This article was originally published by Undark Magazine.
When Ina Chung, a Colorado mother, first fed packaged foods to her infant, she was careful to read the labels. Her daughter was allergic to peanuts, dairy, and eggs, so products containing those ingredients were out. So were foods with labels that said they “may contain” the allergens.
Chung felt like this last category suggested a clear risk that wasn’t worth taking. “I had heard that the ingredient labels were regulated. And so I thought that that included those statements,” Chung says. “Which was not true.”
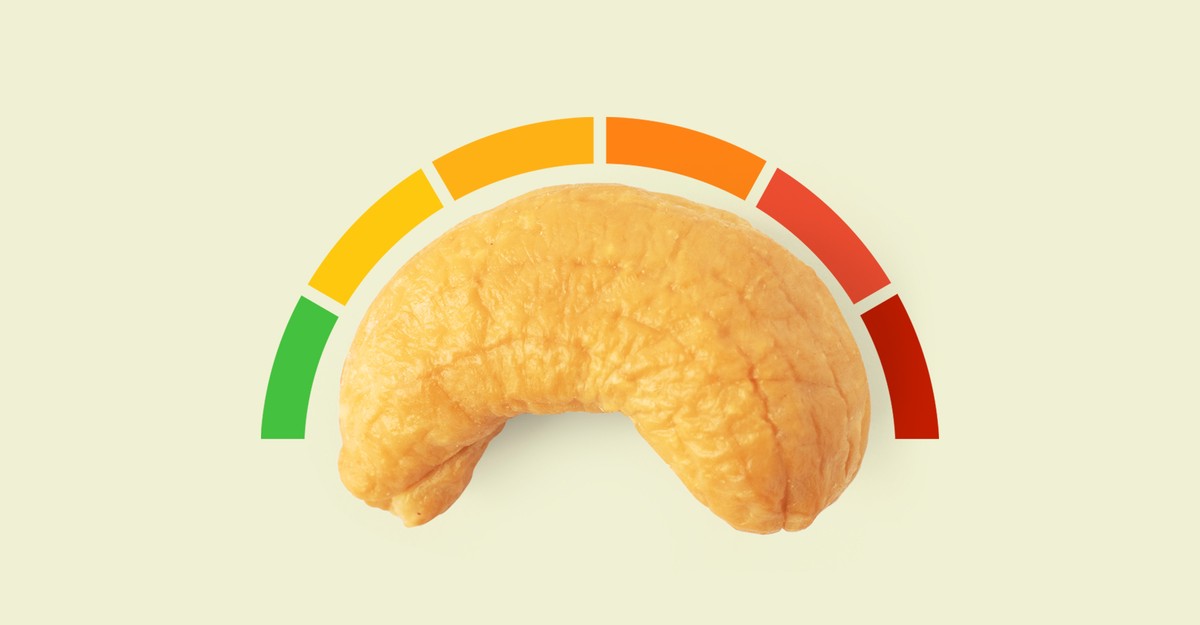
Precautionary allergen labels like those that say “Processed in a facility that uses milk or may contain fish” are meant to address the potential for cross-contact. For instance, a granola bar that doesn’t list peanuts as an ingredient could still say they may be included. And in the United States, these warnings are voluntary and not regulated; companies can use whatever precautionary phrasing they choose on any product. Some don’t use any labels, even in facilities where unintended allergens slip in; others list allergens that may pose little risk. Robert Earl, the vice president of regulatory affairs at the nonprofit Food Allergy Research & Education, or FARE, has even seen labels that include all nine common food allergens. “I would bet my bottom dollar not all of those allergens are even in the facility,” he says.
So what are the roughly 20 million people with food allergies in the U.S. supposed to do with these warnings? Should they eat that granola bar or not?
Recognizing this uncertainty, food-safety experts, allergy advocates, policy makers, and food producers are discussing how to demystify precautionary allergen labels. One widely considered solution is to restrict warnings to cases where visual or analytical tests demonstrate that there is enough allergen to actually trigger a reaction. Experts say the costs to the food industry are minimal, and some food producers across the globe, including in Canada, Australia, Thailand, and the United States, already voluntarily take this approach. But in the U.S., where there are no clear guidelines to follow, consumers are still left wondering what each individual precautionary allergen label even means.
Pull a packaged food off an American store shelf, and the ingredients label should say if the product intentionally contains one of nine recognized allergens. That’s because, in 2004, Congress granted the FDA the power to regulate labeling of eight major food allergens: eggs, fish, milk, crustaceans, peanuts, tree nuts, soybeans, and wheat. In 2021, sesame was added to the list.
But the language often gets murkier further down the label, where companies may include precautionary allergen labels, also called advisory statements, to address the fact that allergens can unintentionally wind up in foods at many stages of production. Perhaps wheat grows near a field of rye destined for bread, for instance, or peanuts get lodged in processing equipment that later pumps out chocolate-chip cookies. Candy manufacturers, in particular, struggle to keep milk out of dark chocolate.
Because the declarations are voluntary, the FDA offers no labeling guidance beyond saying that “advisory statements should not be used as a substitute for adhering to current good manufacturing practices and must be truthful and not misleading.”
Companies can choose when to use these warnings, which vary widely. For example, a 2017 survey conducted by the FDA and the Illinois Institute of Technology of 78 dark-chocolate products found that almost two-thirds contained an advisory statement for peanuts; of those, only four actually contained the allergen. Meanwhile, of 18 bars that carried no advisory statement for peanuts specifically, three contained the allergen. (One product that was positive for peanuts did warn more generally of nuts, but the researchers noted that this term is ambiguous.) Another product that tested positive included a nut warning on one lot but not on another. Individual companies also select their own precautionary-label phrasing.
For consumers, the inconsistency can be confusing, says Ruchi Gupta, a pediatrician and the director of the Center for Food Allergy & Asthma Research at Northwestern University’s Feinberg School of Medicine. In 2019, Gupta and her colleagues asked approximately 3,000 U.S. adults who have allergies, or care for someone who does, about how different precautionary-allergen-label phrases make a difference when they are considering whether to buy a particular food. About 85 percent said that they never purchase products with a “may contain” warning. Fewer than half reported avoiding products with labels suggesting that they were manufactured in a facility that also processes an allergen, even though some studies suggest that the wording of a precautionary allergen label does not always reflect the actual risk level. “People are making their own decisions on what sounds safe,” Gupta says.
When Chung learned that advisory labels are unregulated, she experimented with ignoring them when her then-toddler really wanted a particular food. When her daughter developed hives after eating a cereal labeled “May contain peanuts,” Chung went back to heeding warnings of peanut cross-contact but continued ignoring the rest.
“A lot of families just make up their own rules,” she says. “There’s no way to really know exactly what you’re getting.”
Most countries don’t regulate precautionary allergen labels, but many food-safety experts are exploring how they could. One popular tactic hinges on thresholds: the smallest amount of an allergen that could prompt an allergic reaction. If food producers abide by thresholds, the theory goes, they could restrict labels to products that contain allergens at or above this level.
Allergen sensitivities vary widely. To determine thresholds that would protect most people, researchers combine data from thousands of individual oral food challenges, in which an allergist presents a patient with increasing doses of an allergen until they have a reaction or have consumed a meal-size portion.
In 2022, an expert committee convened by the United Nations’ Food and Agriculture Organization (FAO) and the World Health Organization established thresholds for key allergens; the large majority of consumers with food allergies would not react at levels below these thresholds. The list initially included all allergens recognized in the U.S. except soy, and additionally broke tree nuts into specific examples—walnut, pecan, cashew, pistachio, almond, hazelnut. In 2023, the committee also established thresholds for additional allergens such as celery and soy.
That year, the committee also made recommendations on how policy makers could use the thresholds to regulate precautionary allergen labels. “It is critical that companies incorporate appropriate quality control, hygiene and risk mitigation practices into their overall allergen control programs,” Joseph Baumert, an FAO/WHO expert committee member, wrote in an email. Baumert is the director of the Food Allergy Research and Resource Program, an industry-funded consortium between the University of Nebraska at Lincoln and more than 100 member companies.
Companies, the recommendations suggest, should then be required to quantify the unintended allergens in products. This could include visual inspections for allergens such as whole sesame seeds, and using laboratory techniques to determine how much protein from an allergen is present. Taking into account how much of a food a person is likely to eat, the food producer should then determine whether an allergen’s concentration exceeds the recommended threshold-based limit; products with concentrations higher than this limit would have a label, whereas others would not. And all of the labels would need a single, standardized phrase.
A system like this “would be helpful for so, so many,” Chung says.
The FAO/WHO’s Codex Committee on Food Labelling, which helps set international food-labeling standards, may use the recommendations in developing its guidance on precautionary allergen labels. If adopted, many countries will follow the recommendations, predicts Marjan van Ravenhorst, who directs Allergenen Consultancy B.V. in the Netherlands.
But some companies already use thresholds for precautionary labels through the Voluntary Incidental Trace Allergen Labelling Program. Though VITAL was developed in Australia and New Zealand, companies headquartered in many countries, including the U.S., Canada, the United Kingdom, France, South Africa, and Thailand, have also subscribed, according to the food-safety specialist Jasmine Lacis-Lee, the president of the board of directors for Allergen Bureau, an industry-operated not-for-profit that runs the voluntary labeling program. In Switzerland, precautionary allergen labels are required when an allergen’s protein levels reach a concentration greater than 1,000 parts per million. Japan requires companies to list unintended allergens on the ingredients list itself whenever they are detected above an exceedingly low threshold.
Meanwhile, in the Netherlands, a mandatory threshold-based system will become fully enforced in 2026, and will require advisory labels when allergen concentrations surpass the thresholds recommended by the FAO/WHO committee. If there is no risk of an allergen, companies will not be able to use precautionary allergen labels.
A threshold-based approach should not have a major impact on the cost of food production, Lacis-Lee says. When it comes to implementing a VITAL risk assessment, she adds, “most businesses producing food should already be doing the vast majority of what is required.”
Exactly how often allergen testing is required under the threshold-based system depends on a facility’s risk level, says van Ravenhorst, who helped write the guidelines for the Netherlands’ new advisory-statement requirements: “If you only cut vegetables, and there is no allergen in your facility, it’s insane to test for different allergens every week.”
One concern about standardizing precautionary allergen labels is consumer comfort level. The FAO/WHO thresholds are designed to protect about 95 percent of an allergic population from an allergic reaction. Up to five percent could still react to allergens at levels so low that they fall under the threshold, at which point using a precautionary label would be against the rules. Of these individuals, some could experience mild to moderate anaphylaxis, but there are no confirmed reports of fatal anaphylaxis from allergens at or below the thresholds, according to the 2023 FAO/WHO report.
The report suggests that this system would improve safety for allergic consumers. Currently, unintended allergens can exist at higher levels without warning; with the proposed system, foods with allergens above the threshold would all carry a label.
Not offering a precautionary label when you know that an allergen is there, even at very low levels, can feel difficult, says van Ravenhorst, who herself has several allergies. But she feels that there’s a balance between overuse of labeling and protection: “We want to be informed when there is a real risk.”
Gupta’s team recently surveyed U.S. allergists for their thoughts on precautionary allergen labels, including whether thresholds should be used; a similar survey for people with allergies is in the works. Gupta wonders whether consumers might prefer a system in which each food label states whether allergens are entirely absent, present above a threshold, or present below a threshold. But she’s already concerned that this alternative would most benefit those who know their sensitivity levels from allergist visits, which may leave out many patients. Her research shows that low-income caregivers of children with allergies spend less on specialist appointments. She worries: “Will it cause a bigger divide?”
Some U.S. companies would likely welcome more guidance on advisory labeling, Baumert said. In keeping with the Food Safety Modernization Act, most already have allergen-control plans, which include monitoring for unintended allergens. Most food companies, for example, do some analytical work to confirm that their cleaning procedures are effective—for instance, when they switch from a recipe that contains an allergen to one that doesn’t.
But according to some companies, the current guidelines make it difficult to respond when producers are unable to eliminate traces of unintended allergens. Looking for a way out of a regulatory gray zone, some even opt to include allergens in recipes so that they can follow clearer guidelines. After Congress declared sesame a major food allergen in 2021, for example, the seed became a listed ingredient in many foods that people with sesame allergies previously enjoyed.
“This addition of sesame would likely not be needed if FDA would establish allergen thresholds or otherwise set forth clear guidance as to when advisory or precautionary labeling (i.e. “may contain” statements) may be used,” Eric Dell, the president and CEO of the American Bakers Association, wrote in a May 2023 letter to select congressional members.
When it comes to precautionary allergen labels, “we recognize that the extensive use of these statements may be confusing to consumers, and we are considering conducting some consumer research in this area,” an FDA spokesperson, Enrico Dinges, wrote in an email.
In January 2024, the FDA published draft guidance for the industry; in it, the agency acknowledged that there may be situations where food producers, even after following good allergen-management practices, cannot assure consumers that food is safe, and therefore should include labeling “that discloses the possible unintended allergen presence in the food.”
But the agency stopped short of universal recommendations on exactly how to determine whether an unintended allergen presents enough risk to warrant an advisory statement. There’s a need for clarity on the FDA’s expectations for precautionary allergen labels, Baumert said: “I think we’ve gotten further on an international basis than we have currently here in the U.S.”
Meanwhile, American families are left to interpret allergen-advisory labels alone. Chung’s daughter is now 6 years old, and the family no longer follows precautionary peanut labels. The change came after Chung learned of a 2021 review paper suggesting that half of people with peanut allergies can eat about half a peanut without reacting. Based on her daughter’s reaction history, Chung felt that her then-5-year-old could likely handle trace amounts too, because a severe allergic response seemed unlikely. So Chung took a chance and let her try a granola bar that her brother loved, despite the fact that the wrapper suggested it might contain peanuts. The response: no reaction. She really wanted it, Chung says, who recalls thinking: “If it’s safe, how wonderful would that be?”
Carolyn Beans
Source link