Emergency responses—being, well, emergency responses—aren’t designed to last forever, and this morning, the World Health Organization declared the one that’s been in place for the COVID-19 pandemic since January 2020 officially done. “This virus is here to stay. It is still killing, and it’s still changing,” Tedros Adhanom Ghebreyesus, the director general of the WHO, said at a press conference; although the coronavirus will continue to pose a threat, the time had simply come, he and his colleagues said, for countries to move away from treating it as a global crisis.
And, really, they already have: The United States, for instance, ended its national emergency last month and will sunset its public-health emergency next week; countries around the world have long since shelved testing programs, lifted lockdowns, dispensed with masking mandates, and even stopped recommending frequent COVID shots to healthy people in certain age groups. In some ways, the WHO was already a straggler. Had it waited much longer, the power of its designation of COVID as a “public health emergency of international concern,” or PHEIC, “would have been undermined,” says Salim Abdool Karim, the director of the Centre for the AIDS Program of Research in South Africa.
There’s no disputing that the virus’s threat has ebbed since the pandemic’s worst days. By and large, “we are in our recovery phase now”—not perfectly stabilized, but no longer in chaotic flux, says René Najera, the director of public health at the College of Physicians of Philadelphia. Still, ending the emergency doesn’t mean that the world has fully addressed the problems that made this an emergency. Global vaccine distribution remains wildly inequitable, leaving many people susceptible to the virus’s worst effects; deaths are still concentrated among those most vulnerable; the virus’s evolutionary and transmission patterns are far from predictable or seasonal. Now, ending the emergency is less an epidemiological decision than a political one: Our tolerance for these dangers has grown to the extent that most people are doing their best to look away from the remaining risk, and will continue to until the virus forces us to turn back.
The end to the PHEIC, to be clear, isn’t a declaration that COVID is over—or even that the pandemic is. Both a PHEIC and a pandemic tend to involve the rapid and international spread of a dangerous disease, and the two typically do go hand in hand. But no set-in-stone rules delineate when either starts or ends. Plenty of diseases have met pandemic criteria—noted by many epidemiologists as an epidemic that’s rapidly spread to several continents—without ever being granted a PHEIC, as is the case with HIV. And several PHEICs, including two of the Ebola outbreaks of the past decade and the Zika epidemic that began in 2015, did not consistently earn the pan- prefix among experts. With COVID, the WHO called a PHEIC more than a month before it publicly labeled the outbreak a pandemic on March 11. Now the organization has bookended its declaration with a similar mismatch: one crisis designation on and the other off. That once again leaves the world in a bizarre risk limbo, with the threat everywhere but our concern for it on the wane.
For other diseases with pandemic potential, understanding the start and end of crisis has been simpler. After a new strain of H1N1 influenza sparked a global outbreak in 2009, disrupting the disease’s normal seasonal ebb and flow, scientists simply waited until the virus’s annual transmission patterns went back to their pre-outbreak baseline, then declared that particular pandemic done. But “we don’t really have a baseline” to return to for SARS-CoV-2, says Sam Scarpino, an infectious-disease modeler at Northeastern University. This has left officials floundering for an end-of-pandemic threshold to meet. Once, envisioning that coda seemed more possible: In February 2021, when the COVID shots were still new, Alexis Madrigal wrote in The Atlantic that, in the U.S. at least, pandemic restrictions might end once the country reached some relatively high rate of vaccination, or drove daily deaths below 100—approximating the low-ish end of the flu’s annual toll.
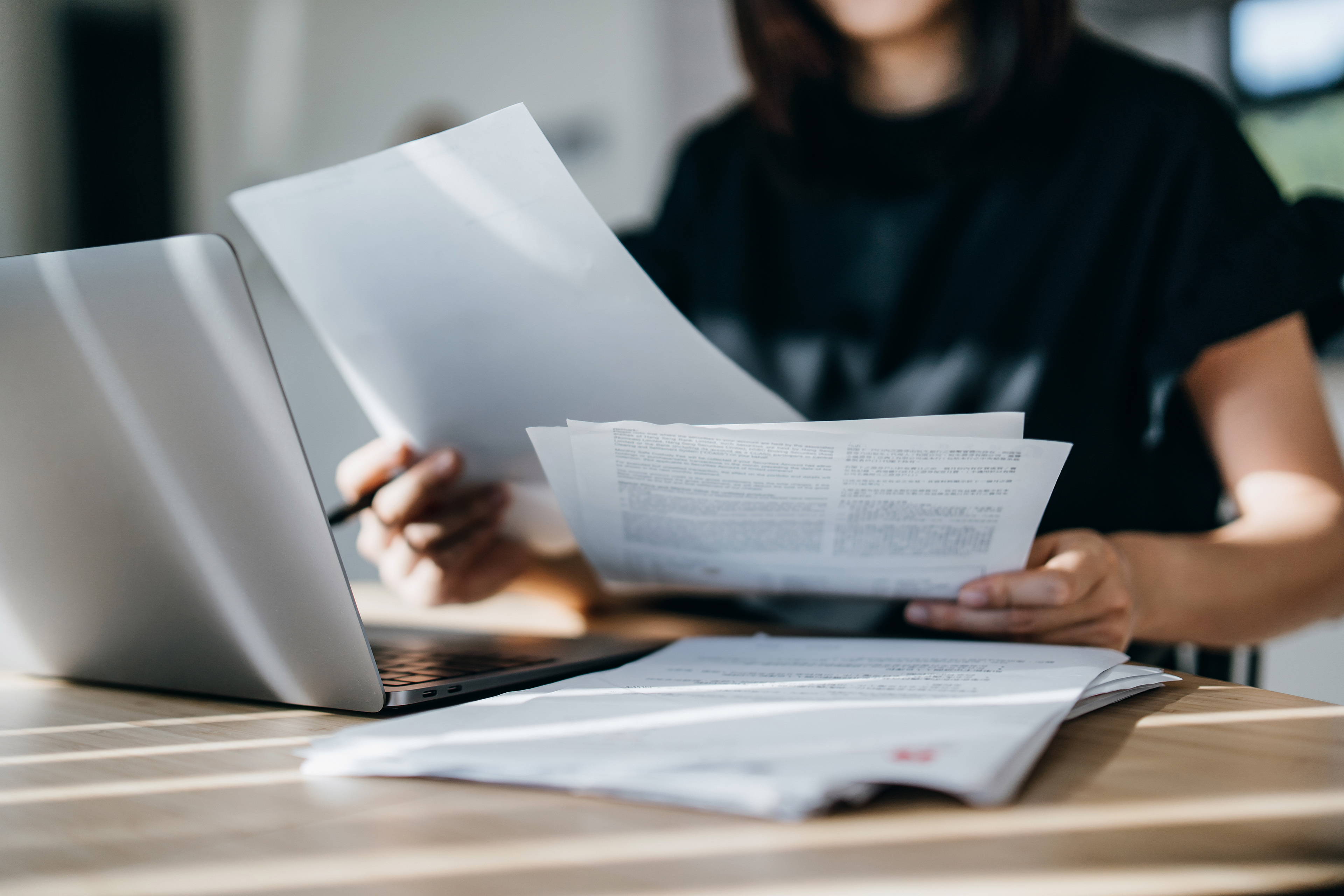
Those criteria aren’t perfect. Given how the virus has evolved, even, say, an 85 percent vaccination rate probably wouldn’t have squelched the virus in a way public-health experts were envisioning in 2021 (and wouldn’t have absolved us of booster maintenance). And even if the death toll slipped below 100 deaths a day, the virus’s chronic effects would still pose an immense threat. But thresholds such as those, flawed though they were, were never even set. “I’m not sure we ever set any goals at all” to designate when we’d have the virus beat, Céline Gounder, an infectious-disease physician at NYU and an editor-at-large for public health at KFF Health News, told me. And if they had been, we probably still would not have met them: Two years out, we certainly have not.
Instead, efforts to mitigate the virus have only gotten laxer. Most individuals are no longer masking, testing, or staying up to date on their shots; on community scales, the public goods that once seemed essential—ventilation, sick leave, equitable access to insurance and health care—have already faded from most discourse. That COVID has been more muted in recent months feels “more like luck” than a product of concerted muffling from us, Scarpino told me. Should another SARS-CoV-2 variant sweep the world or develop resistance to Paxlovid, “we don’t have much in the way of a plan,” he said.
If and when the virus troubles us again, our lack of preparedness will be a reflection of America’s classically reactive approach to public health. Even amid a years-long emergency declaration that spanned national and international scales, we squandered the opportunity “to make the system more resilient to the next crisis,” Gounder said. There is little foresight for what might come next. And individuals are still largely being asked to fend for themselves—which means that as this emergency declaration ends, we are setting ourselves up for another to inevitably come, and hit us just as hard.
As the final roadblocks to declaring normalcy disappear, we’re unlikely to patch those gaps. The PHEIC, at this point, was more symbolic than practical—but that didn’t make it inconsequential. Experts worry that its end will sap what remaining incentive there was for some countries to sustain a COVID-focused response—one that would, say, keep vaccines, treatments, and tests in the hands of those who need them most. “Public interest is very binary—it’s either an emergency or it’s not,” says Saskia Popescu, an infection-prevention expert at George Mason University. With the PHEIC now gone, the world has officially toggled itself to “not.” But there’s no going back to 2019. Between that and the height of the pandemic is middle-ground maintenance, a level of concern and response that the world has still not managed to properly calibrate.
Katherine J. Wu
Source link