In an ideal version of this coming winter, the United States would fully revamp its approach to respiratory disease. Pre-pandemic, fall was just a time for flu shots, if that. Now, hundreds of millions of Americans have at their fingertips vaccines that can combat three cold-weather threats at once: flu, COVID, and, for a subset of us, respiratory syncytial virus. If everyone signed up to get the shots they qualified for, “it would be huge,” says Ofer Levy, the director of the Precision Vaccines Program at Boston Children’s Hospital. Hospital emergency rooms and intensive-care units wouldn’t fill; most cases of airway illness would truly, actually feel like “just” a common cold. “We would save tens of thousands of lives in the United States alone,” Levy told me.
The logic of the plan is simple: Few public-health priorities are more pressing than getting three lifesaving vaccines to those who need them most, ahead of winter’s viral spikes. The logistics, however, are not as clear-cut. The best way to get vaccines into as many people as possible is to make getting shots “very, very easy,” says Chelsea Shover, an epidemiologist at UCLA. But that’s just not what we’ve set up this fall lineup of shots to do.
Convenience isn’t the only issue keeping shots out of arms. But move past fear, distrust, or misinformation, solve for barriers such as insurance coverage, and getting a vaccine in the United States still means figuring out when shots are available and which you qualify for, finding and booking appointments, carving out the time to go. For adults, especially, who don’t routinely visit their doctor for wellness checkups, and whose workplaces don’t require vaccines to the extent that schools do, vaccination has become an onerous exercise in opt-ins.
Bundling this year’s flu, COVID, and RSV vaccines into a single visit could, in theory, help ease the way to becoming a double or triple shotter. “Any time we can cut down on the number of visits for a patient to take care of them, we know that’s a big boost,” says Tochi Iroku-Malize, the president of the American Academy of Family Physicians. But the easiest iteration of that strategy, a three-in-one shot, similar to the MMR and DTaP vaccines of childhood, doesn’t yet exist (though some are in trials). Even the shorter-term solution—giving up to three injections at once—is hitting stumbling blocks. Pharmacies started receiving flu vaccines earlier this summer and are already giving them out to anyone over the age of six months. RSV vaccines, too, have hit shelves, and have been approved for people over the age of 60 and those 32 to 36 weeks pregnant; so far, however, they are being offered only to the first group. And although nearly all Americans are expected to be eligible for autumn’s updated COVID vaccines, those shots aren’t slated to make an appearance until mid-September or so, according to Kevin Griffis, a CDC spokesperson.
Timing two or three shots together isn’t a perfect plan. Get them all too early, and some people’s protections against infection might fade before the season gets into full swing; get all of them too late, and a virus might beat the vaccine to the punch. Respiratory viruses don’t coordinate their seasons: Right now, for instance, COVID cases are on a sharp rise, but flu and RSV ones are not. Some data on the new RSV vaccines also suggests that co-administering them with other shots might trigger slightly worse side effects, or mildly curb the number of antibodies that the injections raise. Still, Levy argues that those theoretical downsides are outweighed by known benefits. “If someone is at clinic in the fall, they should get all the vaccines they’re eligible for,” he told me. Getting a slightly less effective, slightly more ornery shot a few months early is better than never getting a shot at all.
All of that supposes that people understand that they are eligible for these shots. But already, family-medicine physicians such as Iroku-Malize, who practices in Long Island, have been fielding queries about the RSV vaccines from confused patients. Some new parents, for instance, have gotten the impression that the RSV vaccines are designed to be administered to infants, which isn’t quite right: Babies are the target of protection for the shots for pregnant people, but only because they temporarily inherit antibodies—not because they can get the injections themselves. Regulators also haven’t yet nailed down how often older adults might need the shot, though the current thinking is that the vaccine’s protection will last at least a couple of years. “It’s very hard to tell people, ‘I don’t know,’” says Jacinda Abdul-Mutakabbir, an infectious-disease pharmacist at UC San Diego.
Other parts of the RSV-shot messaging are peppered with even more unknowns. The CDC has yet to release its final recommendation for pregnant people; for people over 60, the agency’s language has been “noncommittal,” says Rupali Limaye, a behavioral scientist at Johns Hopkins University. Unlike past guidelines that have straightforwardly recommended flu shots or most doses of the COVID-19 vaccine, RSV guidance says that eligible people may protect themselves against the virus—and are urged to first consult a health-care provider, which not all people have. The wishy-washiness is partly about safety: A few rare but serious medical events cropped up during the RSV vaccines’ clinical trials, including abnormal heartbeats and neurological complications. None of the experts I spoke with had qualms about recommending the shots anyway. Even so, some private health-insurance companies have seized on the CDC’s watered-down recommendation—and the fact that the agency hasn’t yet included RSV in its annual vaccine schedule for adults—as an excuse to not cover the shot, leaving some patients paying $300-plus out of pocket.
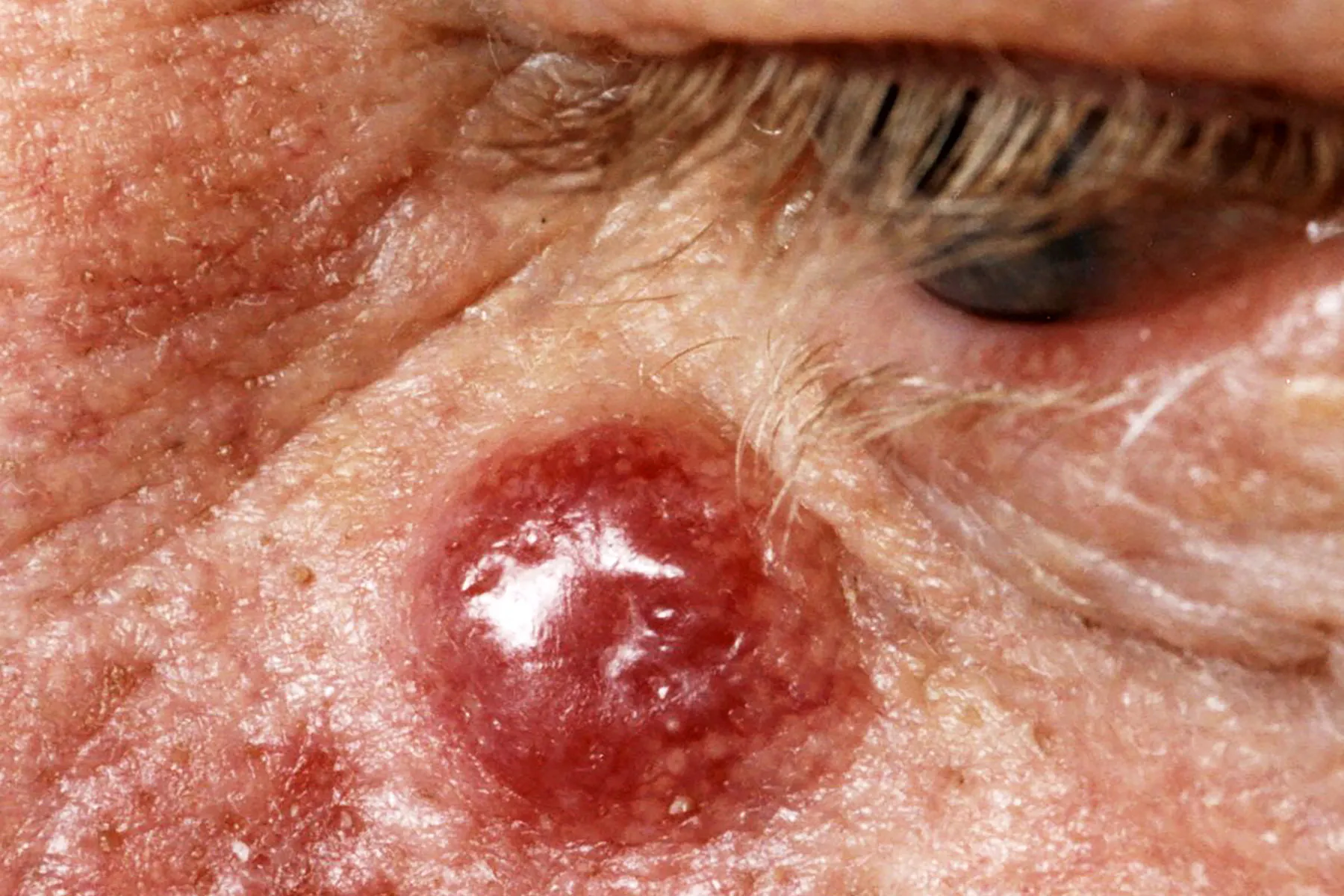
For any of these shots, viral reputation matters too. Despite hospitalizing tens of thousands of Americans each year, especially at age extremes—numbers that, in some years, nearly rival those linked to flu—RSV is a lesser-known winter disease. People tend to take it less seriously, if it’s on their radar at all, Abdul-Mutakabbir told me. Which bodes poorly for future RSV-shot uptake. Annual flu shots have been recommended for 13 years for every American over the age of six months for 13 years. And still, just half the eligible population gets them in any given year. People tend to dismiss shots as subpar interventions against a disease that they don’t much fear, Limaye told me. With COVID, too, “people think it’s gotten mild,” she said. Only 28 percent of American adults are currently up to date on their COVID vaccine. And although older people have historically been more vigilant about nabbing shots, even vaccines against shingles—a notoriously painful disease—have reached just over a third of people who are 60-plus.
To establish fall as an immunity-seeking season, shots would need to become an annual habit, ideally one easy to form. Mandates and financial incentives do prod people toward vaccines, but smaller nudges can persuade people to take initiative on their own. Some strategies may be as simple as semantic tweaks. Studies on HPV and flu vaccines suggest that telling patients they are “due” for a shot is better than offering it as an optional choice, says Gretchen Chapman, a behavioral scientist at Carnegie Mellon University. Other research suggests that carefully worded text-message reminders can evoke ownership—noting that a shot is “waiting for you,” or that the time has come to “claim your dose.” Noel Brewer, a behavioral scientist at the University of North Carolina at Chapel Hill, also thinks that vaccine deliverers could take inspiration from dentists who gently dog their patients with phone calls and postcards.
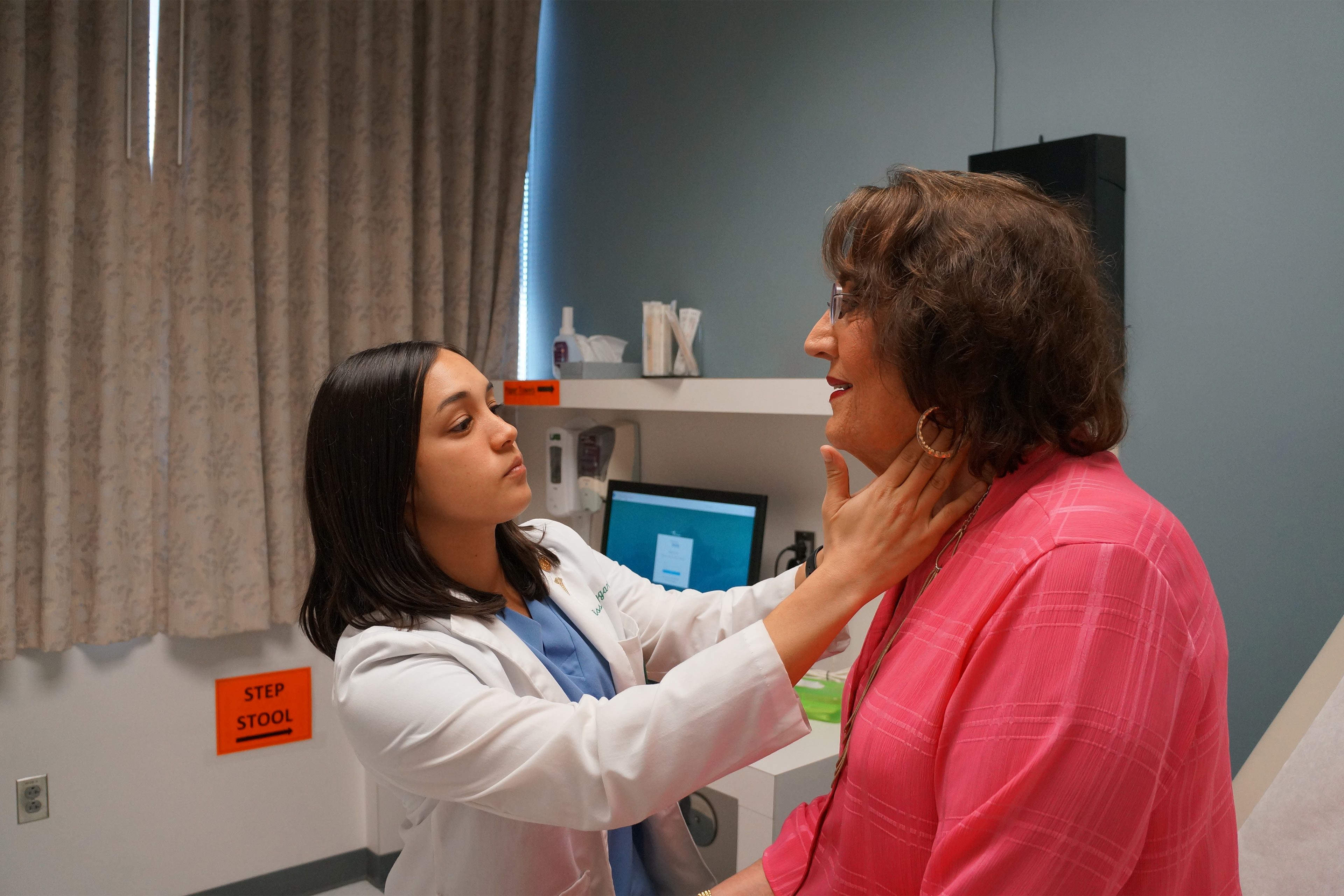
Other interventions could be aimed at streamlining delivery. Government funding could make shots more available in rural regions, ensure access for those who lack insurance, and help local health departments offer shots in churches and hair salons, or even bring them door to door. More schools and workplaces, too, might try boosting uptake among students and employees. And although most shots are already given within the health-care system, there’s sludge to clear from that pipeline too. Better universal recordkeeping could help track people’s vaccination status through their lifetime. Kimberly Martin, a behavioral scientist at Yale, is researching ways to revamp medical training to help health-care providers earn their patients’ trust—especially among populations that remain marginalized by systemic racism. “The single biggest impact on vaccine uptake,” Brewer told me, “is a health-care provider recommendation.”
An ideal vision of a fall in the future, then, would be turning vaccines into a default form of prevention—a more typical part of this country’s wellness workflow, says Saad Omer, the dean of the Peter O’Donnell Jr. School of Public Health, at UT Southwestern. After getting their vital signs checked, patients could have their vaccination status reviewed. “And then, if they’re eligible, you vaccinate them,” Omer told me. It’s a routine that pediatricians already have down pat. If adult health care follows suit, regular immunization is a habit we may never have to outgrow.
Katherine J. Wu
Source link