Dairy products such as milk, yogurt, cheese and cream—any foods made from the milk of other mammals—are a versatile and beloved staple food of the American diet. Dairy products were not part of the human diet until about 10,000 years ago, when livestock were first domesticated. We are told that these foods are essential to a healthy diet, yet for nearly two million years humans and pre-humans thrived on little to no dairy foods at all. We are told that the high levels of calcium in milk are important for the formation of strong bones and healthy teeth. Dairy products are also an inexpensive source of high quality protein. How could a food that our ancestors lived without for so long be considered essential to our health today? Were we designed to require the milk of another species for our own growth and development? Or have we outsmarted Mother Nature and found a way to be healthier than our ancestors by adding dairy to our diets?
Many people have trouble processing dairy foods, and most don’t even realize it. Since most of us in the West have been consuming dairy products every single day since we were very young, we may not make the connection between troublesome symptoms and dairy foods. Some of the most common problems that can be caused by dairy include digestive disorders, asthma, upper respiratory tract infections, muscle and joint pains, urinary tract irritation, migraine, acne and eczema.
When we talk about milk, we are usually referring to cow’s milk. Cow’s milk is a complicated and highly specialized food designed to nourish and grow a baby cow. Therefore, it contains all kinds of interesting things—basic nutritional building blocks like proteins, fats, and carbohydrates, as well as minerals, vitamins, antibodies, growth factors, and other substances to stimulate the development of the little cow. The quality and amount of each of these components varies greatly, depending on the type of cow, how she is raised, and what she is fed. Let’s break milk down into its many parts to see what we are actually getting.
INGREDIENTS:
- Milk sugar
- Milk proteins
- Milk fat
- Minerals
- Hormones
Milk sugar: lactose and lactose intolerance
What is lactose?
Lactose is the type of sugar found in all kinds of mammal milk—from human breast milk to cows’ milk to camels’ milk—the lactose is exactly the same. Each lactose molecule is made of two individual sugar molecules—one glucose molecule linked to one galactose molecule. We can absorb glucose and galactose easily, but we can’t absorb them when they are linked together as lactose. So, when we are babies, and dependent on mother’s milk, we have a special enzyme in our intestines called lactase, which breaks the link and frees up the glucose and galactose, so that we can absorb them. Lactase is like a little pair of chemical scissors that cuts the lactose in half.
What is lactose intolerance?
If you ask me, lactose intolerance is not a medical problem; it’s simply a sign that you’ve grown up.
Between the ages of two and five, most humans lose most or all of their ability to produce lactase, so most of us are lactose intolerant to some degree. Before agriculture was born (at most 10,000 years ago), humans did not have the ability to digest milk in early childhood, after weaning from breast milk. So, all of our hunter-gatherer ancestors were lactose intolerant. However, once people started eating dairy products regularly, a genetic shift occurred that allowed some people to keep the ability to digest milk into their adult years. These people are called “lactase persistent.” They essentially evolved the ability to tolerate lactose.
However, most of us still lose that ability, so by the time we are in grade school, we lack enough of the lactase enzyme to properly digest lactose. Without lactase, the lactose can’t be broken down and absorbed, so it continues on down the gastrointestinal tract, until it eventually encounters intestinal bacteria, who very much enjoy dining upon it. Unfortunately, they don’t break it into glucose and galactose for us. Instead, bacteria ferment the lactose, releasing lactic acid and gases in the process. Not only will these gases make you unpopular at parties, but they can cause you significant bloating, pain, and/or diarrhea, as well.
How common is lactose intolerance?
Approximately two-thirds to three-quarters of the world’s population is lactose intolerant, with the prevalence varying depending on ethnic background. Rates in Asia approach 100%. It is hard to know exactly how many Americans are lactose intolerant, but estimates suggest that approximately 15% of Caucasian Americans, 53% of Hispanic Americans, and 80% of African Americans may have lactose intolerance.
Studies show that lactose intolerance may be a matter of degree for some people. If you are 100% lactose intolerant, you don’t make any lactase at all, while “lactose tolerant” people make enough lactase to digest about 92% of all the lactose they eat. But there are some people in the middle, who make a small amount of lactase. These people can get away with eating small amounts of dairy foods, but if they eat too much, they won’t have enough lactase to digest it, so they will get symptoms of lactose intolerance. Everyone’s tolerance is different. Even most people who test positive for lactose intolerance can get away with drinking up to a cup of milk per day without any significant symptoms.
How do I know if I am lactose intolerant?
If dairy products bother you, you can ask your doctor for a lactose intolerance test. If you are lactose intolerant, the lactose you eat will make it all the way down to your colon, where the bacteria ferment it and create hydrogen gas. This gas passes into your bloodstream, then into your lungs, and comes out in your breath. In the lactose tolerance test, you will be given some lactose, and then your breath will be tested for hydrogen gas. If you breathe out hydrogen gas after eating lactose, you are lactose intolerant. If dairy products bother you and your test result is negative, then you don’t have lactose intolerance, but instead you may have trouble with other ingredients in dairy products, most likely milk protein (see below).
If I’m lactose intolerant, do I have to give up all dairy products?
As far as we know, lactose intolerance is not dangerous to your health. If you have lactose intolerance, there may still be ways for you to comfortably enjoy dairy products. There are many dairy products which contain little to no lactose. These include heavy cream (not half-and-half), sour cream, most hard cheeses (the bacteria used to age cheeses eat all the lactose), butter, and ghee (clarified butter).
Read the product label; since all of the carbohydrates in dairy products are lactose, the higher the carbohydrate gram count, the higher the lactose content. If the carbohydrate content is zero grams, then the product is virtually lactose-free. If you wish to eat foods that contain lactose, you may want to try an over-the-counter lactase product like Lact-Aid®, to help you digest lactose. Lactose-reduced milks are available, as well. Consuming dairy products with meals can also help to reduce the risk of uncomfortable symptoms.
Milk protein: casein and whey
Remember Little Miss Muffett—the chick who sat on her tuffett, eating her curds and whey?
Well, she must have let her milk sit out too long and curdle. If you let milk curdle, what you get are curds (like the lumps in cottage cheese) and whey (the watery stuff that floats to the top). These are the two main protein groups in milk—the curds are made of casein proteins and the whey contains whey proteins.
Caseins
The casein portion of milk is protein-rich and contains most of milk’s calcium. Caseins are very sticky and clump together (casein has historically been used as the active ingredient in wood glue). Caseins are actually designed by nature to form a clot in the stomach. Why in the world would a newborn want a lump of protein in its stomach? It’s ingenious, really—if the proteins don’t stick together, they get rapidly digested and absorbed. Digestive enzymes take longer to chew their way into the middle of a clump, so casein is essentially an extended-release source of protein that is gradually broken down over a number of hours, rather than all at once.
Caseins are very difficult to digest compared to wheys, and cow’s milk contains a LOT more casein than human breast milk. Cow’s milk contains 3 to 4 times as much protein per cup compared to human breast milk because—hello—it’s designed to grow a baby cow, which is SO much bigger than a baby human and grows a LOT faster. A newborn calf can weigh between 40 and 100 pounds, depending on the breed, and gains about 1-1/2 pounds per day, so it needs a LOT more protein. Also, the ratio of caseins to wheys is very different in cow’s milk vs. human milk:
- Cow’s milk protein ratio: 80% caseins and 20% wheys
- Human milk protein ratio: 40% caseins and 60% wheys*
* Milk composition varies depending on stage of breastfeeding; whey protein is very high in early stages (about 80% whey + 20% casein) and lower in later stages (about 50% whey + 50% casein).
So, cow’s milk contains approximately 6 times more casein per cup than human breast milk does. How does the baby cow handle all of that sticky casein?
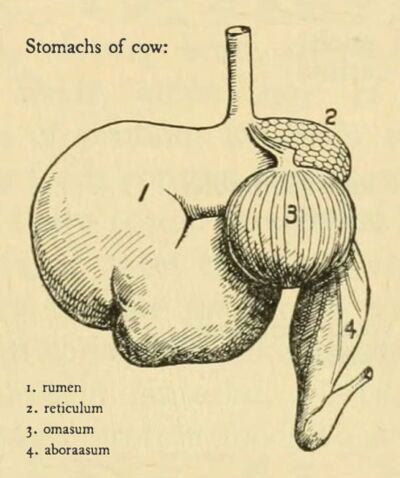
Well, first of all, a baby cow has a completely different digestive system than a baby human does. Not only does a baby cow have FOUR stomachs, the baby cow also has a special enzyme in one of its stomachs called “rennet.” This enzyme is designed to digest the large amount of casein in their mother’s milk. Rennet breaks up the casein clumps into digestible particles. Human babies do not have rennet.
Are cow’s caseins and human caseins different?
There are lots of differences between cow’s caseins and human caseins, but the biggest difference is that the major type of casein found in human breast milk is beta casein, and the major type found in cow’s milk is alpha S1 casein. Alpha S1 casein from cow’s milk is the most common cause of milk protein allergies. All types of mammal milk, including cow’s milk and human milk, also contain another type of casein called kappa casein, but kappa casein comes in two very different forms—a “ruminant” form (for animals with more than one stomach, like cows) and a “non-ruminant” form (for animals with only one stomach, like humans).
It is likely that these major differences between the types of proteins in cow’s milk vs. human milk, and the absence of rennet in the human digestive tract are largely responsible for the significant gastrointestinal distress that can occur in people who are sensitive to cow’s milk products.
Whey proteins
Compared to caseins, whey proteins are softer, finer, much more easily digestible proteins. These proteins include lactoferrin, albumin, and lactalbumin. The whey portion also holds most of the milk’s lactose, as well as the IgA antibodies necessary to pass immune protection from mother to baby.
Human whey proteins are also different from cow’s whey proteins. The primary whey proteins in human milk are lactoferrin, albumin, and lactalbumin, whereas the dominant whey protein in cow’s milk is lactoglobulin.
Milk protein allergy and sensitivity
True allergy symptoms
Many people who have trouble with dairy products do not have lactose intolerance; instead they have trouble with milk proteins. People with serious, true milk allergies are reacting to the proteins in the milk, not the lactose. A true (IgE-mediated) allergy will cause hives, swelling, flushing, rash, oral allergy syndrome (itching/burning in mouth/throat), and/or wheezing within two hours, and may require emergency treatment with epinephrine (EpiPen®) to avoid life-threatening anaphylactic shock. This is why people with true allergies should strictly avoid all dairy products.
How common is true milk allergy?
Cow’s milk protein allergy is the most common allergy in children, affecting 2 to 5% of children under the age of three. Symptoms usually appear within two months or less of feeding cow’s milk to a baby for the first time. The most common symptom of milk allergy in infants and young children is constipation. Other clues include: eczema, asthma, rhinitis (swollen/itchy nose and eyes), reflux, vomiting, and rectal bleeding. Ten percent of colic cases are due to cow’s milk protein allergy. Interestingly, if the nursing mother is consuming dairy products herself, her baby can develop an allergy to cow’s milk proteins through breastfeeding, but the risk is much lower (about 0.5%). In these uncommon cases, the mother is advised to remove dairy products from her own diet if she wishes to continue nursing her baby.
Which milk proteins cause allergy?
Any of the various proteins in milk can cause an allergy. The potentially problematic proteins in milk include casein (4 different kinds), whey, lactalbumin and lactoglobulin. Allergy to caseins is more common than allergy to whey proteins. One type of casein—alpha-S1 casein— is the most common culprit in true milk protein allergy sufferers.
If I’m allergic to cow’s milk, can I have sheep’s or goat’s milk instead?
Unfortunately, virtually 100% of those with a true cow’s milk allergy will also be allergic to sheep’s and goat’s milk, as well. Luckily, special formulas are available for babies who are allergic to cow’s milk. Eighty percent of milk-allergic children outgrow their true milk allergy by the age of 5. However, many of these children continue to have gastrointestinal issues related to milk products many years later. [Note: those with milk protein allergy have about a 10% chance of also being allergic to soy protein, and about a 10% chance of being allergic to a protein in milk and undercooked beef called bovine serum albumin.]
How can I know whether I am truly allergic or just sensitive?
Luckily, there are several kinds of tests available for true milk allergy, but there are no reliable tests available for milk protein sensitivity, which may be even more common than true milk protein allergy. Dairy sensitivity is the cause of colic in some infants, and is a common cause of recurrent ear infections, sinus congestion, and reflux/swallowing problems in infants and young children. Like all food sensitivities, the only way to know if you or your child has milk protein sensitivity is to eliminate all dairy products from the diet for two to four weeks to see if symptoms improve.
If I have milk protein sensitivity, do I have to avoid all dairy products?
In contrast to true allergies, sensitivities are not life-threatening, so you get to decide whether you continue to eat dairy proteins, how much, and how often. However, sensitivities can cause significant discomfort and even temporary disability in some people. If you discover that you have milk protein sensitivity, you may be able to tolerate low-protein dairy products.
There are a few dairy products which are extremely low in proteins, such as heavy cream (not half-and-half), butter, and sour cream. Read the label; if the product contains zero grams of protein, it may not bother you. Keep in mind that zero grams doesn’t mean that it’s guaranteed to be completely protein-free; there are often tiny amounts of proteins in these items. For example, butter is listed as having zero grams of protein, but there is enough protein in it to bother some people. If butter bothers you, you may want to try ghee, which is clarified butter, and is virtually protein-free.
Milk fats
Saturated fat
Approximately 2/3 of the fat in whole milk is saturated fat; the rest of it is monounsaturated and polyunsaturated fat.
The saturated fat in milk fat is called butterfat, and is one of the most complicated mixtures of fats found in nature. The types and relative amounts of fats in milk depend heavily on what the cow is eating, but the predominant fatty acids in butterfat are usually: oleic acid, palmitic acid, and myristic acid.
Omega-3 fatty acids
The amount of omega-3 polyunsaturated fatty acids in milk varies greatly, and depends on what the cow is fed. There are three omega-3 fatty acids: ALA, EPA, and DHA (see my fats page). Cow’s milk contains varying amounts of ALA, depending on what they eat. Grass-fed cows give milk that is higher in ALA.
Cow’s milk does not contain the other two omega-3 fatty acids, EPA or DHA. Human breast milk does contain DHA, with the amount varying greatly depending on the mother’s own diet. Women eating traditional whole foods diets have much higher levels of DHA in their breast milk than women who eat a typical Western diet.
Trans fat
You may be aware that trans fats are considered generally very unhealthy, particularly for the heart. However, the health risks associated with trans fats were connected to the trans fats found in industrially-produced hydrogenated vegetable oils. What many people don’t know is that there is a natural source of trans fats in the world: ruminant animals (animals with more than one stomach). Bacteria in the cow’s digestive tract turn unsaturated fatty acids, such as linoleic acid and alpha-linolenic acid, into trans fatty acids. These can then be absorbed by the cow, and incorporated into the cow’s milk and meat.
There are two naturally-occurring trans fatty acids in cow’s milk: conjugated linoleic acid (CLA) and vaccenic acid (VA). About 2 to 5% of the fat in dairy products consists of these natural trans fats. One cup of standard whole milk contains about 0.2 grams of trans fat. Note: pastured/grass-fed milk contains about twice as much CLA as grain-fed milk does.
Are the natural trans fats in dairy products unhealthy?
Ironically, the reason why there has been so much interest in these fats, particularly CLA, is because there have been numerous studies suggesting that CLA may have health benefits, namely anti-cancer properties in laboratory animals. There have been no human studies that have clarified this relationship, so we currently do not know if CLA has anti-cancer properties in people.
Because industrial trans fats were determined to be associated strongly with heart disease risk, it makes sense to wonder whether dairy trans fats such as CLA may be bad for the heart. So far, the studies have been very mixed, and there is no conclusion yet one way or the other.
Luckily, the amount of CLA that people take in from dairy products is quite small, so it may not matter whether it is good or bad for us. There are too few studies of VA to understand how it affects us. Not only that, even though we humans can’t make trans fatty acids from scratch, we are capable of converting some of the VA we eat to CLA, so whatever effects VA might have on us might be partly due to CLA. It’s complicated.
Milk and bone health
 Cow’s milk contains about one gram of calcium per liter, about four times as much as human breast milk. There is nothing special about the calcium in milk; it is just as easily absorbed as other forms of calcium from other sources. People eating a typical Western diet absorb only about 40% of the calcium they consume.
Cow’s milk contains about one gram of calcium per liter, about four times as much as human breast milk. There is nothing special about the calcium in milk; it is just as easily absorbed as other forms of calcium from other sources. People eating a typical Western diet absorb only about 40% of the calcium they consume.
We are taught that milk is essential for the growth and health of children, especially for nurturing strong bones, because it is such a good source of calcium. Yet, despite the fact that Americans eat more dairy products than people in most other countries, we still have a much higher rate of osteoporosis than many other countries. Osteoporosis seems to follow a similar worldwide pattern to many other “diseases of Western civilization.”
We are not yet entirely sure what it is about the Western diet or lifestyle that is responsible for increased risk for osteoporosis in Western countries such as the U.S., but it is important to keep in mind that the presence or absence of dairy products is only one potential puzzle piece.
We are not generally asked to consider the other elements of our diet that affect bone strength. Some of these other considerations include:
- Vitamin D, which is critical to our ability to use calcium to build bone (Unfortified milk is not a significant source of Vitamin D. Most milk in the US has been fortified with Vitamin D since 1933.)
- Access to high quality protein sources for bone growth
- Plant food anti-nutrients, such as phytic acid and oxalates, which interfere with calcium absorption
- Refined carbohydrates (there they are again . . .), which raise cortisol levels, setting the stage for bone loss
Milk hormones
How does cow’s milk grow a cow, and why should you care?
Job number one of all mammal milks is to make baby mammals grow. To grow, you need proteins, fats, and carbohydrates to build body parts, and milk has all of those ingredients. However, just pouring ingredients into an animal doesn’t cause growth unless the hormonal conditions are just right. Think about it this way: you can pour all the food you want into a 45-year-old woman but she will NOT get any taller.
How does the body know what to do with all the nutrients you are pouring into it? Should the nutrients be stored for later use? Burned for energy? Or turned into new cells? What types of cells? Bone? Muscle? Liver? All of these decisions are made by hormones.
So, Mother Nature not only gave milk all the ingredients needed for growth, she also included the directions about how to grow, when to grow, and what parts should grow. These directions come in the form of hormones called growth factors. As we digest the caseins and whey proteins in cow’s milk, they are broken down into growth factors that send signals to our body.
Please note that I am not referring here to added bovine growth hormone (added BGH). I am referring to the naturally occurring hormones in cow’s milk that are supposed to be there for the sake of the baby cow. This is why no milk can ever be labeled “free of growth hormone”—all cow’s milk, even from the healthiest, most humanely-treated, organically-raised, grass-fed cow, contains growth hormones.
Does cow’s milk affect human hormones?
Whey proteins in milk cause our insulin levels to rise. In fact, milk (which has a low glycemic index and therefore doesn’t cause our blood sugar to spike) causes our insulin levels to rise in a similar fashion to refined carbohydrates. I know that most of us think of insulin simply as the hormone that keeps our blood sugar in check, but this is really not its primary purpose. Insulin is the mother of all growth hormones; it is intimately involved with all aspects of growth (see my carbohydrates page).
Whey proteins in milk also signal our body’s growth hormone (or GH; also known as somatotropin) levels to rise. GH is critical for growing taller.
Casein proteins in milk tell our body’s IGF-1 (Insulin-like Growth Factor-1) levels to rise by as much as 30%. Cow’s milk also contains some IGF-1, which is identical to human IGF-1, but we are not sure if cow IGF-1 is absorbed by people.
GH and IGF-1 work together to grow longer bones and larger organs. They tell cells to multiply. Humans produce this same combination of hormones during puberty, which is why teenagers go through a dramatic growth spurt.
Cow’s milk also contains the pre-hormone 5-alpha-pregnanedione, which can be converted into dihydrotestosterone.
Does cow’s milk make children grow more or mature faster?

All of these special signaling hormones in milk are designed to make a baby cow grow bigger, so it makes perfect sense that cow’s milk might also contribute to the growth of children. Let’s see what the research says.
A number of epidemiological studies find an association between how much milk pregnant women drink and how much their babies weigh at time of delivery, but again, it is hard to be certain that milk itself was the only reason for higher birth weights. IGF-1 in mother’s blood, whether it is her own IGF-1 or whether she absorbed it from cow’s milk, cannot cross the placenta. However, IGF-1 may have effects on the placenta itself, which can in turn affect how babies grow.
A number of epidemiological studies have found that children between 2 and 5 years old who drink more milk tend to be taller. Studies of older children and teenagers are not as well-designed overall, and the results are very mixed. We do know that it is probably not the calcium in the milk that is making children grow faster or taller, because intervention studies (better able to show cause and effect) do not find any connection between how much calcium children get and how much they grow.
Studies to date do not find any association between milk intake and age of menarche (first menses) in girls.
Some may view the growth-promoting properties of cow’s milk as a benefit, helping children to grow tall. I’m not aware of any direct experimental evidence that helps us understand whether milk indeed makes children grow taller, but if it were true, would that be a good thing? We know we are supposed to drink human breast milk early in life, and that human breast milk is designed especially for our growth needs. The problem is that we are only supposed to be receiving this special growth-promoting drink when we are babies and need to grow a LOT, very quickly. Should we be drinking cow growth formula every day of our lives? What might you logically expect to happen if your body is being forced into growth mode all the time, when it shouldn’t be? Is there such a thing as bad growth?
Dairy products and cancer risk
Well, sure—cancer is, hands down, the scariest form of growth, and IGF-1 in particular is famous not only for promoting the growth of normal cells; it is also infamous for promoting the growth of cancer cells.
Some epidemiological studies in adults show an association between dairy products and increased risk for prostate cancer, while other epidemiological studies suggest that milk may reduce the risk for colon and bladder cancer in adults. Remember that epidemiological studies cannot speak to cause and effect relationships between foods and diseases, and therefore cannot show that drinking more milk may be the reason for any of these confusing associations. Cancer is a very complicated disease, and dairy products are very complicated foods. It is nearly impossible to tease out any real connection between these two things in epidemiological studies.
Therefore, it is not surprising that two very recent reviews of all pertinent studies of dairy products and cancer risk both concluded that there is not enough evidence to say whether dairy products increase or decrease the risk of various types of cancer.
Dairy products and body weight
Since milk stimulates insulin spikes, it would make sense to wonder whether milk increases our risk of obesity and the many other health problems associated with hyperinsulinemia (high insulin levels). (See my carbohydrates page.)
You may have heard commercials claiming that people who eat dairy products tend to weigh less. Unfortunately, it seems not to be true:
“Of 49 randomized trials assessing the effect of dairy products or calcium supplementation on body weight, 41 showed no effect, two demonstrated weight gain, one showed a lower rate of gain, and five showed weight loss . . . Consequently, the majority of the current evidence from clinical trials does not support the hypothesis that calcium or dairy consumption aids in weight or fat loss.” [Lanou and Bernard 2008]
Miscellaneous bioactive peptides in milk
Proteins in cow’s milk and human milk break down during digestion into smaller pieces called “peptides,” some of which have special biological functions.
Peptides with opioid (narcotic) properties
Some milk peptides have natural opioid properties; opioids you may be familiar with include narcotic medications such as morphine and codeine.
So, do milk opioids act like narcotics in our bodies? The natural opioids present in milk are apparently very weak, and may only have effects on the lining of the digestive tract, since it is unclear if they can be absorbed into the bloodstream, let alone cross the blood-brain barrier and make it into the brain. As you may know, opioids act to slow down the activity of the gastrointestinal tract (which is why narcotics tend to cause constipation), so it is possible that some sensitive people may experience this as a side effect of milk products. Some people point to the fact that there are opioid peptides in milk to support the notion that dairy products are addictive and sedating; however, there are no human studies I’m aware of at this time (2012) to help us understand the role that these opioids play in our bodies.
Do dairy products cause acne?
Acne is a disease of Western civilization, in that it is not found in peoples who eat traditional whole foods diets. This pattern strongly suggests a dietary cause.
In the past five years, researchers have begun conducting studies that are shedding light on the diet-acne connection. Two main dietary suspects are emerging from these early studies: dairy products and refined carbohydrates.
The whey portion of milk contains a growth factor called betacellulin. This growth factor binds to something called the epidermal growth factor receptor (EGFR), which stimulates the pilosebaceous unit (the follicle) to overproduce sebum (mixture of natural skin oils and skin cells), which can lead to acne lesions.
The whey portion of milk stimulates insulin and IGF-1 production, and these in turn can stimulate acne formation. High glycemic index and refined carbohydrates also stimulate insulin secretion.
Interestingly, low-fat dairy products contain much more whey protein than full-fat dairy products, so low-fat dairy products are more powerful triggers of risky insulin spikes than full-fat dairy products. The less fat a dairy product contains, the more whey protein it tends to contain. Therefore, non-fat dairy products contain the highest percentage of whey proteins. Since non-fat dairy products and refined carbohydrates both trigger insulin spikes, the worst case scenario would then be a non-fat yogurt with added sugar, or a sweetened skim milk product (such as non-fat chocolate milk). Some people believe that chocolate cause acne breakouts. Plain milk chocolate has not been properly studied yet, but it would make sense that this food, which contains both milk proteins and sugar, might contribute to acne.
We still need more studies to clarify these connections. While there have been a number of human clinical studies, we need larger, randomized, properly-controlled clinical trials that look specifically at these suspects. For more information, please see my post “The Secret to Outsmarting Your Acne.”
Does milk cause iron-deficiency anemia?
In babies less than 12 months old, cow’s milk increases the risk of iron deficiency. There are several theories about why this is. One theory is that the proteins in cow’s milk interfere with the absorption of iron from the baby’s intestines. Another theory is that, in about 40% of babies, cow’s milk causes microscopic bleeding from the baby’s digestive tract, and since blood contains iron, the baby loses a little bit of iron every day. This is one of the reasons why parents in the U.S. are advised not to feed cow’s milk to babies under one year of age.
Does milk increase mucus production in the sinuses, throat, or lungs?
Many people believe this to be true (this is why choral directors and voice coaches often advise singers to avoid dairy products prior to performances), but there have been no studies yet that can confirm or deny this belief. If you suspect this is true for you, remove dairy products from your diet for two weeks to see it makes a difference.
Bottom line about dairy products
- Milk is not necessary for human life or health, and is therefore optional, unless you don’t have reliable access to other complete sources of protein and essential nutrients such as meat, seafood, poultry or eggs.
- Babies under one year of age should not drink milk (unless other nutritious options are not available) because it increases their risk for iron-deficiency anemia.
- Many people suffer from dairy intolerance, particularly people of Asian, African and Latin American ancestry.
My opinion about dairy products
There is plenty of strong evidence that dairy products can cause health problems and no good evidence that dairy products are essential to health (unless other nutritious foods are not available).
As with most foods, if you enjoy them, and they don’t seem to bother you, then you may choose to include them in your diet. However, the only way to know if they bother you is to remove them from your diet for several weeks (I would recommend one month) and see how you feel without them. If you choose to eat them, just be aware of the potential risks involved.
Since the most troublesome ingredients in dairy products are 1) milk proteins and 2) lactose, I would recommend choosing full-fat dairy products, since these are lower in proteins and lactose than low-fat versions, are more satisfying (therefore you may eat less of them), and they taste better to many people.
References
Agostoni C, Turck D. Is cow’s milk harmful to a child’s health? J Pediatr Gastroenterol Nutr. 2011;53(6):594–600.
Bartley J, McGlashan SR. Does milk increase mucus production? Med Hypotheses. 2010;74(4):732–734.
Benhamou A, Schäppi Tempia MG, Belli DC, Eigenmann PA. An overview of cow’s milk allergy in children. Swiss Med Wkly. 2009;139(21-22):300-307.
Bischoff-Ferrari HA, Dawson-Hughes B, Baron JA et al. Calcium intake and hip fracture risk in men and women: a meta-analysis of prospective cohort studies and randomized controlled trials. Am J Clin Nutr. 2007;86(6):1780–1790.
Bischoff-Ferrari HA, Dawson-Hughes B, Baron JA, et al. Milk intake and risk of hip fracture in men and women: a meta-analysis of prospective cohort studies. J Bone Miner Res. 2011;26(4):833–839.
Chagas CEA, Rogero MM, Martini LA. Evaluating the links between intake of milk/dairy products and cancer. Nutr Rev. 2012;70(5):294-300.
DeGreef E, Salvatore S, D’Auria E, et al. Diagnosis and management of cow’s milk protein allergy in infants. World J Pediatr. 2012;8(1):19-24.
El-Hodhod M, Younis NT, Zaitoun YA, Daoud SD. Cow’s milk allergy related pediatric constipation: appropriate time of milk tolerance. Pediatr Allergy Immunol 2010(2 pt 2);21:e407–e412.
Erbersdobler HF, Trautwein E, Greulich HG. Determinations of taurine in milk and infant formula diets. Eur J Pediatr. 1984;142(2):133-144.
European Food Safety Authority Review of the potential health impact of β-casomorphins and related peptides. EFSA Scientific Report. EFSA Journal. 2009;231:1-107.
Feskanich D, Willett WC, Stampfer MJ, Colditz GA. Milk, dietary calcium, and bone fractures in women: a 12-year prospective study. Am J Public Health. 1997;87(6):992-997.
Gebauer SK, Chardigny JM, Jakobsen MU, et al. Effects of ruminant trans fatty acids on cardiovascular disease and cancer: a comprehensive review of epidemiological, clinical, and mechanistic studies. Adv Nutr. 2011;2(4):332-354.
Ginger M, Grigor M. Comparative aspects of milk caseins. Comp Biochem Physiol B Biochem Mol Biol. 1999;124(2):133-145.
Gueguen L, Pointillart A. The bioavailability of dietary calcium. J Am Coll Nutr. 2000;19(2):119S-136S.
Haug A, Høstmark AT, Harstad OM. Bovine milk in human nutrition—a review. Lipids Health Dis. 2007;6:25.
Hochwallner H, Schulmeister U, Swoboda I, et al. Patients suffering from non-IgE-mediated cow’s milk protein intolerance cannot be diagnosed based on IgG subclass or IgA responses to milk allergens. Allergy. 2011;66:1201-1207.
Lampe J. Dairy products and cancer. J Am Coll Nutr. 2011;30(5):464S-470S.
Lanou AJ, Bernard ND. Dairy and weight loss hypothesis: an evaluation of the clinical trials. Nutr Rev. 2008;66(5):272-279.
Lanou AJ, Berkow SE, Barnard ND. Calcium, dairy products, and bone health in children and young adults: a reevaluation of the evidence. Pediatrics. 2005;115(3):736-743.
Law D, Conklin J, Pimentel M. Lactose intolerance and the role of the lactose breath test. Am J Gastroenterol. 2010;105(8):1726-1728.
Leerbeck E, Sundergaard H. The total content of vitamin D in human milk and cow’s milk. Br J Nutr 1980;44(1):7-12.
Martin MA, Lassek W, Gaulin S, et al. Fatty acid composition in the mature milk of Bolivian forager-horticulturalists: controlled comparisons with a US sample. Matern Child Nutr. 2012;8(3):404-418.
Melnik B. Evidence for acne-promoting effects of milk and other insulinotropic dairy products. Nestle Nutr Inst Workshop Ser Pediatr Program. 2011;67:131-145.
Nagpal R, Behare P, Rana R, et al. Bioactive peptides derived from milk proteins and their health beneficial potentials: an update. Food Funct. 2011;2(1)2:18.
Paddack A, Gibbons T, Smith C, Patil S, Richter GT. Food hypersensitivity and otolaryngologic conditions in young children. Otolaryngol Head Neck Surg. 2012;147(2):215-220.
Qin L-Q, He K, Xu JY. Milk consumption and circulating insulin-like growth factor-1 level: a systematic literature review. Int J Food Sci Nutr. 2009;60(S7):330-340.
Rudloff S and Kunz C. Protein and nonprotein nitrogen components in human milk, bovine milk, and infant formula: quantitative and qualitative aspects in infant nutrition. J Pediatr Gastroenterol Nutr. 1997;24(3):328-334.
Spencer EH, Ferdowsian HR, Barnard ND. Diet and acne: a review of the evidence. Int J Dermatol. 2009;48(4):339-347.
Suchy FJ, Brannon PM, Carpenter TO, et al. National Institutes of Health consensus development conference: lactose intolerance and health. Ann Intern Med. 2010;152(12):792-796.
Wiley A. Cow milk consumption, Insulin-like growth factor-I, and human biology: a life history approach. Am J Hum Biol. 2012;24(2):130-138.