What effects do fasting and a plant-based diet have on TBI and migraines?
An uncontrolled and unpublished study purported to show a beneficial effect of fasting on migraine headaches, but fasting may be more likely to trigger a migraine than help it. In fact, “skipped meals are among the most consistently identified dietary triggers” of headaches in general. In a review of hundreds of fasts at the TrueNorth Health Center in California, the incidence of headache was nearly one in three, but TrueNorth also published a remarkable case report on post-traumatic headache.
The U.S. Centers for Disease Control and Prevention (CDC) estimates that more than a million Americans sustain traumatic brain injuries (TBIs) every year. Chronic pain is a common complication, affecting perhaps three-quarters of those who suffer such an injury. There are drugs, of course, to treat post-traumatic headache. There are always drugs. And if drugs don’t work, there is surgery, cutting the nerves to the head to stop the pain.
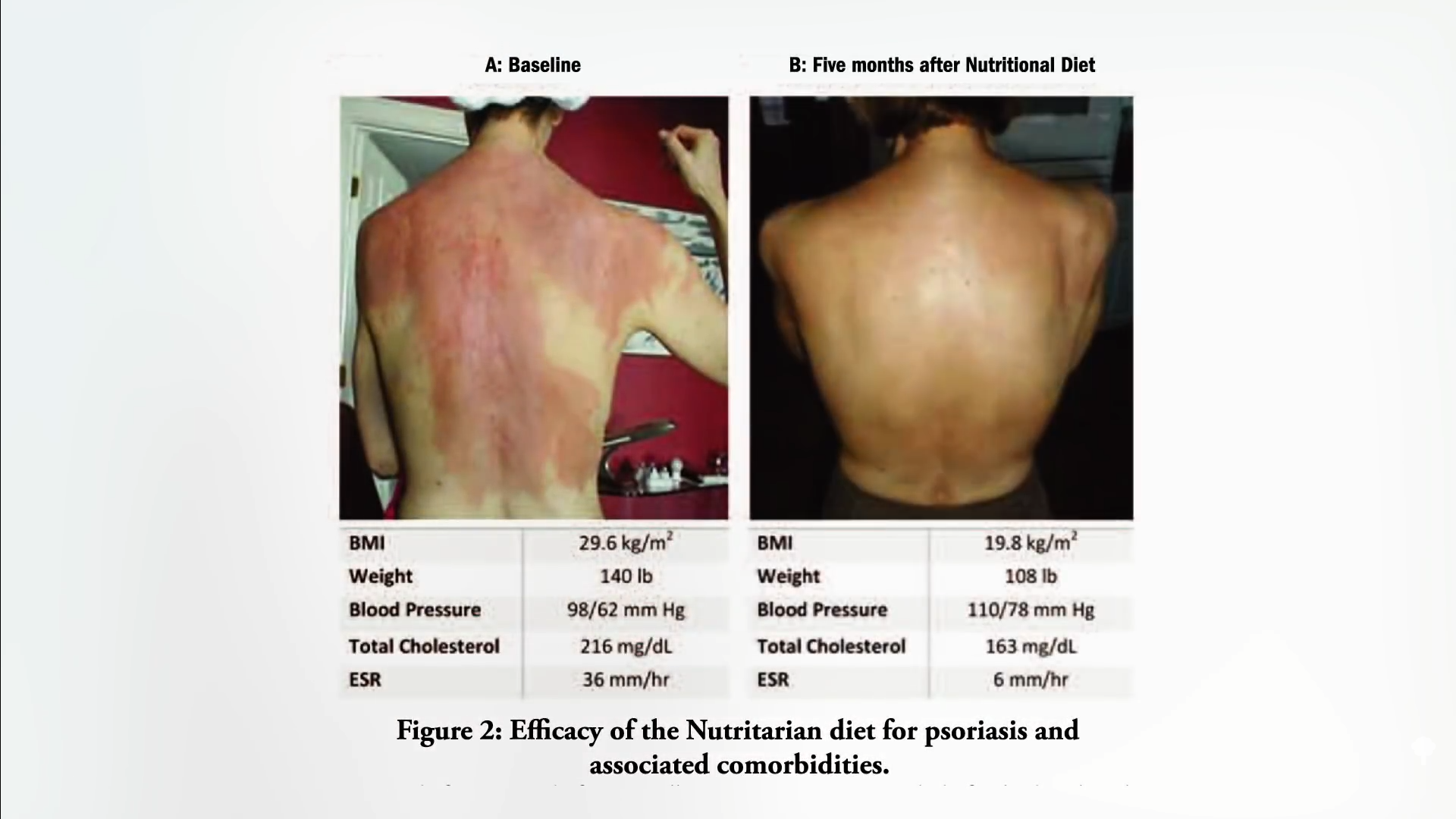
What about fasting and plants? A 52-year-old woman presented with a highly debilitating, difficult-to-manage, unremitting, chronic post-traumatic headache. And when I say chronic, I mean chronic; she experienced pain for 16 years. She then achieved long-term relief after fasting, followed by an exclusively plant-foods diet, free of added sugar, oil, or salt.
Before then, she had tried drug after drug after drug after drug after drug—with no relief, suffering in constant pain for years. Before the fast, she started out in constant pain. Then, after the fast, the intensity of the pain was cut in half, and though she was still having daily headaches, at least there were some pain-free periods. Six months later, she tried again, and eventually her headaches became mild, lasting less than ten minutes, and infrequent. She continued that way for months and even years, as you can see below and at 1:45 in my video Fasting for Post-Traumatic Brain Injury Headache.
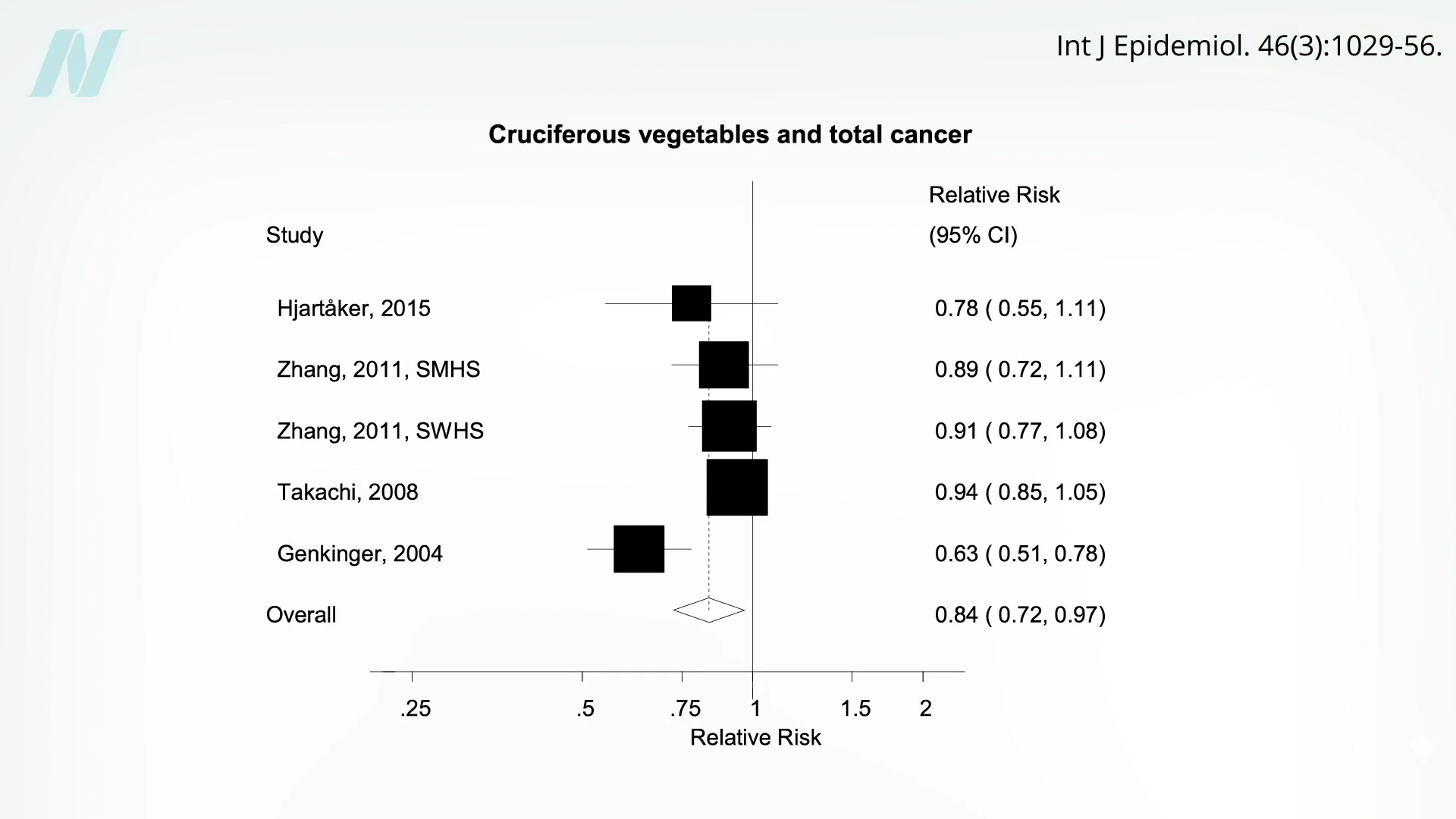
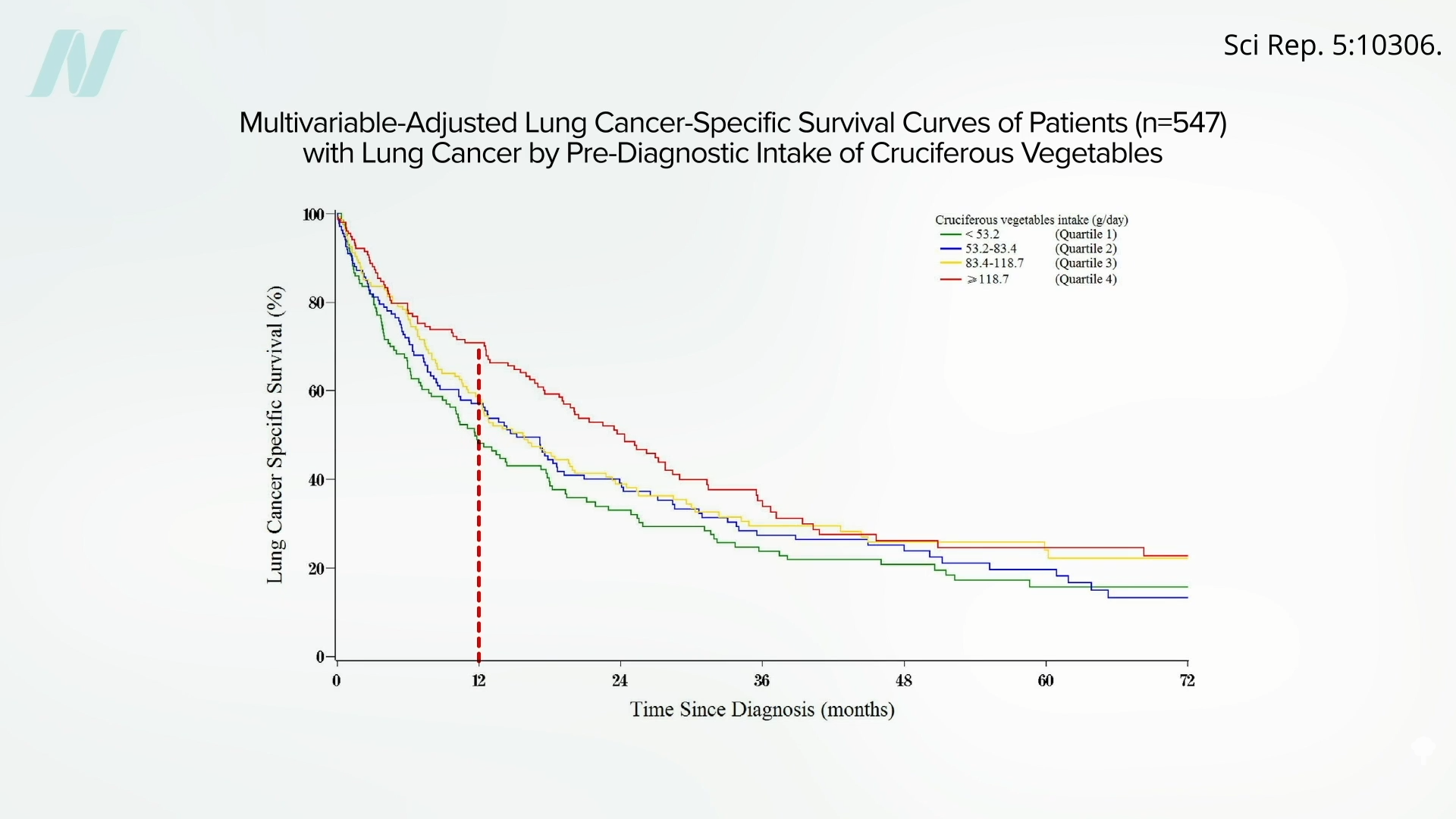
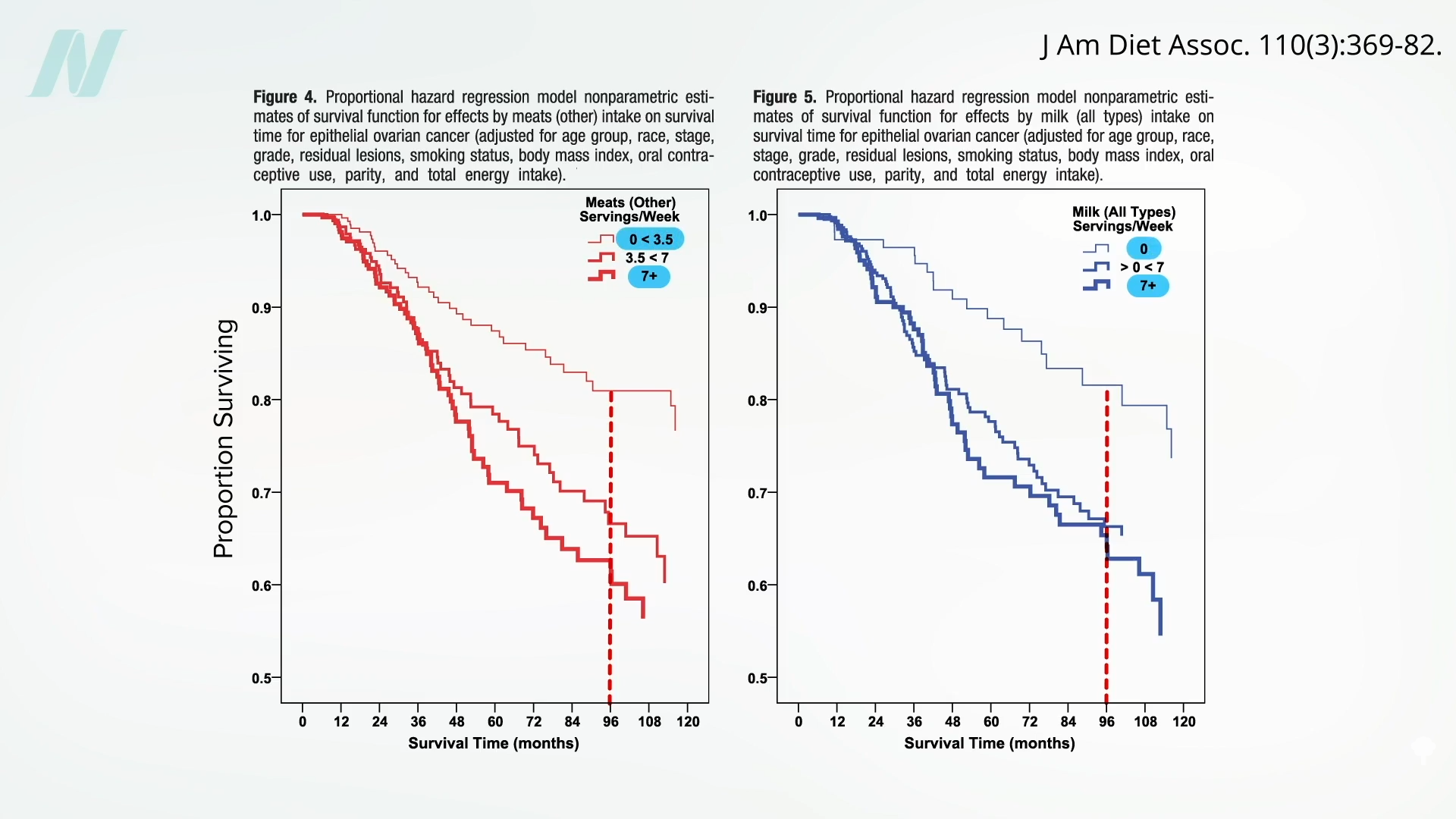
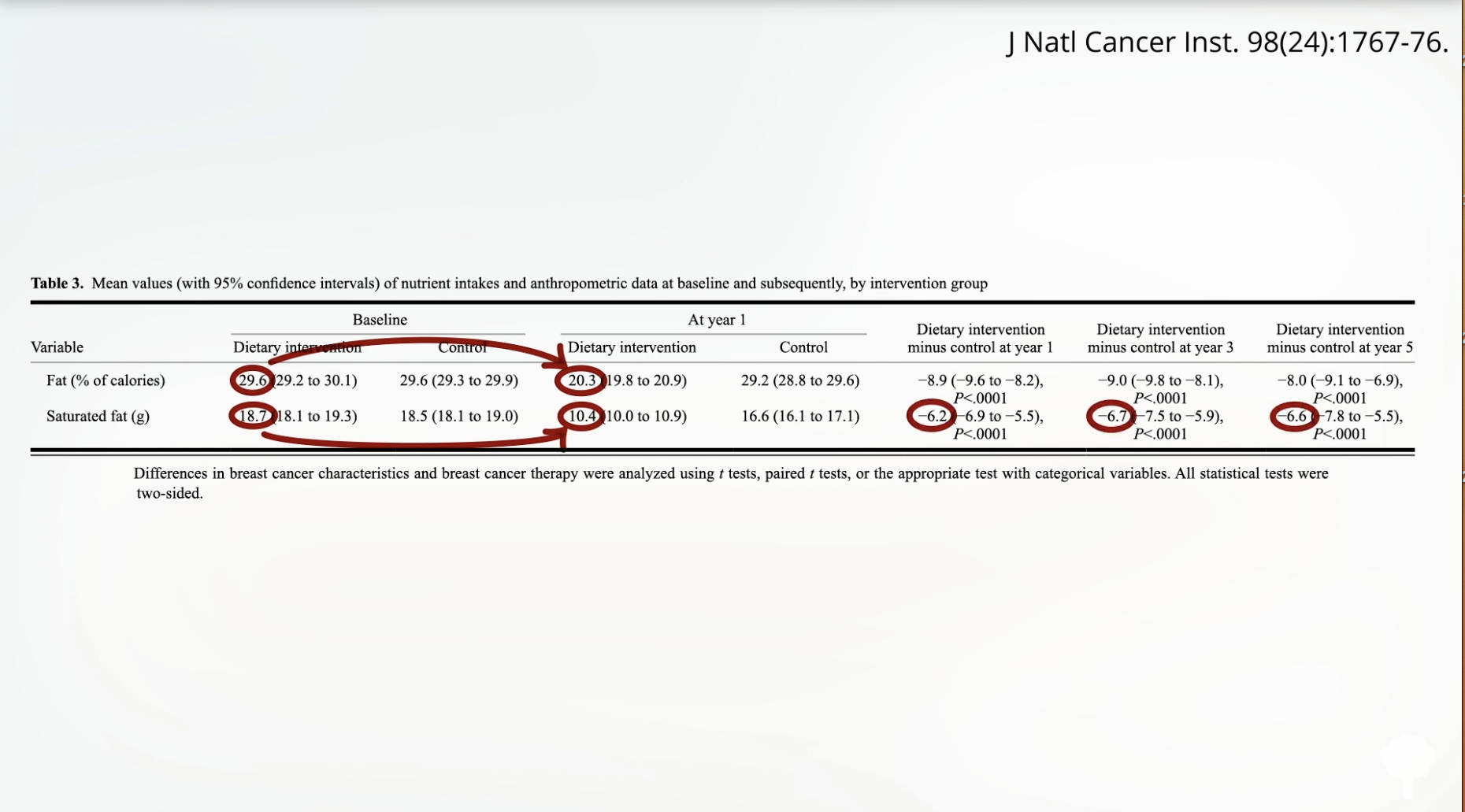
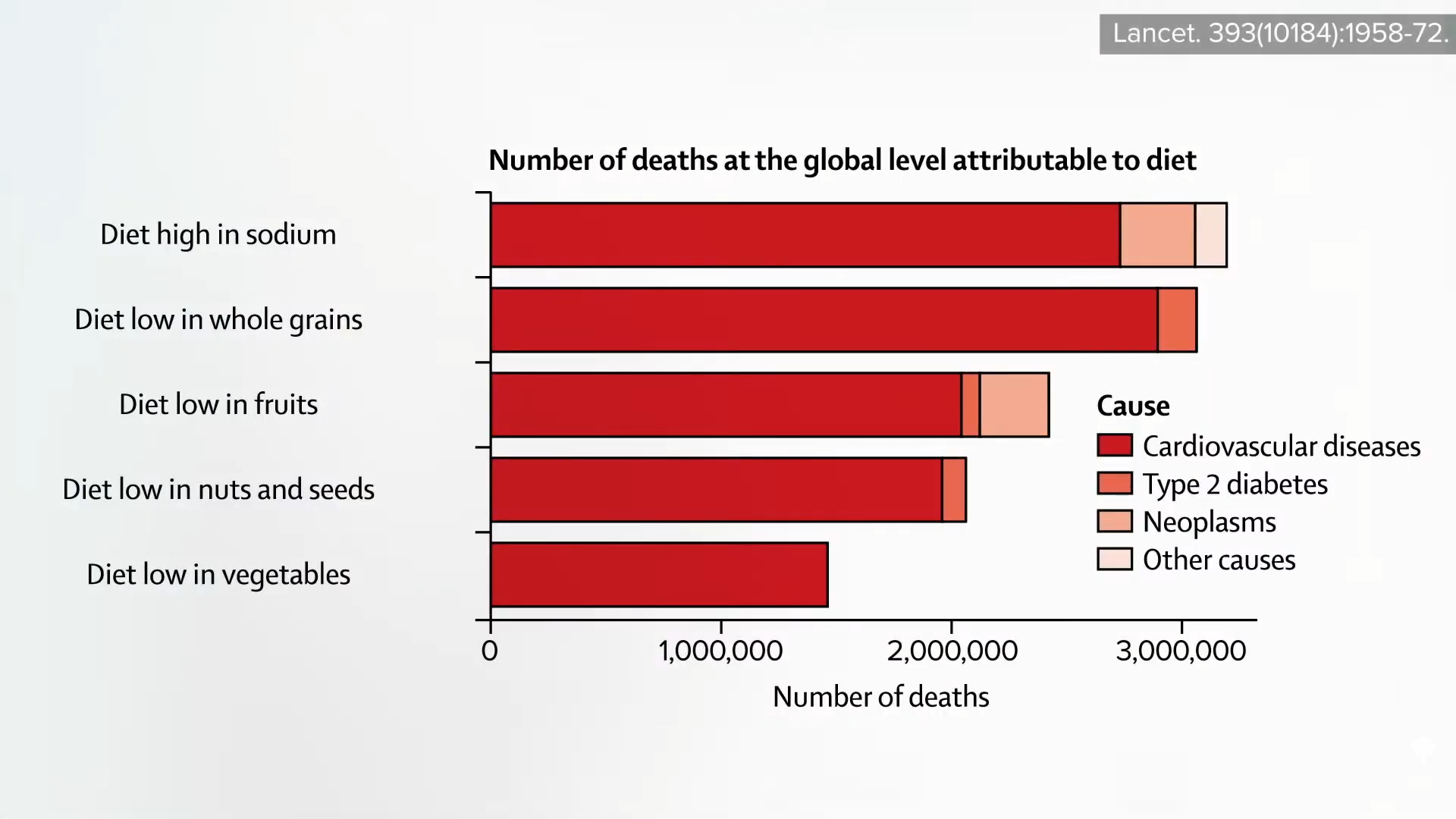
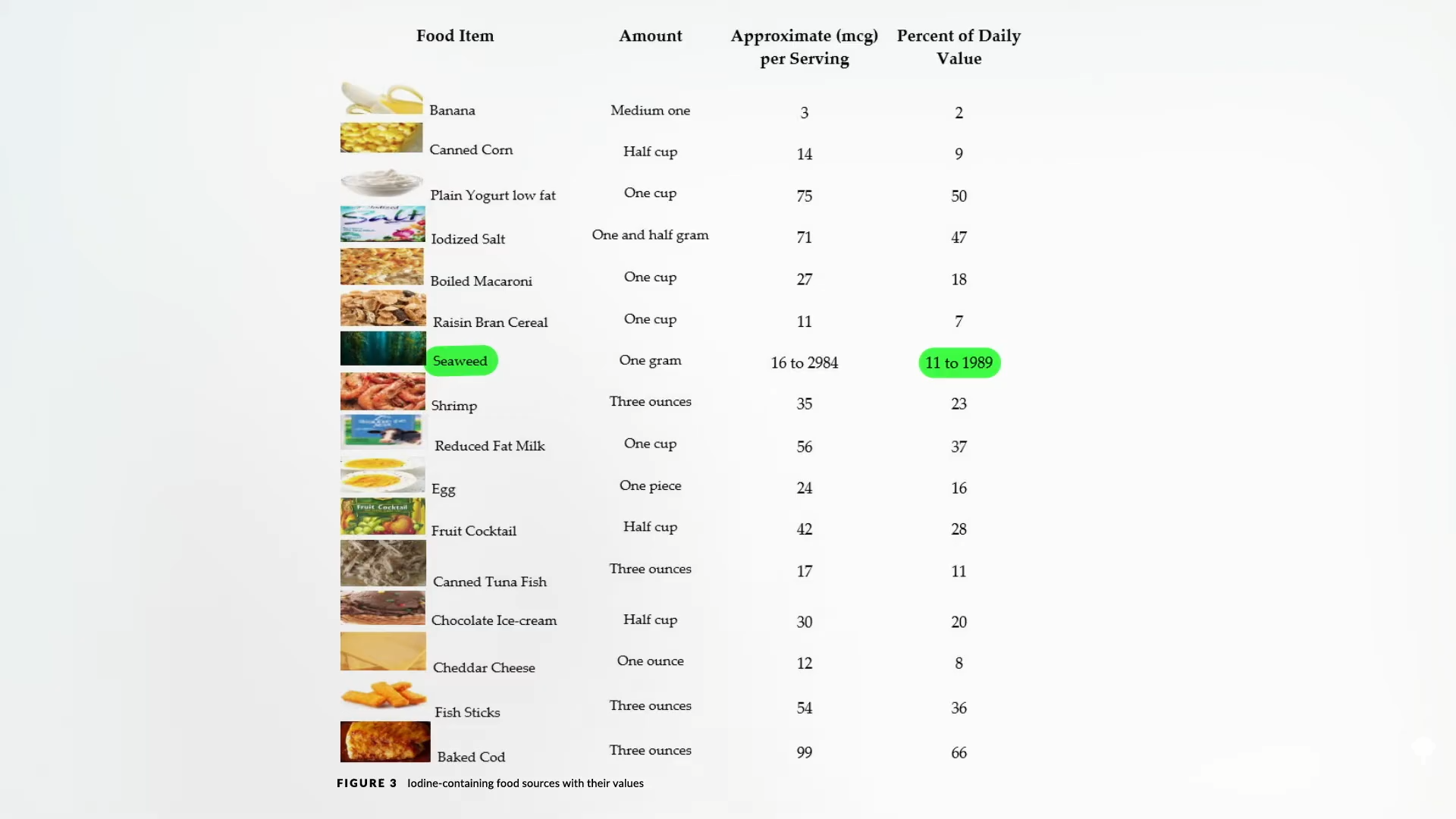
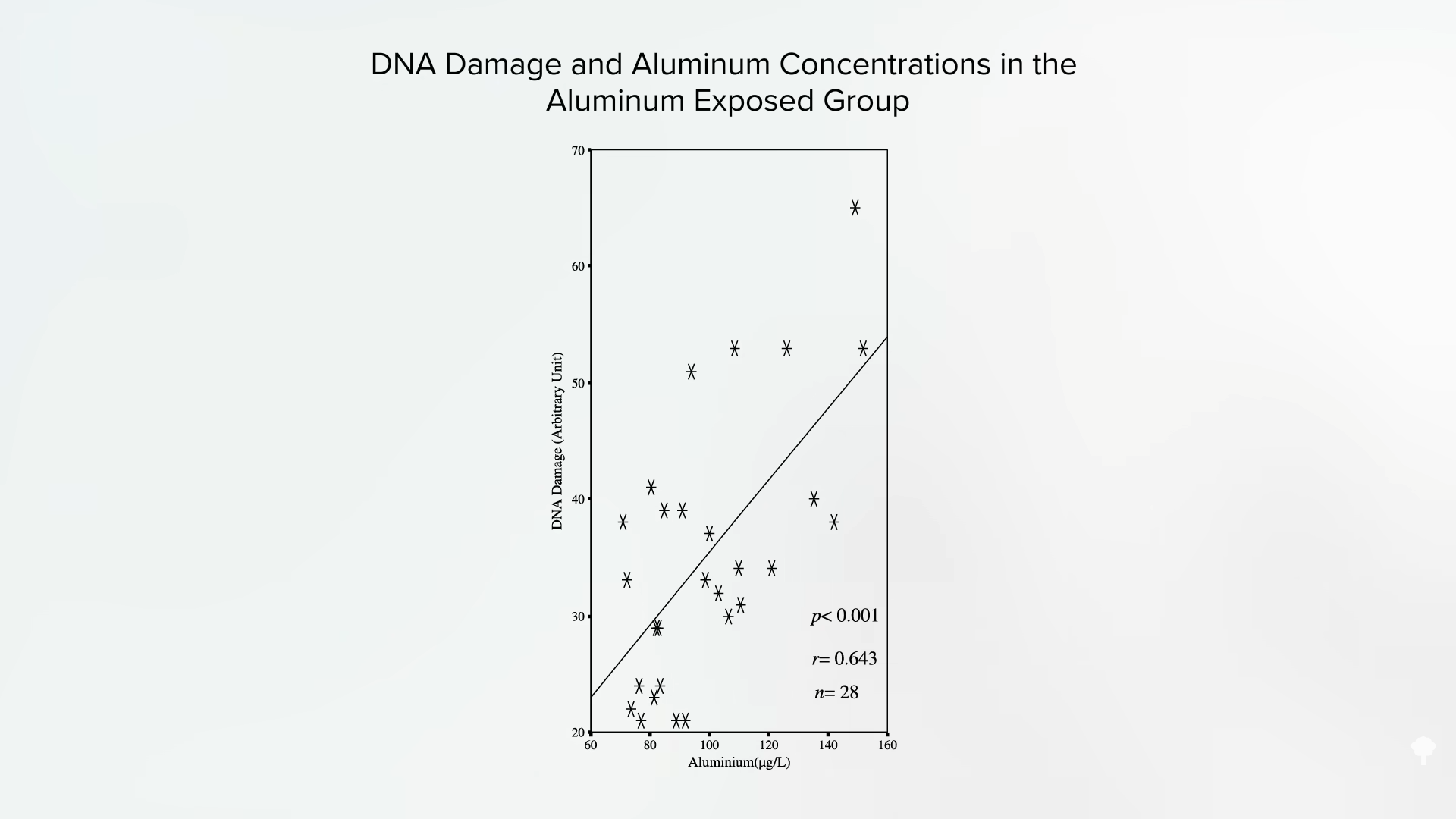
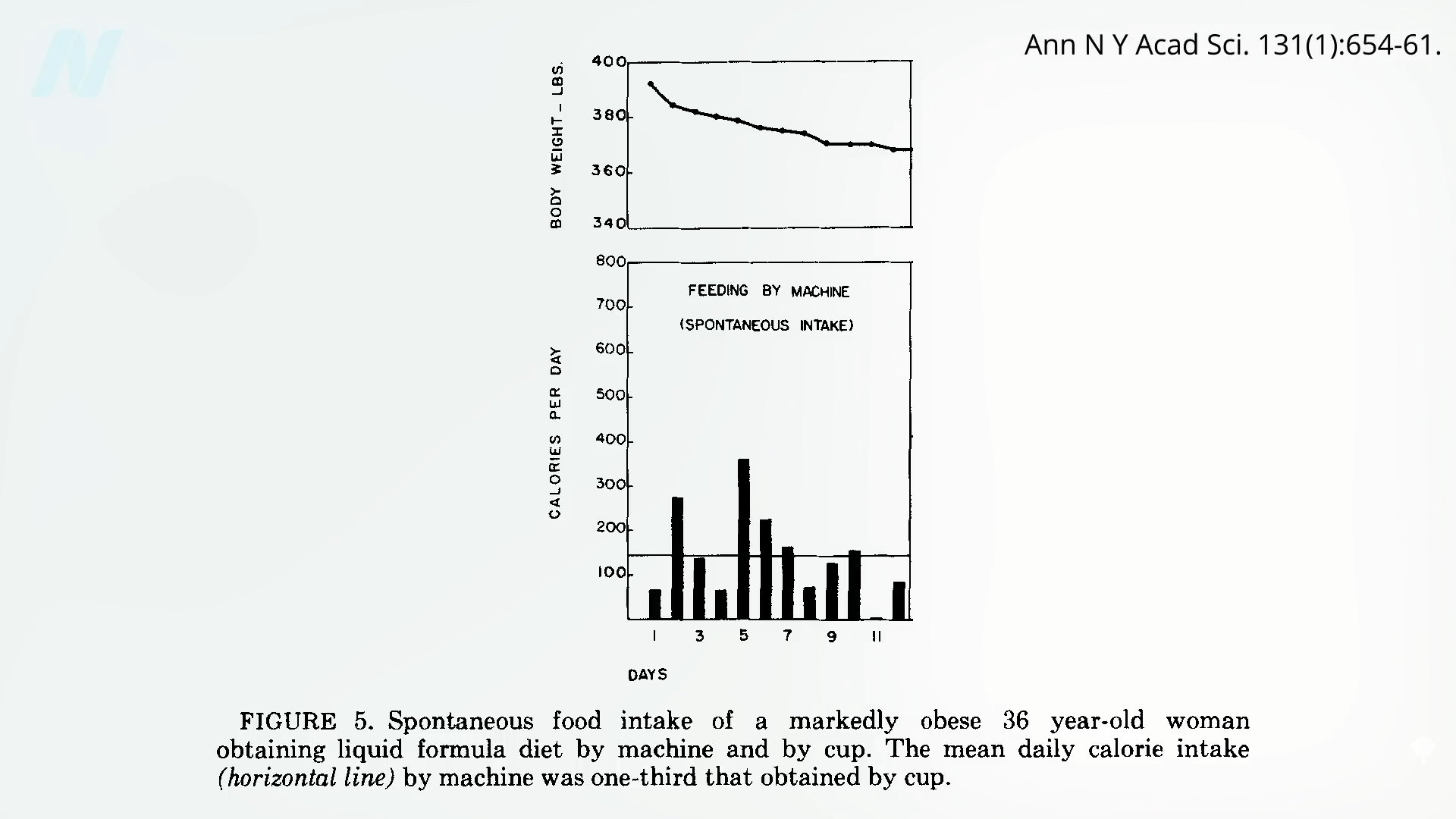
Now, of course, it’s hard to disentangle the effects of the fasting from the effects of the whole food, plant-based diet she remained on for those ensuing years. You’ve heard of analgesics (painkillers). Well, there are some foods that may be pro-algesic (pain-promoting), such as foods high in arachidonic acid, including meats, dairy, and eggs. So, the lowering of arachidonic acid—from which our body makes a range of pro-inflammatory compounds—may be accomplished by eating a more plant-based diet. So, maybe that contributed to the benefit in the fasting case, since many plant foods are high in anti-inflammatory components. In terms of migraine headaches, more plant foods and less animal foods may help, but you don’t know until you put it to the test.
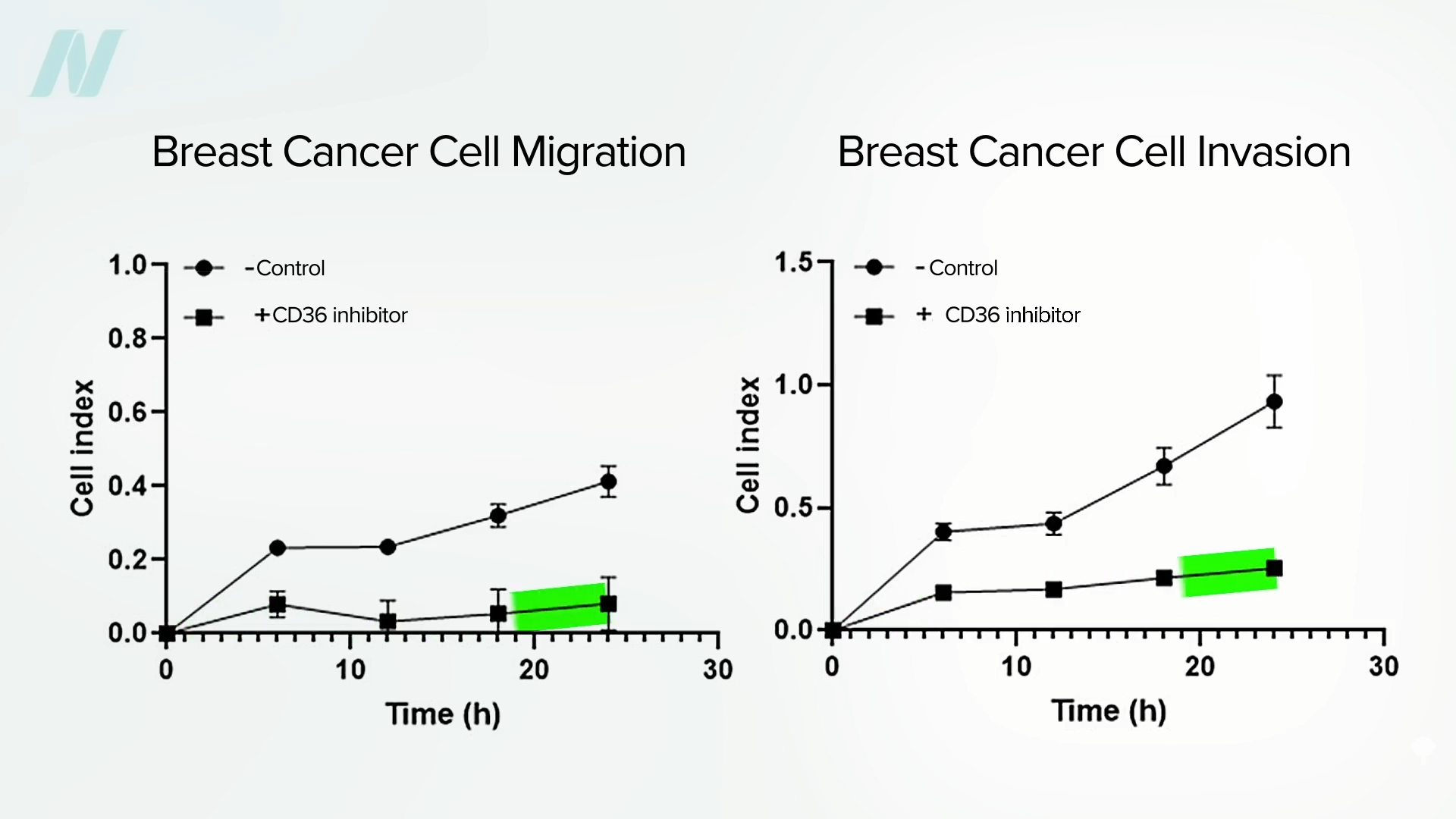
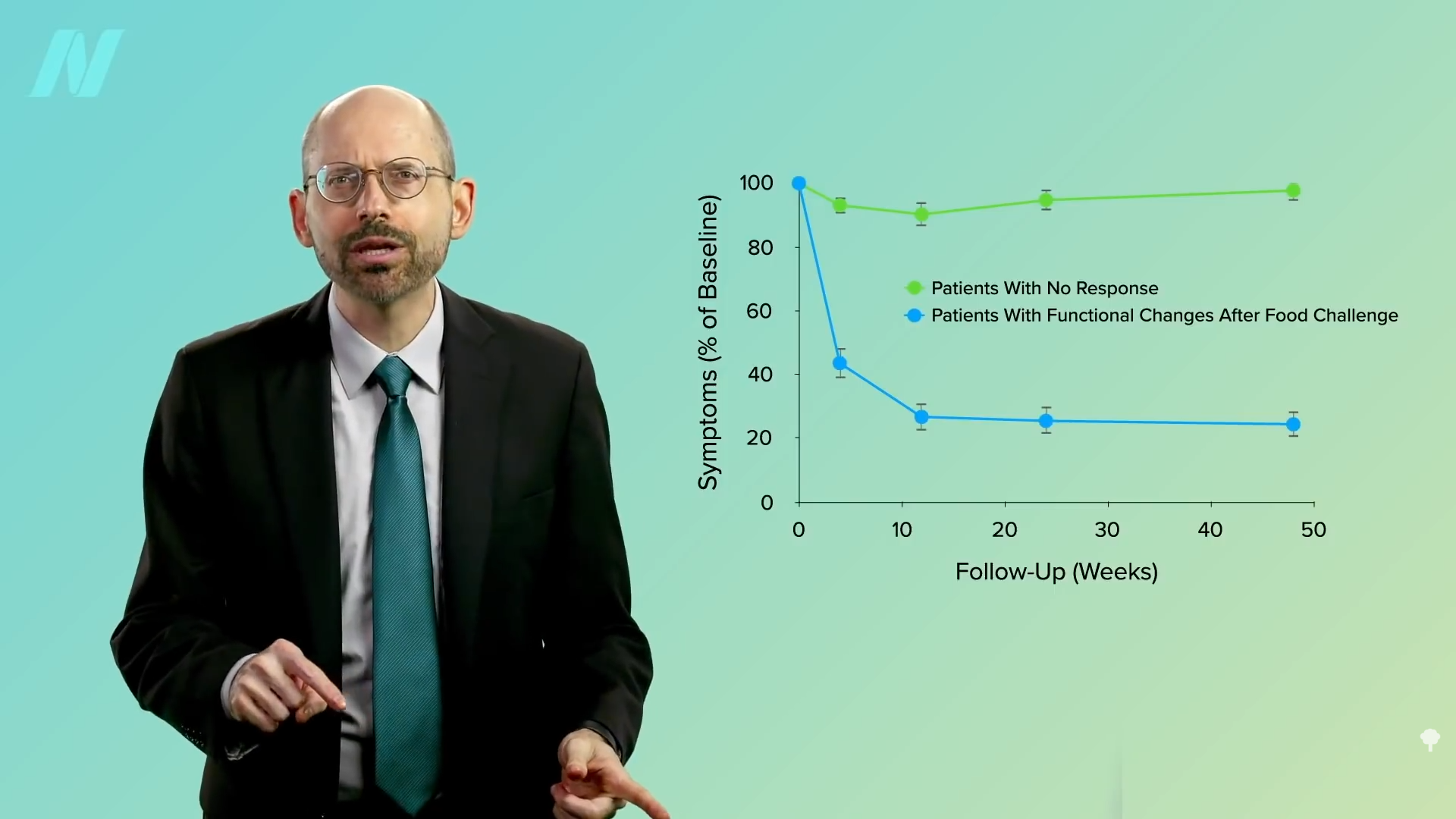
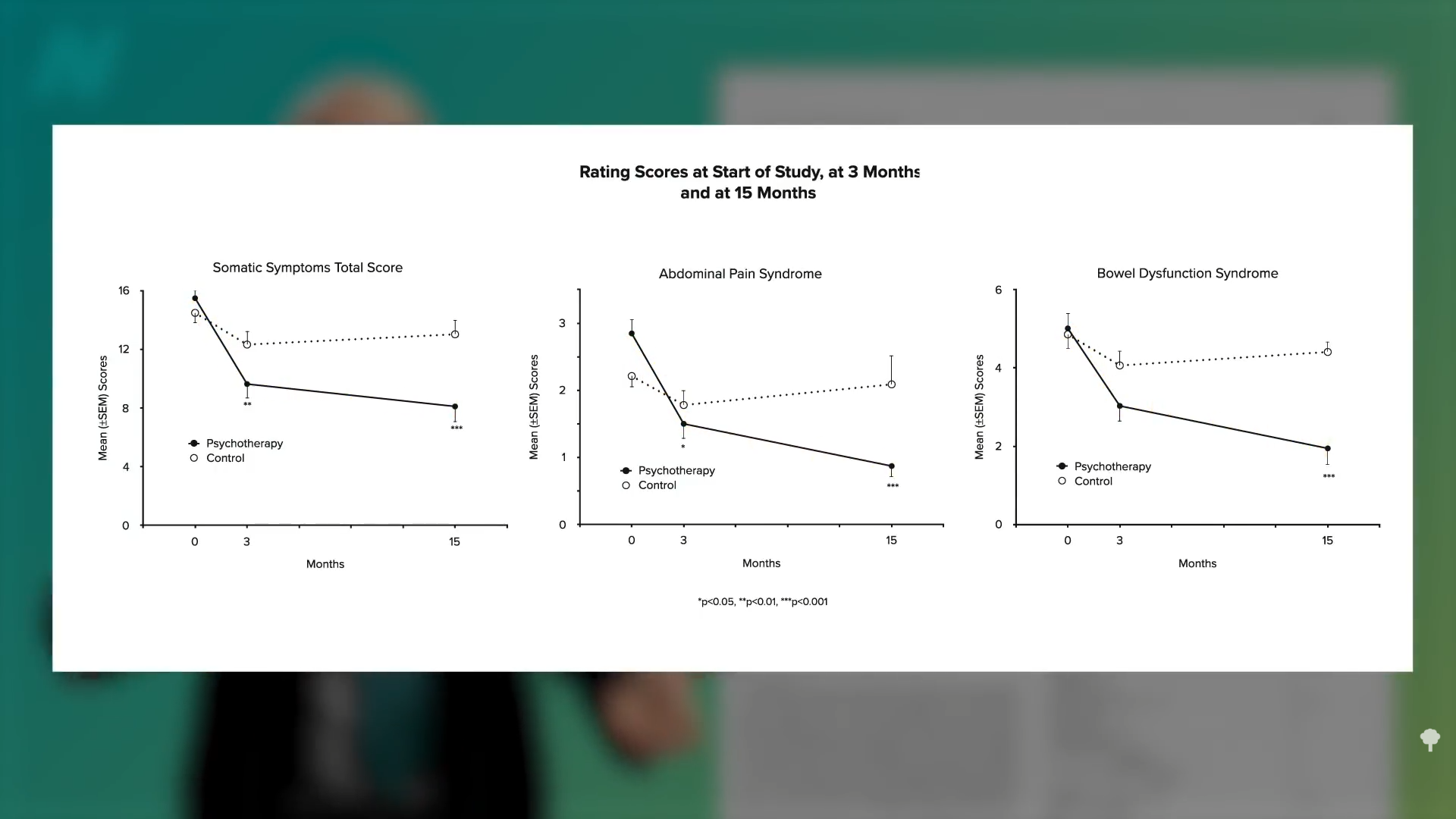
Researchers figured a plant-based diet may offer the best of both worlds, so they designed a randomized, controlled, crossover study where those with recurrent migraines were randomized to eat a strictly plant-based diet or take a placebo pill. Then, the groups switched. During the placebo phase, half of the participants said their pain improved, and the other half said their pain remained the same or got worse. But, during the dietary phase, they almost all got better, as you can see here and at 3:11 in my video.
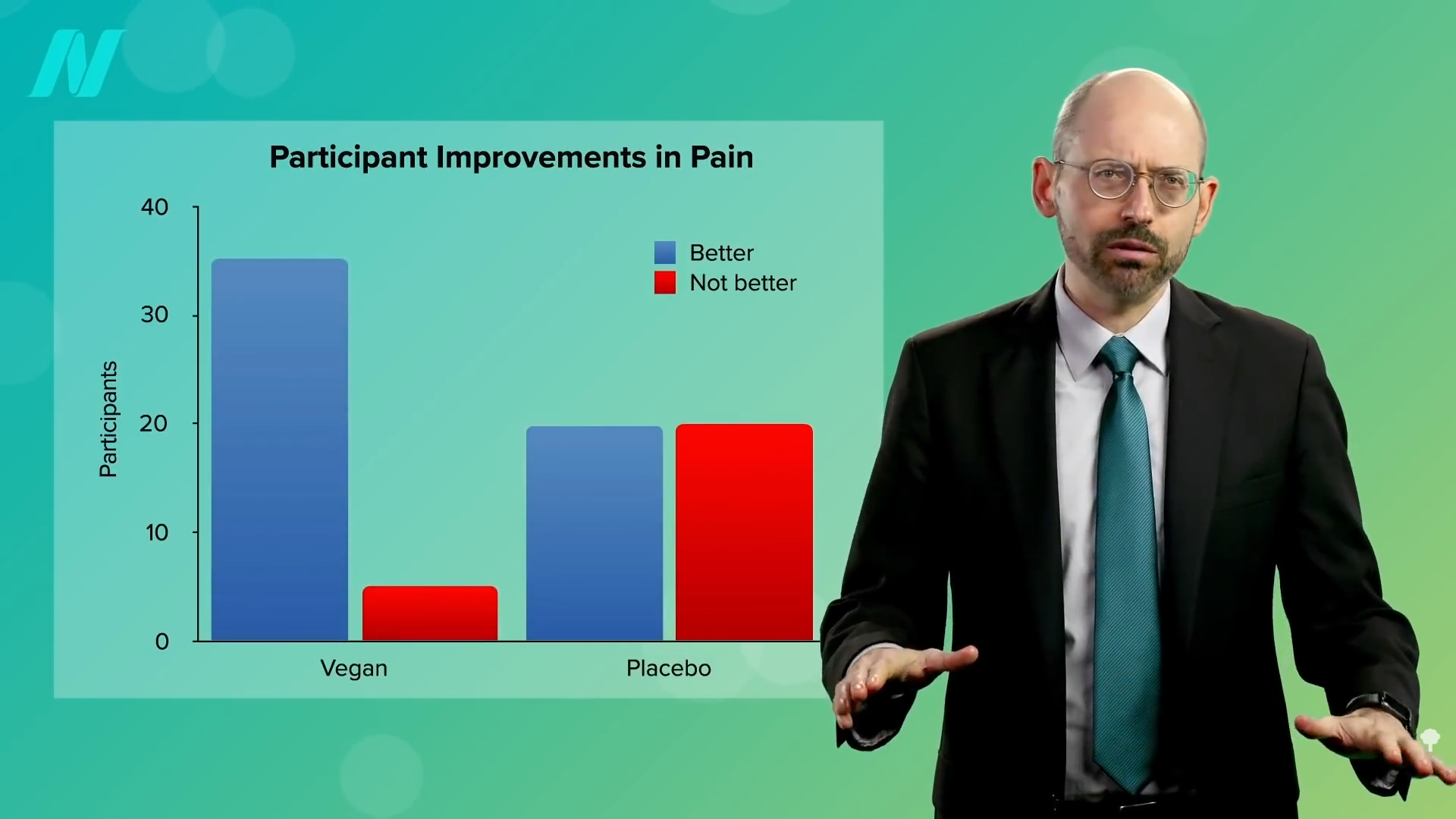
During that first phase, the diet group experienced significant improvements in the number of headaches, pain intensity, and days with headaches, as well as a reduction in the amount of painkillers they needed to take. In fact, it worked a little too well. Many individuals were unwilling to return to their previous diets after they completed the diet phase of the trial, thereby refusing to complete the study. Remember, the participants were supposed to go back to their regular diets and take a placebo pill, but they felt so much better on the plant-based diet that they refused. We’ve seen this with other trials, where those trying plant-based diets felt so good, they often refused to abandon them, harming the study. So, plant-based diets can sometimes work a little too well.
All my videos on fasting are available in a digital download here.
Michael Greger M.D. FACLM
Source link
 We appear to
We appear to