Areas of bipartisan agreement are few and far between in Washington, but improving our system of medicine by cracking down on the influence of special interests should be an area of common ground. Making strides against this destructive force will go a long way toward repairing public trust and preparing for the next health emergency. President Biden had it right when he took aim at the “record profits” of the pharmaceutical industry at his State of the Union. Congress needs to rebalance the role of a central regulatory state with the power of a doctor’s judgment in providing patients the best possible care.
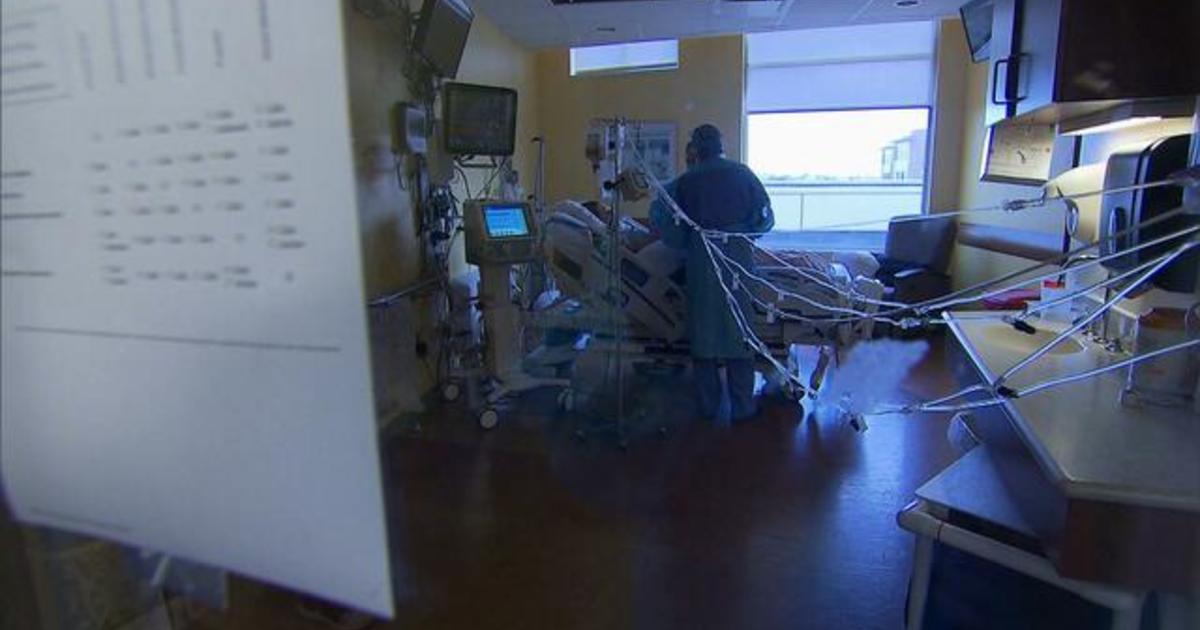
The COVID-19 pandemic highlighted the weaknesses of our health infrastructure, particularly the deficiencies in researching and deploying readily available drugs. Our public health agencies put all their weight behind randomized controlled trials (RCTs). These complex, time-consuming studies were in many cases run by scientists paid by the pharmaceutical industry — and unsurprisingly concluded that pricey, new, patented drugs were best. Hospitals and health care facilities moved in lockstep with the government in demanding a forceful, uniform response. Doctors felt tremendous pressure to follow the science — not the science they observed treating patients, but the science that was enforced — and patients had few treatment options.
We’re only beginning to understand how deeply this has disrupted medical practice. Doctors thinking critically and trusting their own experience has formed the foundation of medicine for a thousand years. They apply the scientific method, testing different approaches to heal patients, building on what works and discarding what doesn’t.
In the early 20th century, this process was used when Alexander Fleming discovered a compound, penicillin, that prevented fungus growing in his lab. Years later, a team at Oxford tested his observation in a tiny study of just eight rats. Four treated with penicillin survived Streptococcus infection, while the other four died. That insight changed the world as the medicine was scaled up for mass treatment against bacterial infection in the ensuing decades, through World War II. Insulin was discovered around the same time when physicians noticed pancreatic secretions that affected the body’s ability to process glucose. It was observed, extracted, and then used in patients.
This process has produced hundreds of new drugs in the last century. It’s also produced new uses for drugs. In clinical practice, doctors routinely observe how drugs intended for one use can perform another function like reducing cholesterol, moderating blood pressure, or regulating depression. The Agency for Healthcare Research and Quality estimates that doctors prescribe 20% of drugs “off-label” for a different use than what FDA approved.
On our present course, where doctors are trained to be less curious and blindly follow standards of care rather than developing and testing treatment hypotheses, we’re going to see fewer medical breakthroughs. RCTs produce some useful data, but they must be complemented with the real-world evidence doctors accrue every day in practice that helps to translate our approved treatments into improved health and life expectancy. Congress can take two immediate actions to advance this goal.
First, it can ensure adequate funding for the National Center for Advancing Translational Sciences, the agency within the National Institutes of Health that enhances the development of diagnostics and therapeutics. This agency can accelerate knowledge around existing molecules and combined treatments. It should add a new function to robustly collect and analyze observational work of physicians to shape a scientific framework that can more effectively advance beyond single drug trials. As we learned with COVID-19, the virus was first infectious and later a disease of excessive coagulation. These are radically different disease processes. Our system was not set up to adapt.
Second, it needs to replenish the Biomedical Advanced Research and Development Authority, which sits inside Health and Human Services and expand the oversight and data collection capacity to assure that political bias stays out of future funding decisions. A cross-section of scientists, even contrarian ones, but especially must include experienced physicians from the community without ties to the pharmaceutical industry — the conflicts of interest must stop. If this is accomplished, I believe we could devise a method to systematically test approved drugs alongside and with expensive new molecules.
With funding at the federal level, we can create a pathway for both individuals and groups of scientists to research new uses for old and new drugs and share their findings. This will lead to more inclusive processes for discovery of how off patent molecules can be applicable to today’s health challenges. And it will ensure that future discoveries are minimally influenced by money, special interests, and political meddling.
Kory is president and chief medical officer of the Front Line COVID-19 Critical Care Alliance.
Dr. Pierre Kory
Source link

:quality(70):focal(433x261:443x271)/cloudfront-us-east-1.images.arcpublishing.com/tronc/BMWRHYIIRRBEZOXWLO2SINKRC4.jpg)

:quality(70)/cloudfront-us-east-1.images.arcpublishing.com/tronc/QJKMNQ24J5DKXILN5QBO3FIK7I.jpg)