Post-traumatic stress disorder diagnoses among college students more than doubled between 2017 and 2022, climbing most sharply as the coronavirus pandemic shut down campuses and upended young adults’ lives, according to new research published on Thursday.
The prevalence of PTSD rose to 7.5 percent from 3.4 percent during that period, according to the findings. Researchers analyzed responses from more than 390,000 participants in the Healthy Minds Study, an annual web-based survey.
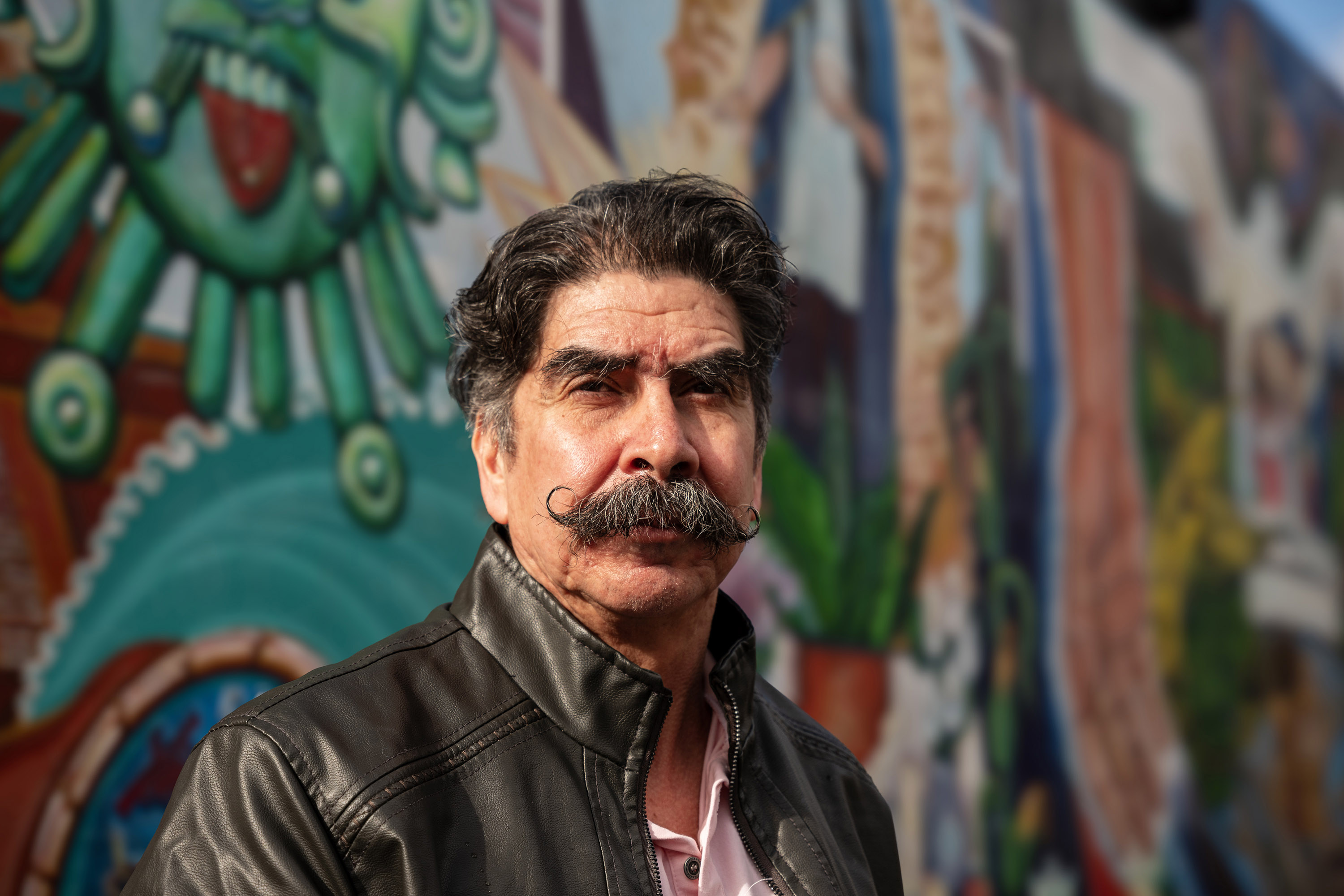
“The magnitude of this rise is indeed shocking,” said Yusen Zhai, the paper’s lead author, who heads the community counseling clinic at the University of Alabama at Birmingham. His clinic had seen more young people struggling in the aftermath of traumatic events. So he expected an increase, but not such a large one.
Dr. Zhai, an assistant professor in the Department of Human Studies, attributed the rise to “broader societal stressors” on college students, such as campus shootings, social unrest and the sudden loss of loved ones from the coronavirus.
PTSD is a mental health disorder characterized by intrusive thoughts, flashbacks and heightened sensitivity to reminders of an event, continuing more than a month after it occurs.
It is a relatively common disorder, with an estimated 5 percent of adults in the United States experiencing it in any given year, according to the most recent epidemiological survey conducted by the Department of Health and Human Services. Lifetime prevalence is 8 percent in women and 4 percent in men, the survey found.
The new research also found a sharp rise in the prevalence of a similar condition, acute stress disorder, which is diagnosed less than a month after a trauma. Diagnoses rose to 0.7 percent among college students in 2022, up from 0.2 percent five years earlier.
Use of mental health care increased nationally during the pandemic, as teletherapy made it far easier to see clinicians. Treatment for anxiety disorders increased most steeply, followed by PTSD, bipolar disorder and depression, according to economists who analyzed more than 1.5 million insurance claims for clinician visits between 2020 and 2022.
PTSD was introduced as an official diagnosis in 1980, as it became clear that combat experiences had imprinted on many Vietnam veterans, making it difficult for them to work or participate in family life. Over the decades that followed, the definition was revised to encompass a larger range of injury, violence and abuse, as well as indirect exposure to traumatic events.
However, the diagnosis still requires exposure to a Criterion A trauma, defined in the Diagnostic and Statistical Manual of Mental Disorders as “death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence.”
It is not uncommon for young adults to experience traumatic events. A 1996 study of Detroit residents found that exposure to traumatic events — such as violent assaults, injuries or unexpected death — peaked sharply between the ages of 16 and 20. It then declined precipitously after age 20.
Research suggests that less than one-third of people exposed to traumatic events go on to develop PTSD.
Shannon E. Cusack, an academic researcher who has studied PTSD in college students, said there was division within the field about whether the profound disruptions that young adults experienced during the pandemic — abrupt loss of housing and income, social isolation and fear about infections — amount to triggering events.
“They’re causing symptoms that are consistent with the PTSD diagnosis,” said Dr. Cusack, a clinical psychologist and an assistant professor of psychiatry at Virginia Commonwealth University. “Am I not going to treat them because their stressor doesn’t count as a trauma?”
The prevalence data, she said, points to a pressing need for PTSD treatment on college campuses. Short-term treatments developed for veterans, such as prolonged exposure therapy and cognitive processing therapy, have proved effective in managing PTSD symptoms.
Stephen P. Hinshaw, a professor of psychology at the University of California, Berkeley, said that the disruptions of the pandemic might have left college students emotionally depleted and less resilient when faced with traumatic events.
“Midway through this study, there may have been legitimately more trauma and death,” he said, adding that the lockdowns may have caused more general despair among young people. “With the general mental health deterioration, is it harder to cope with traumatic stressors if you do get exposed to them?”
Some changes to the diagnostic manual may have blurred the line between PTSD and disorders like depression or anxiety, Dr. Hinshaw said. In 2013, the committee overseeing revisions to the manual expanded the list of potential PTSD symptoms to include dysphoria, or a deep sense of unease, and a negative worldview, which could also be caused by depression, he said. But the changes, he added, do not account for the sharp increase in diagnoses.
Ellen Barry
Source link