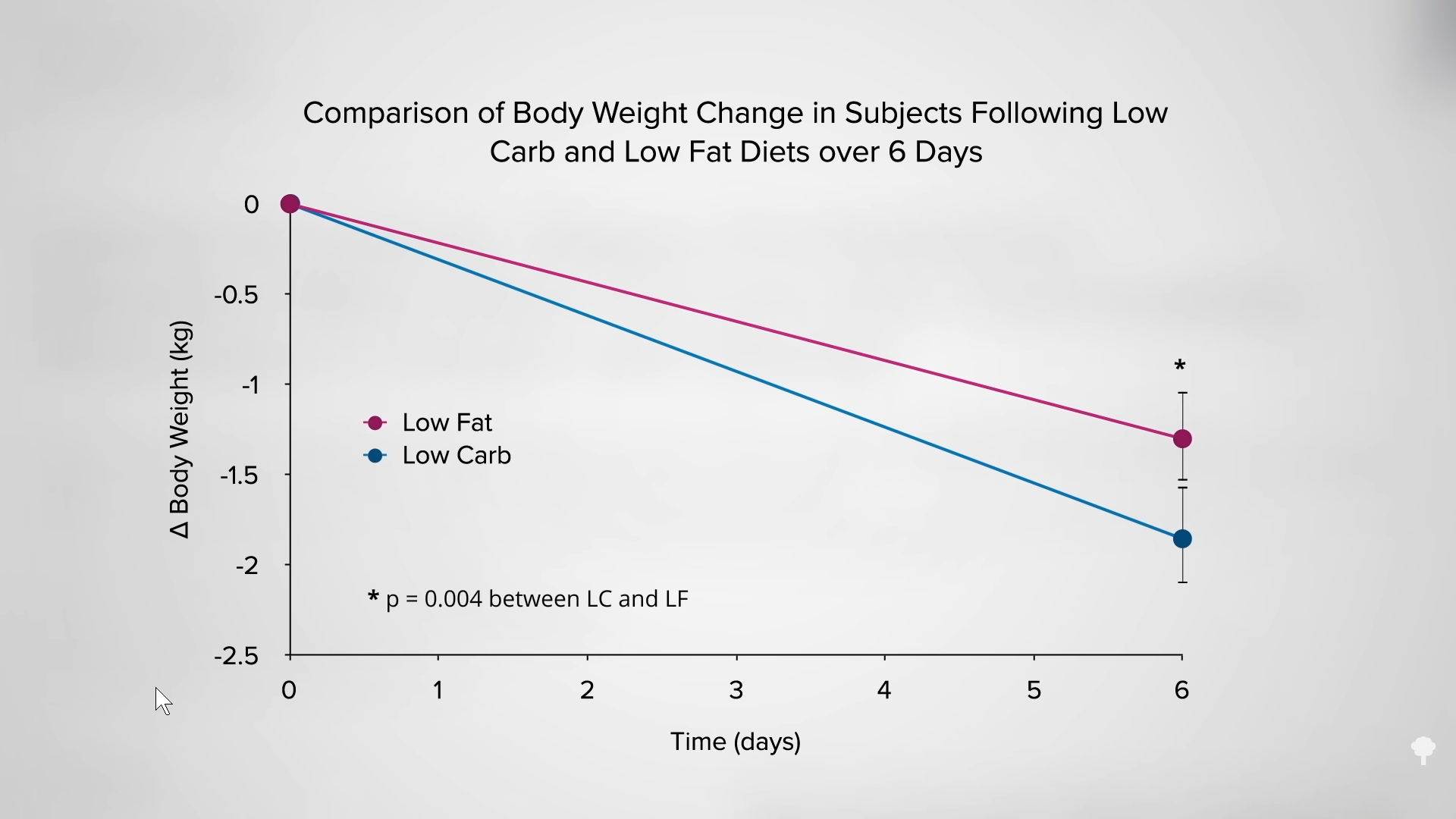
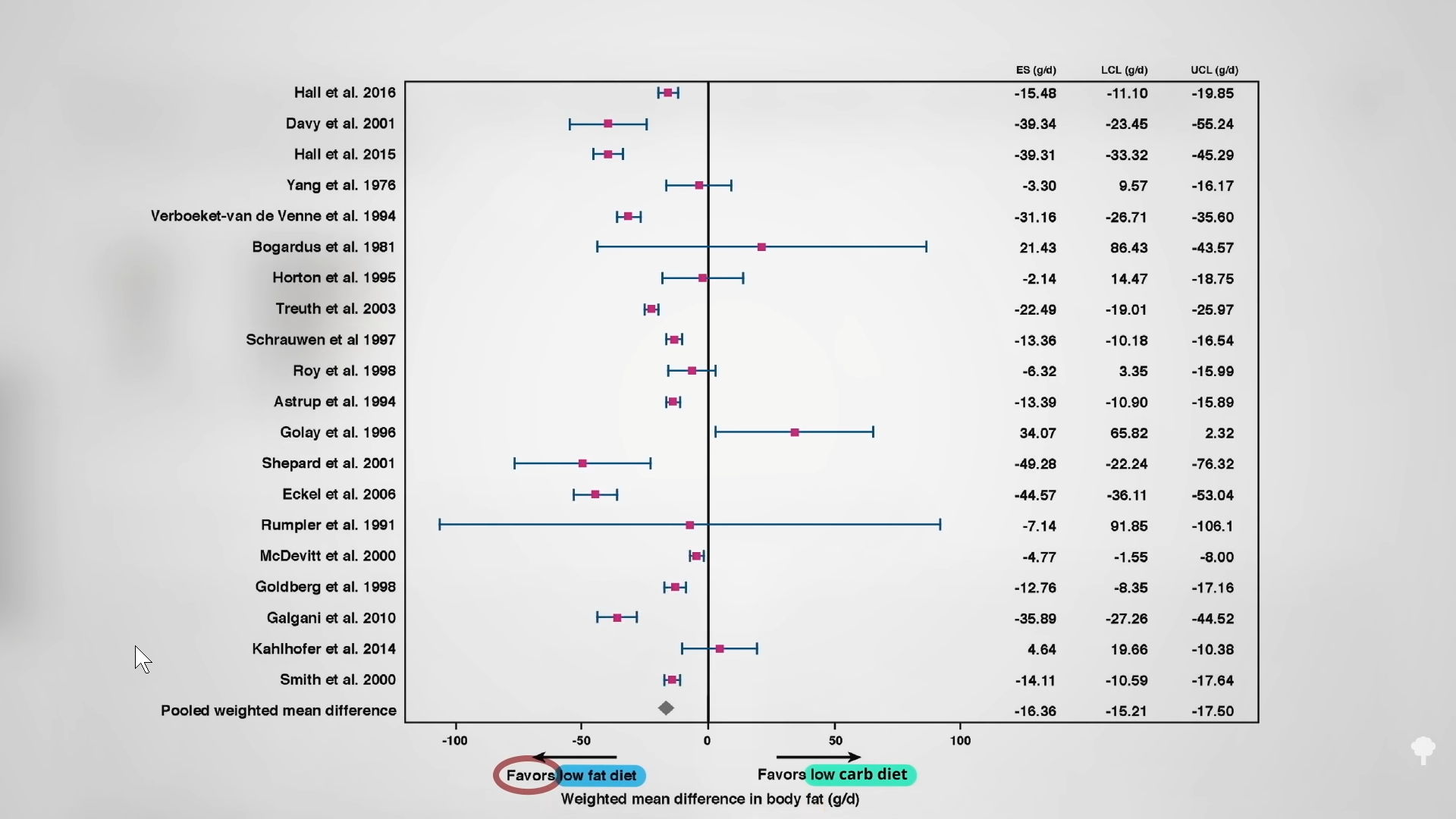
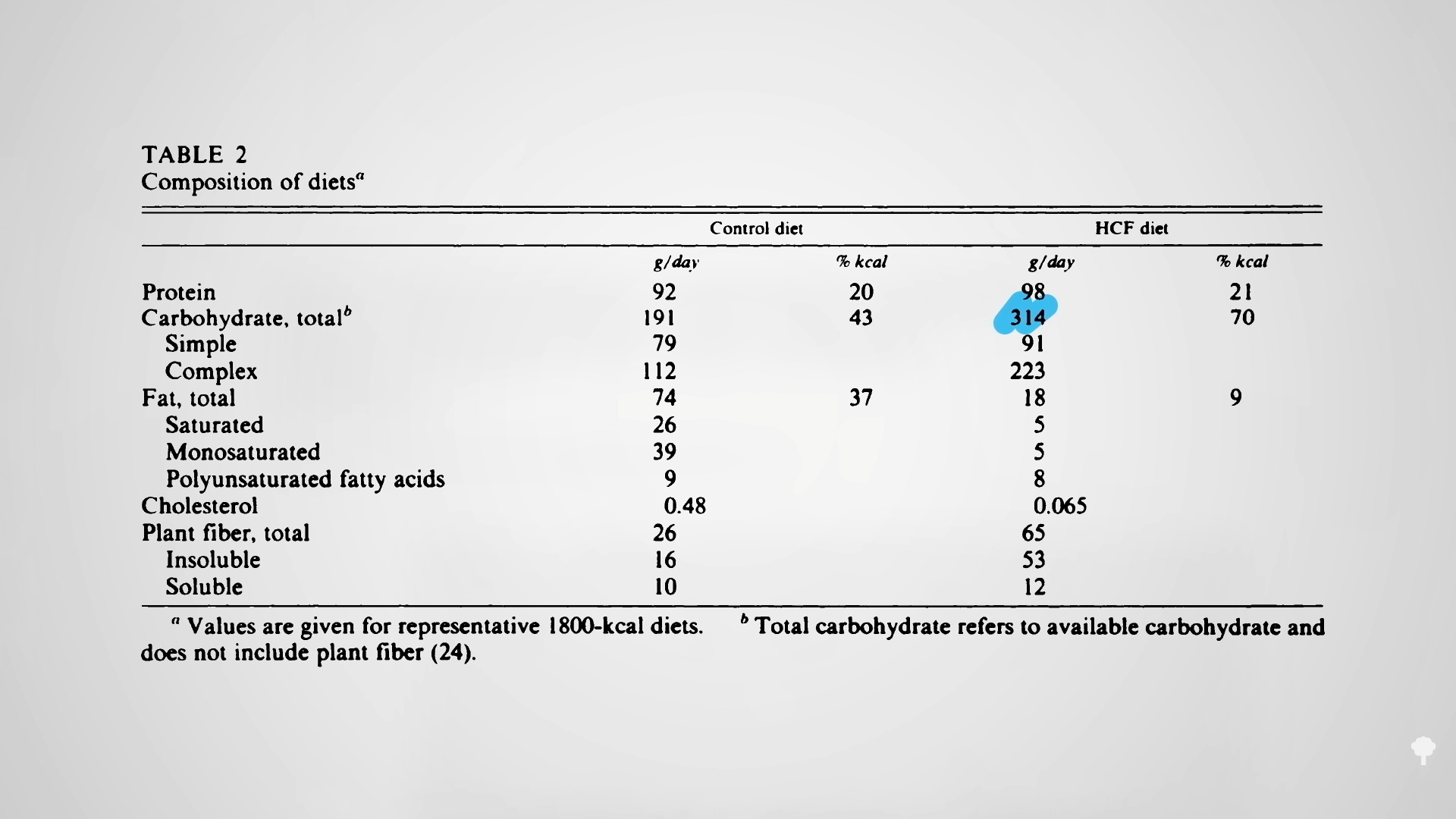
 Low-carb diets cut down on refined grains and added sugars, and low-fat diets tend to cut down on added fats and meat, so they both tell people to cut down on donuts. Any diet that does that already has a leg up. I figure a don’t-eat-anything-that-starts-with-the-letter-D diet could also successfully cause weight loss if it caused people to cut down on donuts, danishes, and Doritos, even if it makes no nutritional sense to exclude something like dill.
Low-carb diets cut down on refined grains and added sugars, and low-fat diets tend to cut down on added fats and meat, so they both tell people to cut down on donuts. Any diet that does that already has a leg up. I figure a don’t-eat-anything-that-starts-with-the-letter-D diet could also successfully cause weight loss if it caused people to cut down on donuts, danishes, and Doritos, even if it makes no nutritional sense to exclude something like dill.